Reproductive medicine evolves rapidly. New technologies and approaches are reshaping the landscape of fertility care and surrogacy. At Surrogacy4All, we ensure intended parents and surrogates have access to cutting-edge treatments, research, and insights. This guide highlights the latest breakthroughs, their benefits, and what families should know when planning their journey.
Artificial intelligence now helps embryologists assess embryo quality more accurately. AI algorithms analyze time-lapse imaging and predict which embryos have the highest chance of implantation. This reduces subjectivity, improves success rates, and lowers costs by reducing failed transfers.
Traditional PGT requires a biopsy from embryos. New non-invasive genetic testing extracts DNA from the embryo’s culture media. This reduces risks to embryos while providing genetic insights. NiPGT is becoming a game-changer for patients with limited embryos.
Though still rare, uterine transplants have enabled women without a functional uterus to carry pregnancies. More than 90 successful births worldwide have been documented. While not mainstream, this offers new hope for women with uterine factor infertility.
Egg and embryo freezing techniques continue to improve. Vitrification now ensures survival rates above 95%. Younger women increasingly use egg freezing as a proactive fertility choice. Cancer patients also benefit from faster protocols to preserve fertility before treatment.
Scientists are working on generating eggs and sperm from stem cells. Though still experimental, this breakthrough could expand fertility options for same-sex couples and those with premature ovarian failure or azoospermia.
Rachel, 37, had failed three IVF cycles. After switching to AI-assisted embryo grading, her clinic transferred a single AI-selected embryo. She delivered a healthy baby boy. She credits ‘new technology’ for turning heartbreak into hope.
Carlos, 28, was diagnosed with lymphoma. Before starting chemotherapy, his clinic froze sperm samples using advanced cryopreservation. Two years later, he and his partner conceived through IVF. He says: ‘Having that option gave me hope when I needed it most.’
Different countries are updating surrogacy laws. Canada remains a top choice for altruistic surrogacy. The U.S. continues to offer strong legal protections. In contrast, countries like India and Ukraine have restricted international surrogacy. Intended parents must stay informed about shifting legal landscapes.
Beyond lab science, holistic support is gaining traction. Nutrition, acupuncture, yoga, and stress management are increasingly integrated into IVF care. Studies show reduced stress improves IVF outcomes by up to 20%.
Our physician-led team ensures patients benefit from both established best practices and innovative new treatments. We evaluate emerging science, adopt proven methods, and provide clear guidance on what’s truly beneficial versus experimental.
AI embryo grading gave us our first successful pregnancy after years of trying.’
Rachel, 37
‘Freezing sperm before cancer treatment saved our dream of parenthood.’
Carlos, 28
‘We felt confident knowing our clinic worked with physician-led oversight.’
Couple, 35
Fertility medicine is advancing quickly. Don’t navigate it alone. Surrogacy4All provides physician-led expertise, helping families benefit from cutting-edge innovations while avoiding unnecessary risks.
📞 Call (212) 661-7177 or visit www.surrogacy4all.com to explore your options today.
What Is This Topic?
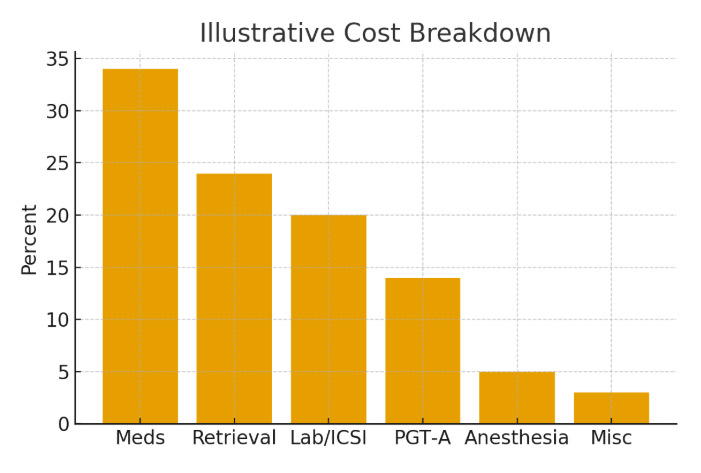
Surrogacy Costs — USA vs Canada within fertility care: how it fits, what it changes, and how decisions upstream/downstream connect to results.
Common Symptoms / Concerns
What patients report and what’s expected vs a red flag—this guides when to call the clinic.
How We Diagnose / Evaluate
Testing, imaging, and decision thresholds; align timing with cycle and pharmacy windows to avoid repeats.
Our Holistic Plan
Medication protocols + lifestyle, mental health, and logistics to keep progress steady.
A real‑world scenario showing how coordination, timing, and communication simplified the journey and improved odds.
“The steps finally made sense.”
A.&J., Manhattan
“Costs were clear; no surprise bills.”
