Polycystic Ovary Syndrome (PCOS) affects nearly one in ten women of reproductive age and is one of the most common causes of infertility. Understanding the PCOS test panel—particularly how to interpret LH/FSH, AMH, and ultrasound results—is crucial for creating a personalized fertility plan. Within the FertilityTesting & Diagnostics pathway, these tests help doctors predict egg quality, ovarian reserve, and hormonal balance, allowing for targeted treatments that improve IVF success rates while controlling costs and emotional strain.
1) Definitions and Where This Fits in the Journey
The PCOS test panel typically includes:
- LH (Luteinizing Hormone) and FSH (Follicle-Stimulating Hormone): Their ratio helps determine if ovulation is occurring regularly.
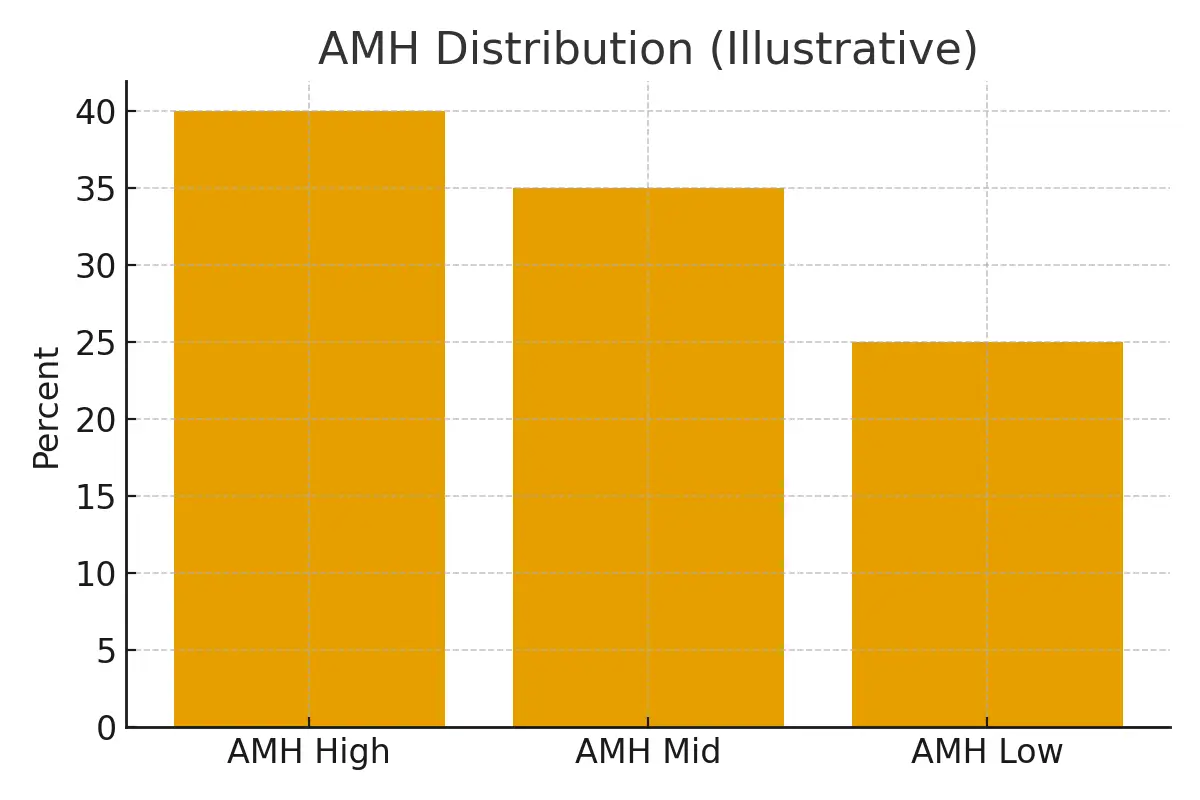
- AMH (Anti-Müllerian Hormone): Indicates ovarian reserve and predicts how the ovaries might respond to stimulation.
- Pelvic Ultrasound: Assesses the number of antral follicles and checks for cystic patterns in the ovaries.
