Understanding fertility often starts with one of the simplest yet most misunderstood tests — the semen analysis. For many couples in the IVF and fertility journey, these early diagnostics play a key role in clarifying the next steps toward conception. But semen analysis is more than just a number on a chart; it reflects timing, consistency, and actionable data that can shape your treatment plan in NYC or anywhere you seek fertility care.
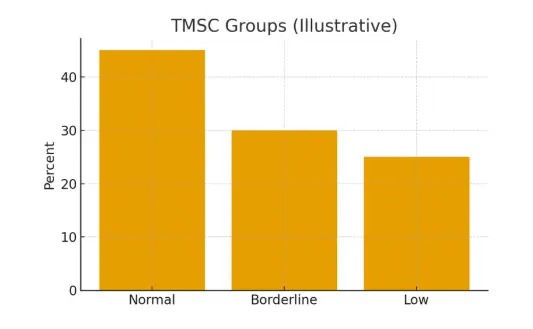
This guide goes beyond the numbers — explaining how TMSC (Total Motile Sperm Count) and morphology fit into your fertility pathway, when to act, and how to interpret results to improve success rates and manage costs effectively.
Understanding the Basics: Where Semen Analysis Fits in the Journey
A semen analysis is typically the first step in fertility diagnostics for couples trying to conceive for six months to a year without success. The test measures several factors including:
- Volume: Total amount of semen produced.
- Concentration: Number of sperm per milliliter.
- Motility: How well sperm move (progressive or non-progressive).
- Morphology: The shape and structure of sperm.
- TMSC (Total Motile Sperm Count): A key metric combining volume, concentration, and motility.
Why It Matters in IVF and Fertility Planning
In IVF programs, these numbers help clinics tailor stimulation and insemination timing. For instance, a lower TMSC might prompt a clinic to recommend ICSI (Intracytoplasmic Sperm Injection), while normal morphology may support standard IVF insemination. Understanding this data early helps reduce uncertainty and improve success rates across the fertility journey.
Eligibility Signals: When to Escalate or Pause
Not every variation in semen results requires immediate intervention. The key is pattern recognition over time:
- Stable but low TMSC: Optimize lifestyle factors and repeat testing after 6–8 weeks.
- Fluctuating morphology: Check for lab consistency and timing of abstinence.
- Severe abnormalities: Consider early referral to a fertility urologist in NYC or your local region.
When results remain inconclusive, escalating to diagnostic imaging or hormonal profiling can uncover hidden causes like varicoceles or testosterone imbalance. Knowing when to pause and when to escalate can prevent unnecessary costs and emotional fatigue.
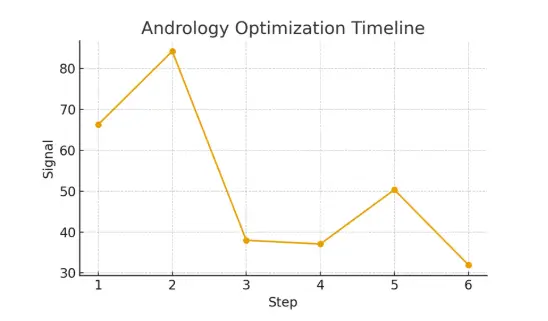
Step-by-Step: Timing Checkpoints in the Fertility Journey
Timing is critical in fertility care. Here’s how semen analysis fits into your overall plan:
Step 1: Initial Testing (Cycle 0)
Complete a baseline semen analysis along with hormone testing and ultrasound for both partners.
Step 2: Review & Optimization (1–2 months)
Make lifestyle adjustments — sleep, diet, supplements, and abstinence periods.
Step 3: Repeat Testing (3 months)
Sperm regeneration cycles take around 70–90 days. Re-testing confirms whether interventions worked.
Step 4: Treatment Matching (Cycle 3–6)
Data guides whether to proceed with IUI, IVF, or ICSI, based on motility and morphology outcomes.
Step 5: Monitoring and Adjustment
Track results through subsequent cycles to refine protocols and maximize IVF success rates.
Pros, Cons, and Practical Costs
Advantages of Early Semen Testing
- Non-invasive and affordable.
- Provides baseline metrics for male fertility health.
- Helps forecast which fertility pathway (IUI, IVF, ICSI) is most suitable.
Limitations
- One test is rarely enough; sperm parameters can vary by as much as 30%.
- Results depend on timing, abstinence period, and lab calibration.
- Emotional stress and overinterpretation can cloud judgment.