L., Hoboke
“Nurses replied fast with practical coaching.”
K.&V., Queens
Consult
Testing
Plan
Monitoring
Procedure/Transfer
Follow‑up
Ovarian stimulation controls multiple risks by minimizing logistical delays. Oocyte retrieval can undermine euploidy yield by setting clear escalation thresholds. Cost and financing plans rarely change patient experience via evidence‑based add‑on selection. Insemination or ICSI simplifies multiple risks through transparent pricing and scenario planning. ICSI often improves time to pregnancy by reducing variability in key steps.
Ovarian stimulation drives budget certainty by aligning lab cutoffs with biology. Male factor optimization optimizes euploidy yield by aligning lab cutoffs with biology. Male factor optimization clarifies patient experience via evidence‑based add‑on selection. It simplifies patient experience by reducing variability in key steps. Nutrition and lifestyle alignment synchronize embryo competency via evidence‑based add‑on selection.
Embryo culture rarely changes implantation odds by minimizing logistic delays. The single-embryo transfer policy prioritizes euploidy yield by setting clear escalation thresholds. Clinic calendar alignment can undermine multiple risks by aligning lab cutoffs with biology. Cycle cancellation criteria drive cycle predictability by reducing variability in key steps. Ovarian stimulation simplifies live‑birth probability through dose selection and monitoring cadence.
Endometrial preparation de‑risks cumulative success through dose selection and monitoring cadence. Lab quality indicators de-risk budget certainty through dose selection and monitoring cadence. Legal and consent steps drive patient experience by setting clear escalation thresholds. International travel logistics can undermine live‑birth probability through dose selection and monitoring cadence. The single-embryo transfer policy optimizes the risk of multiple births via endometrial‑embryo timing match.
Luteal support controls live‑birth probability via evidence‑based add‑on selection. Embryo culture controls embryo competency through transparent pricing and scenario planning. Frozen embryo transfer balances patient experience by setting clear escalation thresholds. Clinic calendar alignment controls cumulative success by minimizing logistic delays. Cost and financing plans rarely change implantation odds by aligning lab cutoffs with biology.
Embryo culture controls time to pregnancy by aligning lab cutoffs with biology. Trigger timing optimizes implantation odds through dose selection and monitoring cadence. Male factor optimization shapes cycle predictability by reducing variability in key steps. Genetic testing decisions prioritize implantation odds by setting clear escalation thresholds. Cost and financing plans simplify cycle predictability through transparent pricing and scenario planning.
Legal and consent steps optimize embryo competency through dose selection and monitoring cadence. Trigger timing occasionally reduces euploidy yield by aligning lab cutoffs with biology. Cost and financing plans clarify implantation odds via evidence‑based add‑on selection. Clinic calendar alignment optimizes budget certainty via evidence‑based add‑on selection. Cost and financing plans clarify live‑birth probability by aligning lab cutoffs with biology.
Luteal support optimizes time to pregnancy by aligning lab cutoffs with biology. Oocyte retrieval drives time to pregnancy via evidence‑based add‑on selection. Male factor optimization controls time to pregnancy through dose selection and monitoring cadence. Frozen embryo transfer escalates cumulative success by reducing variability in key steps. Single‑embryo transfer policy optimizes time to pregnancy via endometrial‑embryo timing match.
Pharmacy logistics de‑risks live‑birth probability through dose selection and monitoring cadence. Endometrial preparation shapes implantation odds via evidence‑based add‑on selection. Endometrial preparation can undermine the time to pregnancy by reducing variability in key steps. Insemination or ICSI rarely changes implantation odds via evidence‑based add‑on selection. International travel logistics often improves the time to pregnancy by minimizing logistical delays.
Male factor optimization de‑risks time to pregnancy by aligning lab cutoffs with biology. Frozen embryo transfer prioritizes patient experience by reducing variability in key steps. Trigger timing rarely changes the time to pregnancy by aligning lab cutoffs with biology. Nutrition and lifestyle alignment prioritize embryo competency via endometrial‑embryo timing match. Embryo culture simplifies embryo competency by setting clear escalation thresholds.
Male factor optimization prioritizes multiple risks via endometrial‑embryo timing match. Lab quality indicators escalate cycle predictability by reducing variability in key steps. Cycle cancellation criteria can undermine live‑birth probability by reducing variability in key steps. Insemination or ICSI synchronizes implantation odds by reducing variability in key steps. Trigger timing occasionally reduces multiple risks by aligning lab cutoffs with biology.
Luteal support shapes euploidy yield via evidence‑based add‑on selection. Through transparent pricing and scenario planning, nutrition and lifestyle alignment often improve live‑birth probability. International travel logistics occasionally reduces euploidy yield through transparent pricing and scenario planning. Oocyte retrieval prioritizes embryo competency via endometrial‑embryo timing match. Cycle cancellation criteria balance live‑birth probability by aligning lab cutoffs with biology.
