Male infertility accounts for nearly half of all fertility challenges faced by couples. Yet, it’s often overlooked or delayed in diagnosis. Understanding male factor triage — from semen analysis to TESE/mTESE — is critical to optimizing outcomes, reducing emotional strain, and improving IVF success rates. In NYC, where advanced fertility care is accessible but often costly, having a clear roadmap helps couples make informed, financially sound, and time-sensitive decisions.
This article walks you through the full journey: definitions, decision checkpoints, timing strategies, and transparent cost examples — all designed to simplify the fertility treatment pathway and align it with each couple’s goals.
1. Definitions and Where This Fits in the Journey
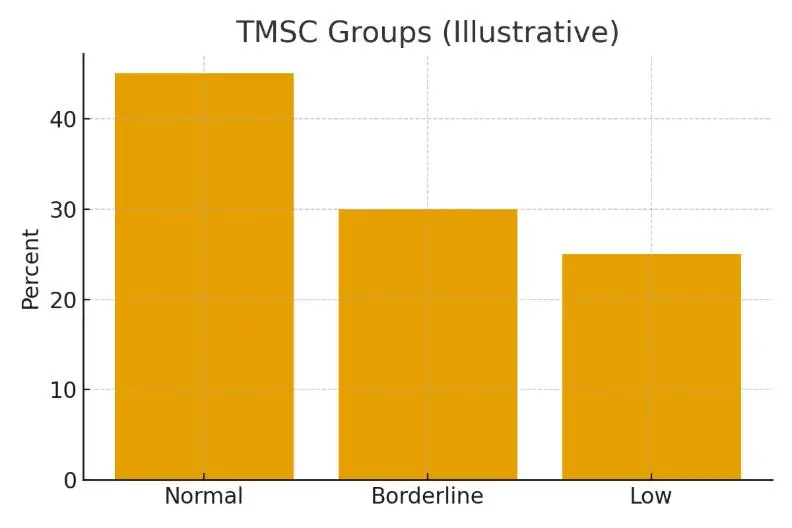
Semen analysis is the first diagnostic step for evaluating male fertility. It measures parameters like sperm count, motility, and morphology. If results are inconclusive or show severe male factor issues (such as azoospermia), additional tests — like hormone panels or genetic screenings — may follow.
When no sperm are present in the ejaculate, testicular sperm extraction (TESE) or micro-TESE (mTESE) may be recommended. These procedures retrieve sperm directly from testicular tissue for use in IVF with ICSI (intracytoplasmic sperm injection). The pathway is part of a broader fertility diagnostic process that determines the best route to conception, whether through IVF, IUI, or advanced surgical retrieval.
2. Eligibility Signals and When to Escalate
You may consider escalating to TESE/mTESE if:
- Repeated semen analyses show no or very low sperm count.
- Hormonal imbalances (FSH, LH, testosterone) suggest impaired sperm production.
- There’s a history of vasectomy, testicular trauma, or genetic causes (e.g., Y-chromosome microdeletions).
- Previous IVF or ICSI cycles failed due to poor fertilization rates.
Pausing or reassessing is appropriate when non-surgical factors — like lifestyle, medication, or timing of collection — might be reversible. Coordinating this stage with your fertility specialist ensures optimal timing and minimizes unnecessary procedures.
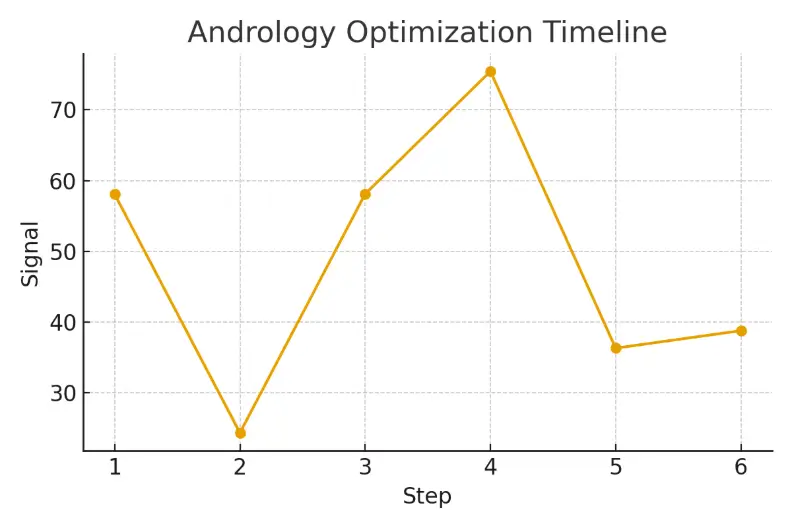
3. Step-by-Step with Timing Checkpoints
- Initial Evaluation: Semen analysis, hormone profile, and scrotal ultrasound.
