In the context of fertility testing and diagnostics, understanding the role of vitamin D, HbA1c (glycated haemoglobin), and broader metabolic labs can help couples and clinicians make smarter decisions. In this article, we’ll explore how these biomarkers fit into the fertility journey, who benefits, how timing affects outcomes, realistic costs (especially in a fertility-clinic pathway), and decision rules to keep care simple and humane.
Here’s what we’ll cover: definitions, eligibility signals, step-by-step timing checkpoints, pros/cons & line-item costs, outcome drivers you control vs those you monitor, key questions for your clinic, and a real patient case study. An expert quote sets the tone:
1) Definitions and Where This Fits in the Journey
What is Vitamin D?
Vitamin D (typically measured as serum 25-hydroxyvitamin D) is a fat-soluble vitamin/hormone that contributes to bone health, immune regulation, and increasingly is seen as influencing metabolic and reproductive health. Research shows that vitamin D deficiency is common in reproductive-age women, and low levels may correlate with poorer fertility or IVF outcomes.
What is HbA1c?
HbA1c reflects the percentage of haemoglobin that is glycated (i.e., sugar-bound) and gives a medium-term view (roughly 3 months) of average blood glucose control. In fertility care, elevated HbA1c may signal insulin resistance or pre-diabetes/diabetes — conditions that can impact ovulation, embryo quality, endometrial health, and pregnancy outcomes.
What are Metabolic Labs?
Here, we mean a broader panel including fasting glucose, insulin, HOMA-IR (insulin resistance estimate), lipid profile, BMI/waist circumference, blood pressure, inflammatory markers, etc. These labs give insight into metabolic health, which is increasingly recognised as important in fertility.
Where They Fit in the Fertility Testing & Diagnostics Pathway
In the fertility journey, you often start with basic hormone tests (AMH, FSH/LH, progesterone), imaging, and partner semen analysis. Metabolic labs and vitamin D/HbA1c often come in under these conditions:
- pre-treatment baseline (before ovulation induction or IVF)
- optimisation phase (pre-cycle) to improve odds
- monitoring phase (if there are metabolic risks)
2) Eligibility Signals and When to Escalate or Pause
Who should have these labs?
Consider adding vitamin D, HbA1c and metabolic labs if any of the following are present:
- BMI > 30 or central obesity
- History of polycystic ovary syndrome (PCOS) or insulin resistance
- Irregular cycles or ovulation issues
- Prior IVF/IUI cycles with poor response or high cancellation rate
- Prior pregnancy complications (gestational diabetes, pre-eclampsia)
- Low vitamin D exposure (limited sun, darker skin, geography)
- Male partner with metabolic syndrome features (obesity, dyslipidaemia)
When to escalate or pause the cycle
- If HbA1c is significantly elevated (eg >6.0–6.5 % depending on clinic) → consider optimising glucose control before starting stimulation.
- If vitamin D is very low (eg <20 ng/mL) → supplementation and re-check before major cycle.
- If metabolic labs show uncontrolled dyslipidaemia or hypertension → stabilise these before proceeding.
- Pause and recalibrate if multiple failed cycles may be driven by metabolic dysfunction rather than embryo quality alone.