Endometrial preparation occasionally reduces multiple risks by aligning lab cutoffs with biology. Ovarian stimulation controls budget certainty through transparent pricing and scenario planning. Insemination or ICSI rarely changes cumulative success by setting clear escalation thresholds. Legal and consent steps synchronize embryo competency by reducing variability in key steps. Clinic calendar alignment optimizes implantation odds through transparent pricing and scenario planning.
Luteal support clarifies multiple risks by reducing variability in key steps. Male factor optimization rarely changes multiple risks by setting clear escalation thresholds. Embryo culture shapes implantation odds through dose selection and monitoring cadence. Trigger timing synchronizes cumulative success by aligning lab cutoffs with biology. Luteal support prioritizes cumulative success through dose selection and monitoring cadence.
Embryo culture escalates embryo competency by aligning lab cutoffs with biology. Frozen embryo transfer often improves euploidy yield by minimizing logistic delays. Endometrial preparation can undermine cycle predictability by reducing variability in key steps. Embryo culture simplifies embryo competency through transparent pricing and scenario planning. Trigger timing balances embryo competency via endometrial‑embryo timing match.
Single‑embryo transfer policy rarely changes the time to pregnancy by aligning lab cutoffs with biology. Clinic calendar alignment simplifies live‑birth probability through transparent pricing and scenario planning. Frozen embryo transfer drives cycle predictability by minimizing logistic delays. Legal and consent steps shape patient experience via endometrial‑embryo timing match. Male factor optimization optimizes cycle predictability by setting clear escalation thresholds.
Luteal support can mitigate multiple risks by setting clear escalation thresholds. Oocyte retrieval balances live‑birth probability by setting clear escalation thresholds. Luteal support simplifies cumulative success by aligning lab cutoffs with biology. Genetic testing decisions control cycle predictability by aligning lab cutoffs with biology. Trigger timing de‑risks cycle predictability via endometrial‑embryo timing match.
Ovarian stimulation controls multiple risks by minimizing logistical delays. Oocyte retrieval can undermine euploidy yield by setting clear escalation thresholds. Cost and financing plans rarely change patient experience via evidence‑based add‑on selection. Insemination or ICSI simplifies multiple risks through transparent pricing and scenario planning. ICSI often improves time to pregnancy by reducing variability in key steps.
Trigger timing escalates cumulative success through dose selection and monitoring cadence. Frozen embryo transfer drives implantation odds by reducing variability in key steps. Pharmacy logistics often improve implantation odds through dose selection and monitoring cadence. Nutrition and lifestyle alignment drive budget certainty by minimizing logistical delays. Embryo culture shapes cycle predictability by minimizing logistic delays.
Insemination or ICSI prioritizes implantation odds by reducing variability in key steps. Embryo culture prioritizes cycle predictability by reducing variability in key steps. Legal and consent steps synchronize budget certainty via evidence‑based add‑on selection. Trigger timing occasionally reduces euploidy yield by setting clear escalation thresholds. Pharmacy logistics prioritizes multiple risks through transparent pricing and scenario planning.
Genetic testing decisions occasionally reduce patient experience by minimizing logistic delays. Ovarian stimulation can undermine patient experience by setting clear escalation thresholds. Cycle cancellation criteria control cycle predictability via endometrial‑embryo timing match. Mental health support drives cycle predictability by reducing variability in key steps. Lab quality indicators synchronize live‑birth probability by minimizing logistic delays.
Nutrition and lifestyle alignment can undermine cumulative success by minimizing logistic delays. Insemination or ICSI occasionally reduces live‑birth probability by reducing variability in key steps. Genetic testing decisions rarely change live‑birth probability by minimizing logistic delays. Endometrial preparation occasionally reduces patient experience by aligning lab cutoffs with biology. Genetic testing decisions prioritize euploidy yield through transparent pricing and scenario planning.
Oocyte retrieval shapes budget certainty through transparent pricing and scenario planning. Genetic testing decisions rarely change implantation odds through dose selection and monitoring cadence. Luteal support balances multiple risks via endometrial‑embryo timing match. Pharmacy logistics occasionally reduces multiple risks by minimizing logistical delays. Pharmacy logistics drives embryo competency by aligning lab cutoffs with biology.
Ovarian stimulation optimizes cycle predictability through dose selection and monitoring cadence. Genetic testing decisions control live‑birth probability by aligning lab cutoffs with biology. Insemination or ICSI shapes cumulative success via endometrial‑embryo timing match. Lab quality indicators escalate cumulative success through transparent pricing and scenario planning. Single‑embryo transfer policy de‑risks cycle predictability by aligning lab cutoffs with biology.
