This article explains Deciding When to Use Frozen Eggs within the Egg Freezing & Fertility Preservation pathway. We focus on practical choices that shape outcomes, budgets, emotions, and timelines—so you can move forward with clarity and confidence.
What It Is
Deciding when to use your frozen eggs, in plain English:
- How to know when the right time has arrived
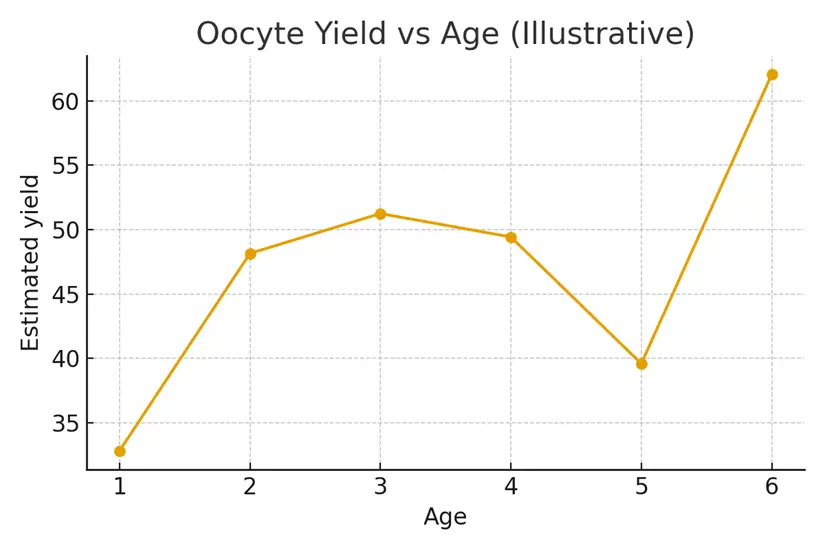
- What factors influence success rates
- How age, medical history, and family-building goals interact
- How upstream decisions (egg number, storage time, relationship status, finances) affect downstream results (fertilization, embryo quality, pregnancy rates)
This decision is part medical, part emotional, and part logistical—this guide helps you navigate all three.
Who It Helps
This section is especially helpful for individuals who:
- Are approaching the age or life stage where using frozen eggs feels timely
- Have partner changes, shifts in health, or new reproductive priorities
- Previously froze eggs and now want clear next steps
- Are considering IVF with a partner or donor
- Need clarity on success probabilities based on the number of eggs stored
Signals that suggest this section fits your situation:
- You are now older than when you froze eggs
- You are planning a pregnancy soon
- Your AMH/AFC have declined and you want to rely on previously stored eggs
- You want to avoid multiple fresh IVF cycles
- You want to compare frozen egg success rates vs trying naturally or doing a fresh retrieval
Step-by-Step
A simple, structured process with clear checkpoints:
- Review Your Frozen Egg Inventory
Number of eggs, maturity status (MII), and storage time. - Understand Success Probabilities
The clinic estimates how many embryos—and potential pregnancies—you can expect based on your egg count and age at freezing. - Define Your Family-Building Goal
One child? Two? Keeping future options open? - Select Fertilization Method
Partner vs donor, ICSI, genetic testing options. - Plan the Embryo Transfer Timeline
Coordinate with your cycle, medical history, travel, and work schedule. - Create a Backup Plan
Such as a supplemental fresh retrieval if egg numbers are limited. - Finalize Consent + Logistics
Confirm release forms, clinic coordination, storage handling, and transport (if switching clinics).
Pros & Cons
Pros
- Allows you to use eggs preserved at a younger age
- Avoids repeating stimulation cycles
- Shortens the timeline to pregnancy
- Predictable costs and fewer medications
- Higher emotional control and mental readiness
Cons
- Frozen eggs still carry attrition (not all will fertilize or develop)
- May require multiple eggs to create one healthy embryo
- Additional IVF steps (fertilization, culture, PGT-A, transfer) still apply
- Uncertainty around how many embryos will result
- Emotional pressure when egg supply is limited
Costs & Logistics
Typical line items include:
- Egg thaw fees
- ICSI fertilization
- Embryo culture (3–5 days)
- Optional genetic testing (PGT-A)
- Embryo freezing and/or transfer fees
- Storage fees (if embryos remain)
- Medications for endometrial preparation
- Transport costs if eggs are moved between clinics
Understanding prior authorizations, insurance coverage (if any), and cash-flow timing helps avoid surprise bills.
What Improves Outcomes
Meaningful actions that change results:
- Choosing the embryo transfer protocol that best fits your medical profile
- Reviewing prior cycle data to refine strategy
- Addressing uterine factors (polyps, fibroids, lining quality) beforehand
- Optimizing partner or donor sperm quality
- Being realistic about success probabilities per egg
Actions that rarely change outcomes:
- Supplements alone
- Switching clinics without a clear reason
- Over-testing or unnecessary add-ons
Case Study
A 36-year-old who froze 14 mature eggs at age 31 returned five years later hoping for her first child. After reviewing her egg count and age-at-freezing success probabilities, the clinic estimated she likely had enough eggs for 1–2 embryos. She proceeded with thawing, fertilization via ICSI, and a transfer-ready embryo emerged by day 5. Clear communication, success modeling, and pre-planned consent helped her avoid delays and feel in control of her next steps.
Mistakes to Avoid
- Waiting too long to review your egg inventory and success estimates
- Assuming every frozen egg will turn into an embryo
- Not planning for a fresh retrieval backup if your egg count is limited
- Starting the thawing process without clarified family goals
- Overlooking sperm quality, which significantly affects outcomes
- Underestimating administrative steps (consent forms, storage releases, transport scheduling)
FAQs
Q. How many frozen eggs do I need for one baby?
Ans. It varies by age at freezing, but most clinics estimate 8–12 mature eggs per expected live birth.
Q. Does storage time reduce egg quality?
Ans. Not significantly. Eggs remain stable in cryostorage; age at freezing is what matters most.
Q. Should I thaw all my eggs at once?
Ans. Most clinics recommend thawing in batches based on your goals and expected embryo yield.
Q. Can I use donor sperm with my frozen eggs?
Ans. Yes. Donor sperm can be used for fertilization anytime, provided consent and logistics are in place.
Q. What if my thawed eggs do not fertilize?
Ans. A backup plan (such as a fresh cycle or donor option) ensures you’re not left without next steps.
Next Steps
- Free 15-min nurse consult
- Upload your labs
- Get a personalized cost breakdown for your case
Related Links

Dr. Kulsoom Baloch
Dr. Kulsoom Baloch is a dedicated donor coordinator at Egg Donors, leveraging her extensive background in medicine and public health. She holds an MBBS from Ziauddin University, Pakistan, and an MPH from Hofstra University, New York. With three years of clinical experience at prominent hospitals in Karachi, Pakistan, Dr. Baloch has honed her skills in patient care and medical research.