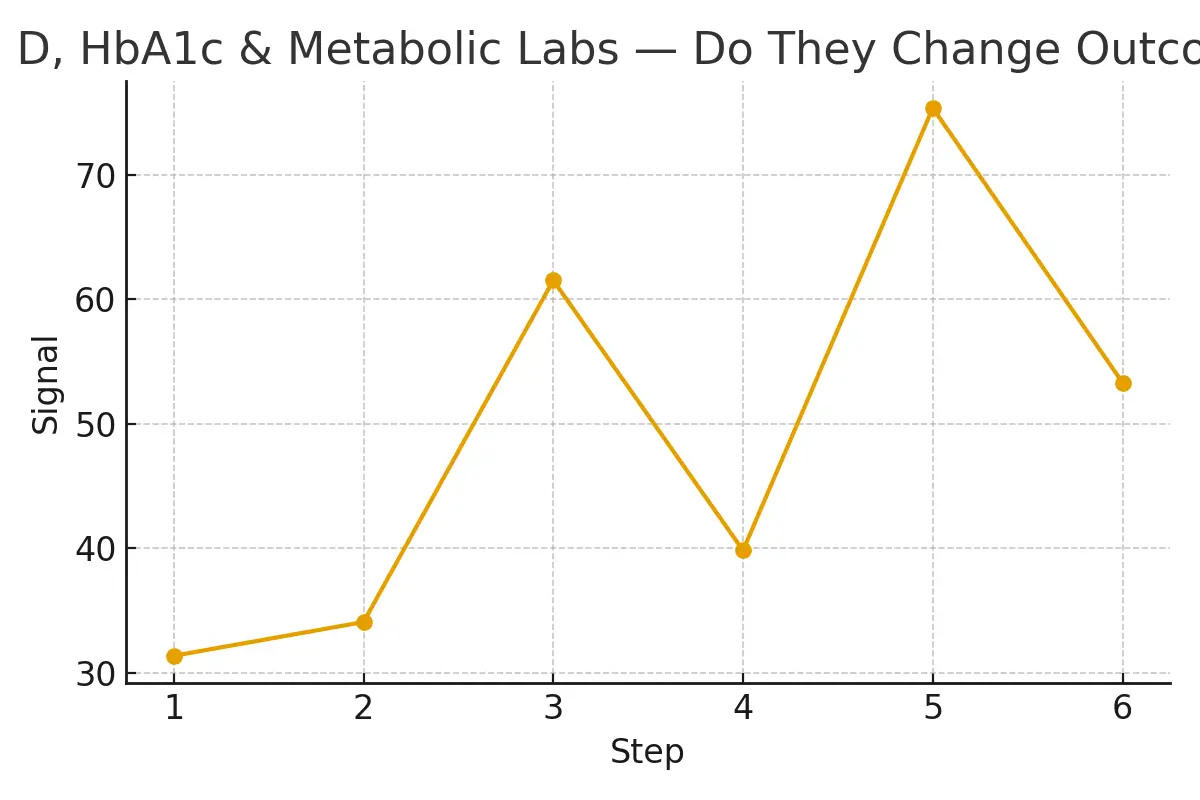
3) Step-by-Step with Timing Checkpoints
Here is a simplified timeline in a fertility pathway where these labs might be used:
Pre-treatment baseline (3-4 months before cycle start)
Order vitamin D, HbA1c, fasting glucose/insulin, lipid profile, BP/waist circumference.
Review results with the clinic nurse or endocrinologist.
Optimisation phase (2-3 months before stimulation)
If vitamin D is low → begin supplementation (eg 2,000–5,000 IU daily or as per clinic).
If HbA1c/elevated glucose → diet + exercise + endocrinology referral.
Lifestyle supports (sleep, exercise, low glycaemic diet) to boost metabolic fertility.
Pre-stimulation check-in (2–4 weeks before cycle)
Re-check vitamin D level (to achieve target, e.g., ≥30–40 ng/mL).
Confirm HbA1c/glucose is acceptable.
Confirm blood pressure and lipids are stable.
Stimulation/embryo development phase
Metabolic labs may guide dose adjustments for stimulation, endometrial prep.
Transfer/endometrium phase
Some clinics monitor metabolic markers since insulin resistance and inflammation can affect receptivity.
Post-treatment follow-up
Review labs, document outcomes, and adjust for next cycle.
4) Pros, Cons, and Practical Costs with Line-Item Examples
Pros
- Improved ability to personalise treatment: clinics can adjust stimulation, diet, and timing based on metabolic health.
- Potential for better outcomes: vitamin D supplementation has been shown to improve HbA1c and glycaemic markers in metabolic studies.
- Reduced cancellation risk: better metabolic health often means better response and fewer surprises mid-cycle.
- Transparent cost/budget planning: Labs are relatively inexpensive compared to full fertility cycle costs.
Cons
- Additional cost and time: pushing out the cycle start might delay treatment.
- The evidence is still somewhat mixed: not all studies show large gains from vitamin D or metabolic optimisation in the fertility context.
- Over-testing risk: Some labs may not add value if the patient is low risk.