Cost Breakdown Example (NYC Fertility Clinics)
Understanding your potential costs upfront helps you plan your fertility journey more effectively. Below is an approximate cost breakdown for common male fertility diagnostics in NYC clinics:
Average Fertility Testing Costs in NYC
Semen Analysis: $150 – $300
A basic but essential test that evaluates sperm count, motility, and morphology.
Hormone Panel (FSH, LH, Testosterone): $200 – $400
Checks hormonal balance and identifies underlying causes of male infertility.
Ultrasound (Optional): $200 – $500
Used to detect structural or vascular issues affecting sperm production.
Specialist Consultation: $250 – $500
Includes review of lab results, diagnosis explanation, and personalized fertility plan.
Average fertility testing costs in NYC range between $600 – $1,500, depending on clinic type and insurance coverage.
Outcome Drivers: What You Control vs. What You Monitor
Factors You Can Control
- Nutrition, hydration, and avoiding excessive heat or alcohol.
- Managing stress levels and maintaining healthy weight.
- Ensuring 2–5 days of abstinence before sample collection.
Factors You Only Monitor
- Genetic quality of sperm.
- Lab methodology and analysis technique.
- Uncontrollable variables like hormonal cycles or external stressors.
Questions to Ask Your Fertility Clinic
- How often should semen analysis be repeated?
- What are the cutoff ranges for TMSC and morphology in your lab?
- Can results improve naturally before moving to IVF?
- How do you decide between IUI and IVF based on these metrics?
- What are the realistic timelines and success rates for each option?
Having these questions ready simplifies communication and ensures that decisions are based on both science and compassion.
Expert Quote
“Protect timing and keep plans simple—quality improves when noise goes down.”
— Clinical Team
This insight reflects the essence of fertility care — reducing unnecessary complexity to enhance both experience and success.
Patient Case Study
A Manhattan couple faced months of inconclusive results. After aligning their testing schedule, adjusting lifestyle factors, and coordinating with a fertility specialist, they gained clarity. Their improved TMSC led to a simplified IVF plan, reducing cycle cancellations and improving pregnancy predictability.
Testimonials
“The steps finally made sense.” — A.&J., Manhattan
“Costs were clear; no surprise bills.” — L., Hoboken
“Nurses replied fast with practical coaching.” — K.&V., Queens
Additional Insights
- Cycle cancellation criteria improve patient experience by reducing delays.
- Trigger timing enhances implantation odds through biologically aligned lab cutoffs.
- Male factor optimization reduces variability, improving IVF success rates.
- Embryo culture control increases budget predictability.
- ICSI or insemination ensures stable outcomes by managing lab precision.
Next Steps with Surrogacy4All
At Surrogacy4All, we simplify the fertility journey through clarity, compassion, and evidence-based care. Whether you’re at the early testing stage or preparing for IVF in NYC, our clinical team helps you understand your data, set expectations, and control costs.
Start your journey today — schedule a free 15-minute nurse consultation, upload your labs for a second opinion, or request a cost breakdown tailored to your case. With Surrogacy4All, your fertility care becomes transparent, predictable, and focused on results.
Frequently Asked Questions (FAQs)
Q. What is the role of semen analysis in IVF success rates?
Ans. It helps clinics match the right treatment — IUI, IVF, or ICSI — to improve fertilization chances and overall success rates.
Q. How do fertility costs vary across NYC?
Ans. Costs differ based on diagnostic depth, medications, and clinic reputation. On average, a single IVF cycle in NYC costs between $12,000 – $18,000, excluding medications.
Q. Can semen quality improve naturally before IVF?
Ans. Yes. Diet, exercise, supplements (like CoQ10 and zinc), and managing heat exposure can improve motility and morphology within 3 months.
Q. How many cycles are typical in a fertility journey?
Ans. It varies per case. Clinics often plan multiple cycles to improve cumulative pregnancy chances, not just single-cycle success.
Q. How can I manage IVF costs effectively?
Ans. Ask for transparent billing, insurance checks, and package plans. Surrogacy4All offers detailed cost breakdowns to help you plan confidently.
Related Links

Dr. Kulsoom Baloch
Dr. Kulsoom Baloch is a dedicated donor coordinator at Egg Donors, leveraging her extensive background in medicine and public health. She holds an MBBS from Ziauddin University, Pakistan, and an MPH from Hofstra University, New York. With three years of clinical experience at prominent hospitals in Karachi, Pakistan, Dr. Baloch has honed her skills in patient care and medical research.