These markers are usually tested early in your fertility journey, ideally on cycle day 2–5, when hormone levels are most stable. For many women in NYC fertility clinics, these tests form the foundation before starting medication or IVF cycles.
2) Eligibility Signals — When to Escalate or Pause
- Escalate testing if you have irregular cycles, persistent acne, excessive hair growth, or unexplained weight changes.
- Pause or monitor if hormones appear borderline, but symptoms are mild—sometimes lifestyle changes improve ovulation naturally.
- Consider IVF or egg freezing if AMH levels are high but ovulation is inconsistent, or if your FSH levels indicate poor ovarian response.
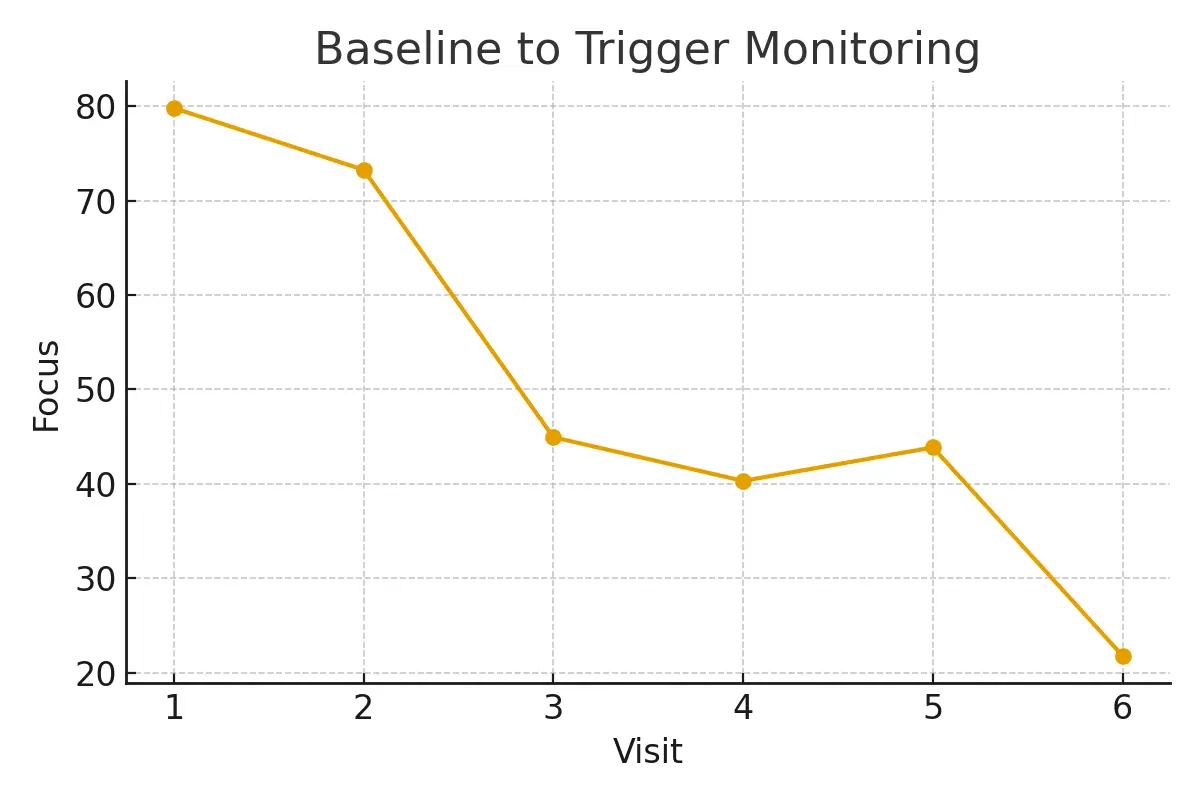
- Proper timing is key. Waiting too long between tests can mislead diagnosis and treatment. Regular updates every 3–6 months help refine your plan.
3) Step-by-Step Testing with Timing Checkpoints
- Cycle Day 2–5: Blood tests for LH, FSH, AMH, and estradiol.
- Mid-Cycle (Day 12–14): Ultrasound and possibly progesterone testing to confirm ovulation.