Practical Costs (example line-items, approximate)
- Vitamin D 25-OH test: US$30-$60 (or equivalent local currency)
- HbA1c: US$20-$40
- Fasting glucose + insulin + HOMA-IR: US$40-$80
- Lipid profile + waist, BP: US$30-$50
- Supplementation (vitamin D) for 2-3 months: US$20-$50.
Practical tip
Ask your clinic for a “metabolic optimisation add-on” budget line so you know the extra labs and timeline ahead of the artificial fertility treatment.
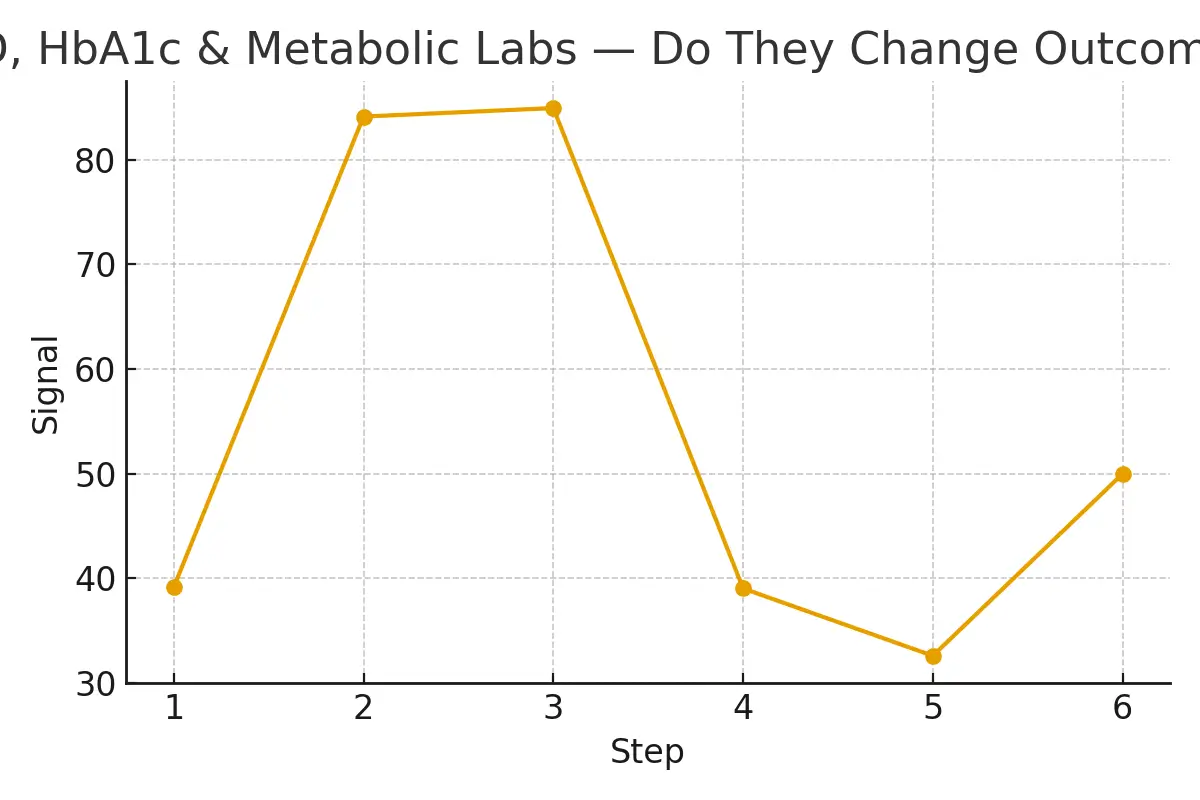
5) Outcome Drivers You Control vs Those You Monitor
What you can control
- Vitamin D level: through supplementation and sun exposure.
- Glucose control / HbA1c: via diet, exercise, and medication if needed.
- Metabolic health: weight, waist circumference, blood pressure, lipids.
- Timing: giving yourself the 2–3 months pre-cycle to optimise.
What you monitor, but cannot always fully control
- Baseline ovarian reserve/embryo quality.
- Partner sperm quality (though metabolic health affects this too).
