When it comes to understanding fertility and planning your IVF journey in NYC, few tools are as insightful as the Antral Follicle Count (AFC). This simple ultrasound measurement offers critical clues about ovarian reserve, timing, and treatment planning — helping couples move from uncertainty to clarity.
In this guide, we’ll explain what AFC is, who benefits from it, how timing influences outcomes, what realistic costs look like, and how to simplify your fertility pathway with confidence.
Understanding Antral Follicle Count (AFC)
What Is AFC and Why It Matters in Fertility Testing
Antral Follicle Count (AFC) refers to the number of small, fluid-filled sacs (follicles) visible on a woman’s ovaries during a transvaginal ultrasound. These follicles contain immature eggs, which represent a woman’s short-term ovarian potential.
In fertility and IVF planning, AFC is one of the most reliable indicators of ovarian reserve — showing how many eggs may respond to stimulation during a treatment cycle.
When paired with AMH (Anti-Müllerian Hormone) testing, AFC helps fertility specialists in NYC tailor IVF protocols, predict medication dosage, and estimate success rates before treatment even begins.
Where AFC Fits in the Fertility Journey
AFC testing typically occurs early in your fertility assessment — right after initial consultations and before starting stimulation medications. It fits between diagnostic steps such as:
- Hormone bloodwork (AMH, FSH, LH, Estradiol)
- Baseline ultrasound scans
- Semen analysis for male partners