- Follow-Up Consultation: A fertility specialist reviews hormone ratios and ultrasound findings to identify whether IVF, ovulation induction, or other treatments are suitable.
- Treatment Adjustment: Based on test results, medication doses or stimulation protocols are tailored to avoid overstimulation or under-response.
This systematic approach reduces trial-and-error, keeping your patient journey efficient and predictable.
4) Pros, Cons, and Practical Costs
Pros:
- Early detection of hormonal imbalance.
- Personalized treatment plans that improve IVF success rates.
- Prevents unnecessary medications or procedures.
Cons:
- Hormone levels can fluctuate, requiring repeat testing.
- Insurance may not cover all fertility diagnostics.
- Emotional strain if results are unclear or delayed.
Typical Costs in NYC:
- LH/FSH Blood Test $150–$300
- AMH Test $200–$400
- Pelvic Ultrasound $250–$600
- Full PCOS Panel $600–$1,200
Transparent costs allow patients to plan without surprises, and some clinics offer bundled fertility evaluations.
5) Outcome Drivers — What You Control vs. What You Monitor
You Control:
- Diet, weight, sleep, and stress—all influence hormonal balance.
- Medication adherence and consistent follow-ups.
You Monitor:
- Hormonal trends (LH/FSH ratio, AMH levels).
- Uterine lining and follicle growth via ultrasound.
- Cycle predictability and ovulation quality.
By aligning these controllable factors with lab and ultrasound results, women can improve fertility success rates over multiple cycles while minimizing costs.
6) Questions to Ask Your Clinic
- How often should I repeat my AMH or LH/FSH tests?
- Can lifestyle changes reduce the need for medication?
- What protocol do you recommend for PCOS-related infertility—IVF, IUI, or medication?
- How do your success rates for PCOS patients compare to the NYC average?
- Can I share my lab results for a second opinion before starting treatment?
Expert Quote
“Protect timing and keep plans simple—quality improves when noise goes down.”
— Clinical Team
Patient Case Study
A Manhattan couple underwent multiple inconclusive fertility tests before getting a clear PCOS diagnosis. Once their care team synchronized testing schedules and interpreted AMH and ultrasound data correctly, their IVF cycle became more predictable. The outcome: fewer medications, reduced costs, and a successful embryo transfer.
Testimonials
“The steps finally made sense.” — A. & J., Manhattan
“Costs were clear; no surprise bills.” — L., Hoboken
“Nurses replied fast with practical coaching.” — K. & V., Queens
Next Steps with Surrogacy4All NYC
Schedule your free 15-minute nurse consult, upload your labs for a second opinion, or request a personalized cost breakdown for your fertility case.
At Surrogacy4All, we support patients across NYC and beyond in navigating every step of fertility testing and treatment—from initial diagnostics to IVF and family planning. Our mission is to simplify complex fertility decisions, improve success rates, and make reproductive care accessible and humane. Contact us today!
Frequently Asked Questions (FAQs)
Q. How does AMH relate to IVF success rates?
Ans. Higher AMH generally indicates more eggs available for stimulation, potentially improving IVF outcomes—but quality matters more than quantity.
Q. What is a normal LH/FSH ratio in PCOS?
Ans. Typically, a ratio above 2:1 may suggest PCOS, but exact values depend on lab standards and timing of testing.
Q. How often should I repeat my PCOS panel?
Ans. Every 3–6 months or before starting a new IVF or medication cycle, depending on your specialist’s recommendation.
Q. Does ultrasound confirm PCOS on its own?
Ans. No. It supports diagnosis but must be paired with hormonal tests and clinical symptoms.
Q. Can PCOS patients still conceive naturally?
Ans. Yes, many can—with or without medical help. Early testing and targeted management improve natural and assisted fertility outcomes.

Dr. Kulsoom Baloch
Dr. Kulsoom Baloch is a dedicated donor coordinator at Egg Donors, leveraging her extensive background in medicine and public health. She holds an MBBS from Ziauddin University, Pakistan, and an MPH from Hofstra University, New York. With three years of clinical experience at prominent hospitals in Karachi, Pakistan, Dr. Baloch has honed her skills in patient care and medical research.





