Endometriosis can be one of the most overlooked factors in the fertility journey. Within the Fertility Testing & Diagnostics pathway, knowing what shows up on tests—and what doesn’t—can change how quickly patients reach answers. This guide explains how to interpret endometriosis indicators, what to expect during testing, and how thoughtful timing, transparent costs, and a clear plan can improve outcomes for patients in NYC and beyond.
1. Where This Fits in the Fertility Journey
Endometriosis occurs when tissue similar to the uterine lining grows outside the uterus, often affecting the ovaries, fallopian tubes, or pelvic lining. For many, it’s discovered only after months or years of unexplained infertility.
Testing for endometriosis fits early in the diagnostic phase—ideally before starting IVF or other advanced reproductive treatments. By identifying underlying inflammation or structural issues first, clinics can personalize treatment and protect future success rates.
2. Eligibility Signals and When to Escalate
Common indicators include painful periods, pain during intercourse, pelvic pain outside of menstruation, and unexplained infertility.
If symptoms persist despite normal hormone or ultrasound results, escalation to imaging or minimally invasive evaluation (such as laparoscopy) may be warranted.
Pausing too long between inconclusive results can delay care, while rushing into IVF without addressing possible endometriosis can reduce implantation potential.
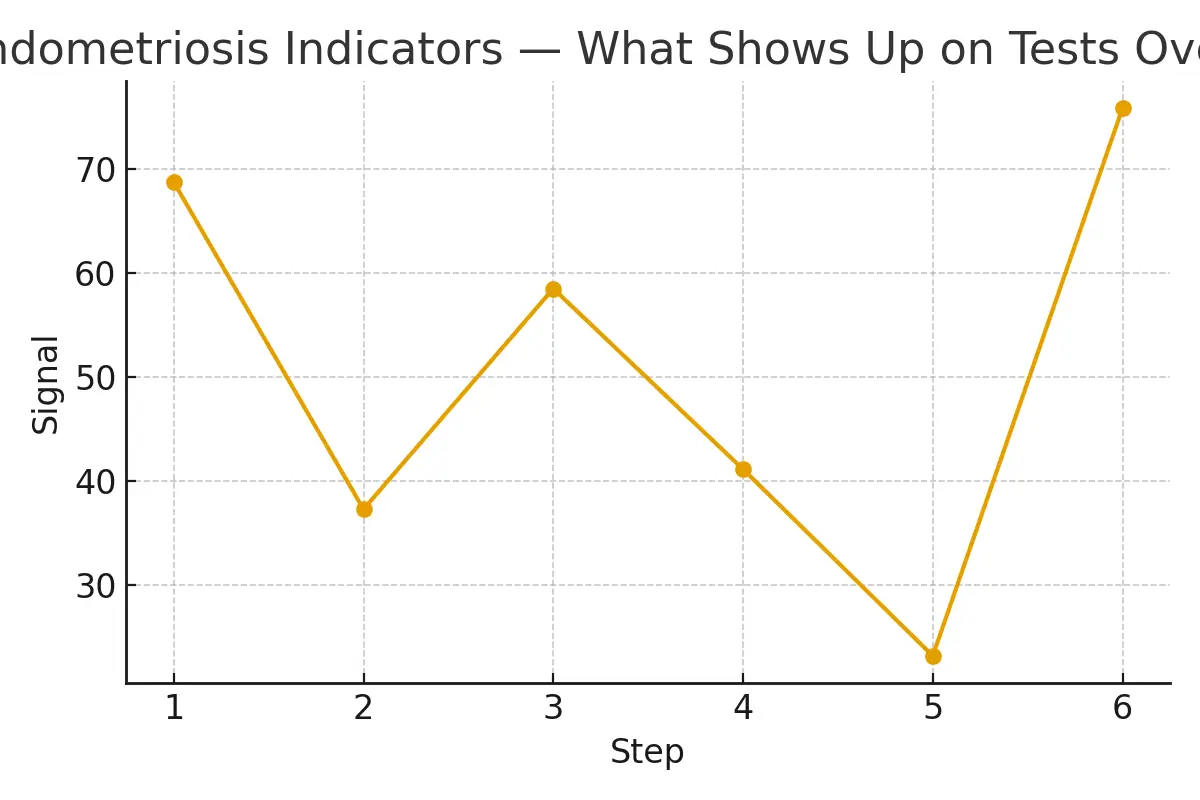
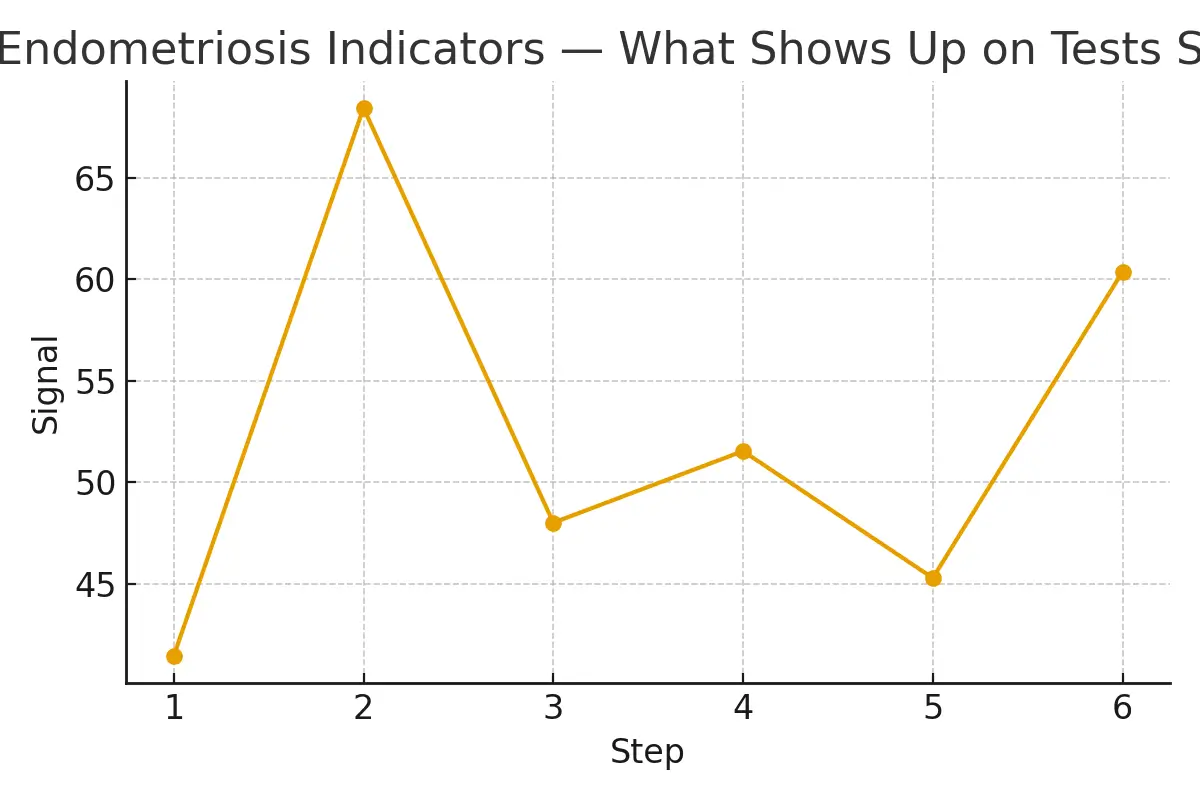
3. Step-by-Step: Timing and Checkpoints
- Baseline assessment: Hormone panel, ultrasound, and medical history.
- Advanced imaging: MRI or transvaginal ultrasound targeting possible endometrial lesions.
- Laparoscopy (if needed): Both diagnostic and therapeutic—can confirm and remove lesions.