This early testing phase allows your clinic to build a personalized fertility roadmap and decide whether IVF, IUI, or egg freezing is the most effective next step.
Eligibility Signals — When to Escalate or Pause
Not everyone needs to jump straight to IVF after one test. Here’s how to interpret common scenarios based on AFC results:
High AFC (More than 15 follicles)
- Indicates a good ovarian reserve.
- Common among younger women or those with PCOS.
- IVF stimulation must be carefully balanced to prevent hyper-response.
Averge AFC (8–15 follicles)
- Suggests a typical ovarian response.
- Most IVF patients in NYC fall in this category.
- Offers balanced chances of success with standard protocols.
Low AFC (Below 8 follicles)
- Indicates lower ovarian reserve.
- IVF may still succeed with adjusted stimulation or use of donor eggs.
- Early testing helps avoid wasted cycles and unexpected costs.
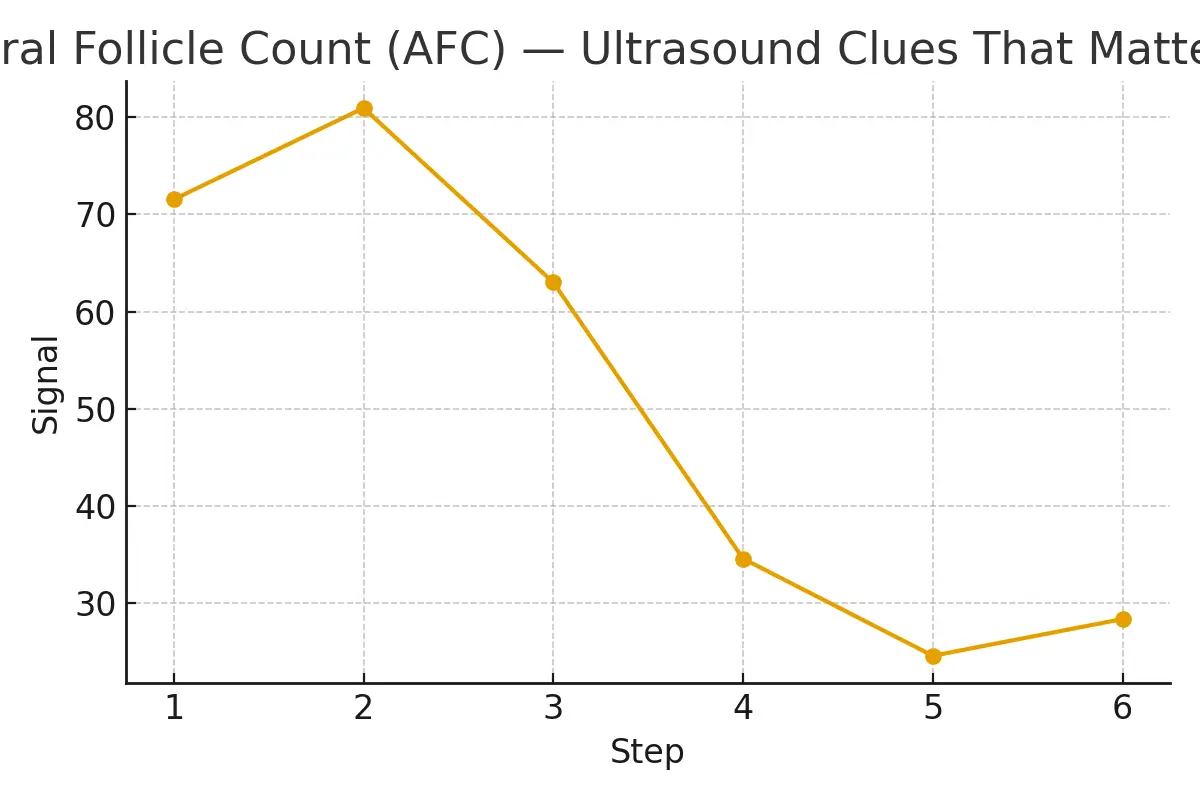
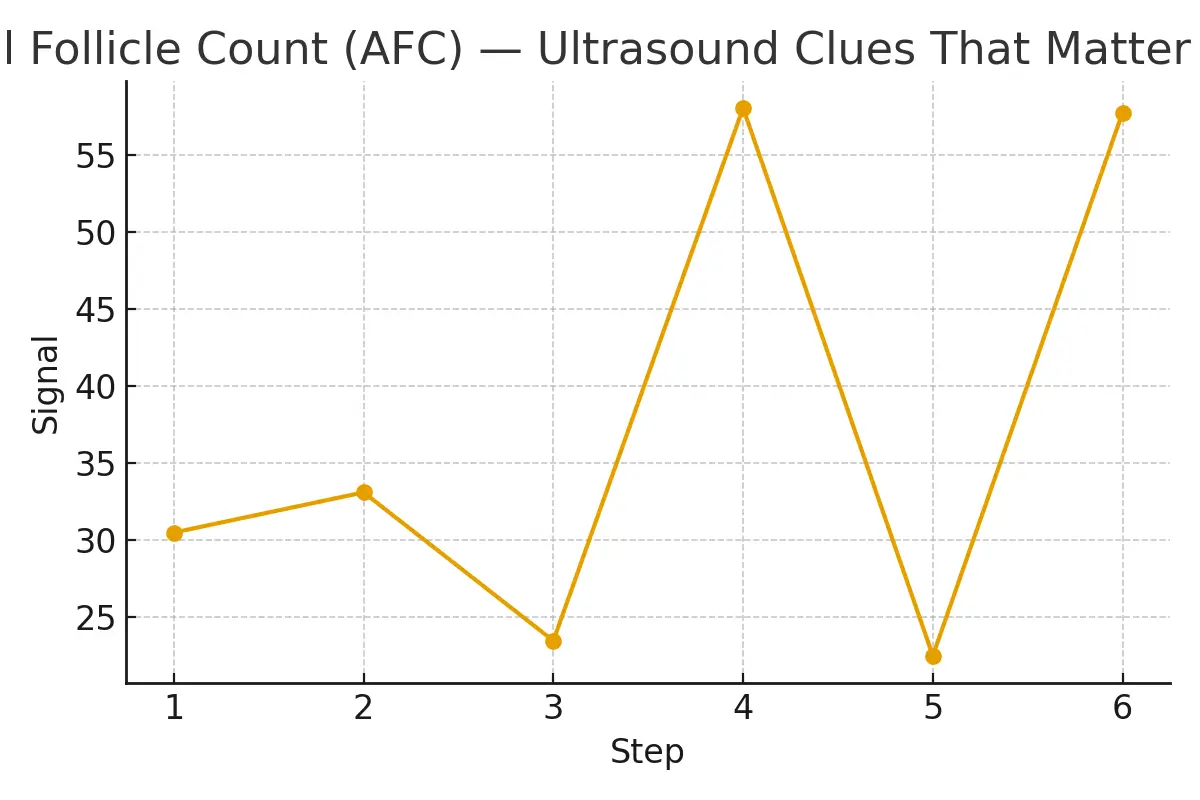
Step-by-Step: AFC and Timing Checkpoints
Timing is everything in fertility. Here’s a clear roadmap of when and how AFC fits into your IVF journey:
Step 1: Baseline Ultrasound (Day 2–4 of Cycle)
Performed early in your menstrual cycle to count resting follicles before stimulation begins.
Step 2: AMH Blood Test and Review
Often done concurrently to cross-verify ovarian reserve.
Step 3: Personalized Stimulation Plan
Fertility specialists adjust IVF medication doses based on AFC readings.
Step 4: Mid-Cycle Monitoring
Ongoing ultrasounds ensure follicles grow at the right rate for retrieval.