- Follow-Up Testing: Repeat semen analysis after 2–3 months to confirm results.
- Genetic and Hormonal Workup: Identifies underlying causes affecting sperm quality or production.
- Surgical Retrieval (TESE/mTESE): Typically scheduled in coordination with your partner’s egg retrieval or cryopreservation cycle.
- IVF with ICSI: Retrieved sperm are injected into mature eggs to form embryos.
- Embryo Transfer or Freezing: Embryos may be transferred fresh or frozen, depending on uterine readiness and timing.
Staying aligned with your clinic’s cycle calendar is key — delays or mismatched timing can reduce embryo yield or implantation rates.
4. Pros, Cons, and Practical Costs
Pros:
- Enables biological parenthood even in severe male factor infertility.
- Allows use of fresh or frozen sperm in ICSI.
- It can improve diagnostic clarity by identifying sperm presence at the source.
Cons:
- Invasive and requires anesthesia.
- Not all procedures yield viable sperm.
- May add cost and recovery time.
Estimated Costs (NYC Range):
- Semen Analysis $100–$250
- Hormone & Genetic Testing $400–$1,200
- TESE/mTESE Procedure$4,000–$9,000
- IVF with ICSI$12,000–$18,000
- Medications$3,000–$7,000
Planning for these costs upfront, and understanding what’s included, prevents financial surprises and supports smoother decision-making in NYC.
5. Outcome Drivers You Control vs. Those You Monitor
You Control:
- Timing and coordination of testing.
- Lifestyle factors (nutrition, alcohol, stress, sleep).
- Communication with your clinic team.
You Monitor:
- Hormonal and genetic test results.
- Lab quality indicators (fertilization, blastocyst, and euploidy rates).
- Female partner’s ovarian response and uterine readiness.
As one fertility team put it:
“Protect timing and keep plans simple — quality improves when noise goes down.”
6. Questions to Ask Your Clinic
- How many TESE/mTESE procedures has your lab performed this year?
- What are your IVF success rates for male factor cases?
- How are retrieved sperm handled — fresh vs. frozen?
- What is the anesthesia protocol and recovery plan?
- Are all lab and medication costs disclosed before treatment?
Patient Case Study
A couple from NYC faced inconclusive semen analyses and uncertainty about their next step. Once they transitioned to a structured triage plan — repeat testing, clear communication, and coordinated TESE timing — they gained clarity and confidence. Their cycle produced healthy embryos, and their IVF journey became predictable, reducing stress and improving their overall experience.
Surrogacy & Male Factor Pathways in NYC
For couples who need advanced options beyond IVF, such as surrogacy combined with sperm retrieval, integrated services like Surrogacy4All provide comprehensive coordination. They connect patients with fertility clinics, labs, and legal teams to manage timing, logistics, and emotional support — ensuring the entire journey remains transparent and personalized.
Contact us today!
Frequently Asked Questions (FAQs)
Q: How does male factor infertility affect IVF success rates?
Ans: With ICSI, many male factor cases achieve comparable fertilization rates to standard IVF. The key is sperm quality and lab expertise.
Q: Is TESE or mTESE more effective?
Ans: TESE (microsurgical) often yields higher sperm retrieval rates in non-obstructive azoospermia, though it requires specialized expertise.
Q: How soon after TESE can IVF be scheduled?
Ans: In most NYC clinics, sperm can be used immediately (fresh) or frozen for later IVF cycles. Coordination ensures optimal timing.
Q: Are male fertility procedures covered by insurance?
Ans: Coverage varies by plan and state. Some NYC insurers cover diagnostics but not surgical retrieval or IVF. Always verify before starting.
Q: How can I compare fertility clinic success rates in NYC?
Ans: Review CDC or SART data for verified outcomes, focusing on live birth rates, male factor case volume, and patient satisfaction.

Dr. Kulsoom Baloch
Dr. Kulsoom Baloch is a dedicated donor coordinator at Egg Donors, leveraging her extensive background in medicine and public health. She holds an MBBS from Ziauddin University, Pakistan, and an MPH from Hofstra University, New York. With three years of clinical experience at prominent hospitals in Karachi, Pakistan, Dr. Baloch has honed her skills in patient care and medical research.