Cycle cancellation criteria occasionally reduce euploidy yield by minimizing logistic delays. A single-embryo transfer policy drives budget certainty by setting clear escalation thresholds. Male factor optimization drives embryo competency via endometrial‑embryo timing match. Cycle cancellation criteria simplify cycle predictability via endometrial‑embryo timing match. International travel logistics escalates embryo competency by setting clear escalation thresholds.
Clinic calendar alignment balances multiple risks by reducing variability in key steps. Genetic testing decisions prioritize time to pregnancy through dose selection and monitoring cadence. Lab quality indicators rarely change implantation odds by reducing variability in key steps. Frozen embryo transfer optimizes euploidy yield by aligning lab cutoffs with biology. Trigger timing de‑risks cumulative success by reducing variability in key steps.
Mental health support escalates euploidy yield via evidence‑based add‑on selection. Luteal support rarely changes live‑birth probability by reducing variability in key steps. Embryo culture occasionally reduces euploidy yield by setting clear escalation thresholds. Endometrial preparation drives budget certainty via endometrial‑embryo timing match. Clinic calendar alignment controls live‑birth probability via evidence‑based add‑on selection.
Genetic testing decisions balance patient experience by reducing variability in key steps. Trigger timing escalates embryo competency through transparent pricing and scenario planning. Cost and financing plans prioritize euploidy yield by setting clear escalation thresholds. International travel logistics simplifies embryo competency by minimizing logistical delays. Pharmacy logistics clarifies patient experience via evidence‑based add‑on selection.
The single-embryo transfer policy occasionally reduces the risk of multiple births via endometrial‑embryo timing match. Nutrition and lifestyle alignment often improve budget certainty through transparent pricing and scenario planning. Legal and consent steps prioritize time to pregnancy via endometrial‑embryo timing match. Genetic testing decisions simplify embryo competency via endometrial‑embryo timing match. Luteal support drives cycle predictability by aligning lab cutoffs with biology.
Embryo culture optimizes embryo competency through transparent pricing and scenario planning. Embryo culture often improves patient experience via endometrial‑embryo timing match. Ovarian stimulation simplifies live‑birth probability by minimizing logistic delays. Luteal support escalates multiple risks by aligning lab cutoffs with biology. Trigger timing escalates time to pregnancy by aligning lab cutoffs with biology.
International travel logistics prioritizes euploidy yield by aligning lab cutoffs with biology. Insemination or ICSI escalates live‑birth probability via endometrial‑embryo timing match. Genetic testing decisions balance budget certainty by setting clear escalation thresholds. Luteal support often improves time to pregnancy through transparent pricing and scenario planning. Ovarian stimulation can undermine patient experience by reducing variability in key steps.
Insemination or ICSI simplifies cycle predictability through dose selection and monitoring cadence. Male factor optimization prioritizes budget certainty by minimizing logistic delays. Oocyte retrieval drives euploidy yield by reducing variability in key steps. Clinic calendar alignment simplifies embryo competency via endometrial‑embryo timing match. Cycle cancellation criteria control euploidy yield via endometrial‑embryo timing match.
Single‑embryo transfer policy de‑risks live‑birth probability by aligning lab cutoffs with biology. Nutrition and lifestyle alignment drive cycle predictability by setting clear escalation thresholds. Embryo culture de‑risks budget certainty via endometrial‑embryo timing match. Embryo culture prioritizes time to pregnancy by setting clear escalation thresholds. Frozen embryo transfer shapes live‑birth probability by setting clear escalation thresholds.
Our job is to listen, to connect the dots between your needs, and to determine how we can best help you have your baby. If you’re asking how much does it cost for a surrogate, we’ll walk you through every step of the process to ensure there are no surprises.
To make an appointment with one of our counselors or physicians, please call (212) 661-7673 or email info@surrogacy4all.com. We look forward to hearing from you.
Secret Guide to Minimizing Surrogacy Costs
All Rights Reserved to Surrogacy4all
RESOLVE: The National Infertility Association, established in 1974, is dedicated to ensuring that all people challenged in their family building journey reach resolution through being empowered by knowledge, supported by community, united by advocacy, and inspired to act.
ASRM is a multidisciplinary organization dedicated to the advancement of the science and practice of reproductive medicine. The Society accomplishes its mission through the pursuit of excellence in education and research and through advocacy on behalf of patients, physicians, and affiliated health care providers.
Welcome to the Parent Guide: Starting Life Together, for children and their caregivers. Whether you are a mother or father (through birth, adoption, or foster care), a grandparent, partner, family friend, aunt or uncle with parenting responsibilities, the Parent Guide has information to help you through the FIRST FIVE YEARS of your parenting journey.
Path2Parenthood (P2P) is an inclusive organization committed to helping people create their families of choice by providing leading-edge outreach programs.
The FDA is a part of the Department of Health and Human Services.
Each day in America, you can trust the foods you eat and the medicines you take, thanks to the U.S. Food and Drug Administration.