Step 5: Egg Retrieval and Fertilization
The final step where timing and AFC directly influence IVF success rates and embryo quality.
Pros, Cons, and Practical Costs
Advantages of AFC Testing
- Non-invasive and affordable — usually included in early fertility consults.
- Predictive power — helps optimize medication doses and prevent overstimulation.
- Better planning — minimizes uncertainty before IVF.
Potential Limitations
- AFC alone doesn’t predict egg quality — age and hormone levels still matter.
- Follicle counts can vary slightly from cycle to cycle.
Cost Breakdown
In NYC, fertility testing packages typically range from $300 to $700, depending on clinic fees and ultrasound technology. When part of a full IVF cycle, AFC testing may be included in bundled costs (often $12,000 to $18,000 per cycle).
Key Cost Drivers:
- Stimulation medications
- Genetic testing (PGT)
- Anesthesia and retrieval procedure
- Cryopreservation and storage fees
Outcome Drivers — What You Control vs. What You Monitor
You Control:
- Lifestyle and nutrition: Balanced diet, exercise, and sleep directly affect egg quality.
- Timing and adherence: Following your treatment schedule precisely improves outcomes.
- Stress management: Mental well-being has measurable effects on hormonal balance.
You Monitor:
- AFC and AMH levels: Indicators of ovarian reserve and responsiveness.
- Embryo growth patterns: Reflect lab quality and stimulation precision.
- Implantation rates: Help fine-tune future IVF cycles.
Questions to Ask Your Clinic
- How do my AFC and AMH results compare to the average for my age group?
- How will these numbers influence my IVF medication plan?
- What are the clinic’s IVF success rates for patients with similar AFC results?
- Are there ways to improve ovarian response before treatment?
- What are my financing or insurance coverage options for testing and IVF?
Expert Insight
“Protect timing and keep plans simple — quality improves when noise goes down.”
— Clinical Team, Surrogacy4All NYC
Fertility care works best when information is clear and decisions are consistent. Simplicity in timing, testing, and treatment sequencing leads to more predictable outcomes.
Patient Case Study
A couple in Manhattan struggled with inconclusive fertility tests for months. After scheduling an AFC ultrasound, they discovered a lower-than-expected ovarian reserve but used that insight to fast-track their IVF plan.
By aligning test timing, medication dosing, and financial expectations, they achieved a more predictable treatment journey — and a healthy pregnancy within three months of starting IVF at their NYC clinic.
Testimonials
“The steps finally made sense.” — A. & J., Manhattan
“Costs were clear; no surprise bills.” — L., Hoboken
“Nurses replied fast with practical coaching.” — K. & V., Queens
Next Steps with Surrogacy4All NYC
If you’re beginning your fertility journey or planning for IVF in NYC, understanding your Antral Follicle Count (AFC) is a crucial first step. At Surrogacy4All, we offer personalized fertility testing, expert consultations, and transparent cost breakdowns — helping you make confident, informed decisions.
Take the next step today:
- Schedule a free 15-minute nurse consult
- Upload your lab reports for a second opinion
- Get a detailed IVF cost estimate for your case
Start your journey toward clarity, confidence, and success with Surrogacy4All NYC — where science meets compassion.
Frequently Asked Questions (FAQs)
Q. What is the role of AFC in IVF success rates?
Ans. A higher AFC often correlates with a stronger ovarian response and increased embryo numbers, improving IVF success rates.
Q. How much does IVF cost in NYC?
Ans. On average, one IVF cycle in NYC costs between $12,000–$18,000, excluding medications and genetic testing.
Q. Can lifestyle changes improve fertility before IVF?
Ans. Yes. Balanced nutrition, adequate sleep, reduced stress, and quitting smoking can all positively influence fertility outcomes.
Q. How long does the fertility testing phase take?
Ans. Most fertility assessments, including AFC, AMH, and semen analysis, are completed within 2–3 weeks before treatment planning begins.
Q. Why choose Surrogacy4All for IVF and fertility care in NYC?
Ans. Surrogacy4All combines advanced IVF technology, transparent pricing, and compassionate support to guide every step of your patient journey.

Dr. Kulsoom Baloch
Dr. Kulsoom Baloch is a dedicated donor coordinator at Egg Donors, leveraging her extensive background in medicine and public health. She holds an MBBS from Ziauddin University, Pakistan, and an MPH from Hofstra University, New York. With three years of clinical experience at prominent hospitals in Karachi, Pakistan, Dr. Baloch has honed her skills in patient care and medical research.