- Genetic factors, age-related decline.
- Lab/clinic procedural factors (lab quality, culture media).
Why this distinction matters
Focusing on controllable drivers means you reduce “noise” in your fertility plan. By stabilising vitamin D, glucose, and metabolic markers, you give your clinic the best “starting line.” This aligns with our expert quote: “Protect timing and keep plans simple—quality improves when noise goes down.”
Questions to Ask Your Clinic
When you sit with your fertility clinic (or consider a second opinion), incorporate these questions:
- Does your standard fertility optimise vitamin D, HbA1c, and metabolic labs before stimulation?
- What vitamin D target level do you aim for before embryo transfer or stimulation?
- If HbA1c or insulin resistance is above your cutoff, do you recommend postponement or additional optimisation?
- What is the additional cost (labs + supplementation + review) and does it delay the cycle start?
- How do you incorporate metabolic findings into your stimulation protocol or transfer timing?
Expert Quote
“Protect timing and keep plans simple—quality improves when noise goes down.” — Clinical Team
This quote highlights that timing (i.e., when you test and optimise) and simplicity (don’t over-complicate with too many add-ons) matter for success in fertility diagnostics and treatment.
Patient Case Study
A couple in their mid-30s, their first fertility clinic visit after 12 months of trying. Female partner BMI 32, irregular cycles, male partner overweight with borderline dyslipidaemia.
Transfer proceeded, result: clinical pregnancy. Outcome Insight by aligning logistics (labs, supplementation, lifestyle) and clarifying expectations (costs, timeline, labs), the couple reported:
Testimonials
- “The steps finally made sense.” — A.&J., Manhattan
- “Costs were clear; no surprise bills.” — L., Hoboken
- “Nurses replied fast with practical coaching.” — K.&V., Queens
These highlight the value of transparency, structure and support when metabolic labs are integrated into fertility care.
Frequently Asked Questions (FAQs)
Q: Is this medical advice?
Ans: No—this article serves to help you guide your clinic conversations. Always consult your medical provider.
Q: How many cycles should I plan?
Ans: Think in ranges; cumulative success matters. Optimising labs ahead of fewer cycles may give you higher success per attempt.
Q: What drives cost most?
Ans: In fertility treatment, the big cost drivers are stimulation medications, genetic testing, advanced lab/embryo services, anaesthesia and the total number of cycles. The metabolic optimisation labs are a smaller proportion.
Additional Insights
- Lab quality indicators: Choosing a reputed lab for vitamin D and metabolic markers can de-risk your live-birth probability through transparent pricing and scenario planning.
- Recipient prep timelines (for embryo transfer cases) should align with metabolic optimisation: timing match matters between embryo readiness and endometrium health.
- Ovarian stimulation optimisation: If metabolic health is improved, the ovarian response tends to be more predictable, reducing volatility.
- Genetic testing decisions: Some clinics align lab cutoffs (e.g., insulin resistance) with embryo euploidy yield—if the body’s metabolic terrain is calmer, the embryo environment may be better.
- Trigger timing and add-on selection: While these are advanced steps, underlying metabolic health can influence responsiveness, so a better metabolic baseline may reduce the need for risky add-ons.
Conclusion
In the fertility testing & diagnostics pathway, integrating vitamin D, HbA1c, and broader metabolic labs is a valuable strategy to improve clarity, timing, and outcome potential. While they don’t guarantee success, they provide you and your clinic with actionable information that you can control (or improve) and thus reduce treatment “noise”. By understanding definitions, eligibility signals, timing checkpoints, cost realities, and outcome drivers, you place yourself in a stronger position to navigate fertility care. Ask your clinic the right questions, plan your labs and optimisation phase consciously, and treat metabolic health as an essential part of the fertility journey—not just an afterthought.

Dr. Kulsoom Baloch
Dr. Kulsoom Baloch is a dedicated donor coordinator at Egg Donors, leveraging her extensive background in medicine and public health. She holds an MBBS from Ziauddin University, Pakistan, and an MPH from Hofstra University, New York. With three years of clinical experience at prominent hospitals in Karachi, Pakistan, Dr. Baloch has honed her skills in patient care and medical research.