- Recovery window: Typically one cycle to allow healing before fertility treatments.
- IVF planning: Integrating test findings to optimize ovarian stimulation and endometrial preparation.
Each step has timing checkpoints to balance accuracy with momentum—avoiding burnout while protecting emotional and financial resources.
4. Pros, Cons, and Practical Costs
Pros:
- Early identification improves treatment targeting and IVF outcomes.
- Reduces trial-and-error costs by clarifying causes of infertility.
- Enables more predictable timelines and emotional stability.
Cons:
- Some tests (especially laparoscopy) are invasive and costly.
- Insurance coverage varies widely across NYC clinics.
Example cost breakdown:
- Advanced ultrasound $300–$600
- MRI pelvic scan $800–$1,500
- Diagnostic laparoscopy $3,000–$10,00
- IVF cycle (if needed) $12,000–$20,000
Understanding costs upfront helps patients make realistic plans and reduces anxiety during treatment.
5. Outcome Drivers You Control vs. Those You Monitor
You control:
- Following the testing timeline and clinic recommendations
- Medication adherence
- Managing inflammation through diet, sleep, and stress reduction
You monitor:
- Hormone response
- Ovarian reserve
- Endometrial receptivity
- Embryo quality and implantation rates
Aligning these factors can make the difference between a drawn-out process and a smoother, more predictable patient journey.
6. Questions to Ask Your Clinic
- How do you screen for endometriosis before IVF?
- What’s your lab’s success rate with patients who have endometriosis?
- Which tests are essential versus optional?
- What’s covered by insurance, and what’s the out-of-pocket range?
- How do you coordinate timing between ovarian stimulation and endometrial preparation?
Expert Insight
“Protect timing and keep plans simple—quality improves when noise goes down.” — Clinical Team
Patient Story
A couple in Manhattan spent months cycling through inconclusive fertility tests. Once their care team identified subtle endometriosis indicators through advanced imaging, they shifted to a more direct treatment plan. The result: improved predictability, controlled costs in NYC, and higher confidence in each IVF step.
Real Testimonials
“The steps finally made sense.” — A.&J., Manhattan
“Costs were clear; no surprise bills.” — L., Hoboken
“Nurses replied fast with practical coaching.” — K.&V., Queens
Next Steps with Surrogacy4all NYC
- Free 15-minute nurse consult
- Upload labs for a second opinion
- Get a personalized cost breakdown
Endometrial preparation, ovarian stimulation, and pharmacy logistics all work together to make care more predictable. By aligning timing, managing expectations, and focusing on clarity, patients can reduce variability and improve outcomes. For compassionate, evidence-based fertility support in NYC, visit our website to explore customized plans designed around your journey.
Frequently Asked Questions (FAQs)
Q: Does endometriosis lower IVF success rates?
Ans. It can, especially if untreated, but success rates improve when lesions are managed before stimulation or transfer.
Q: How do fertility clinics in NYC test for endometriosis?
Ans. Through a mix of ultrasounds, MRIs, and, if needed, diagnostic laparoscopy for confirmation and removal.
Q: What affects IVF costs the most?
Ans. Medications, anesthesia, genetic testing, and the total number of cycles required.
Q: Can I do fertility testing without starting IVF?
Ans. Yes—diagnostic testing helps clarify your fertility status and may prevent unnecessary IVF cycles.
Q: How can I plan my fertility journey in NYC?
Ans. Start with a full diagnostic panel, clarify clinic communication, and plan financially using transparent cost breakdowns.

Dr. Kulsoom Baloch
Dr. Kulsoom Baloch is a dedicated donor coordinator at Egg Donors, leveraging her extensive background in medicine and public health. She holds an MBBS from Ziauddin University, Pakistan, and an MPH from Hofstra University, New York. With three years of clinical experience at prominent hospitals in Karachi, Pakistan, Dr. Baloch has honed her skills in patient care and medical research.





