When fertility testing reveals diminished ovarian reserve (DOR), the path forward can feel uncertain. Understanding how to build the right lab picture helps patients and clinicians make informed, timely choices — optimizing outcomes while minimizing emotional and financial strain. This guide explores how DOR fits into the fertility journey, how testing works, what realistic IVF success rates look like, and how patients in NYC can plan smarter around costs and care.
1. Understanding Diminished Ovarian Reserve
Diminished ovarian reserve means the quantity or quality of a woman’s remaining eggs is lower than expected for her age. It doesn’t necessarily mean pregnancy is impossible — but it signals that time, lab precision, and treatment sequence matter more than ever.
This condition is typically identified through fertility testing and diagnostics, including:
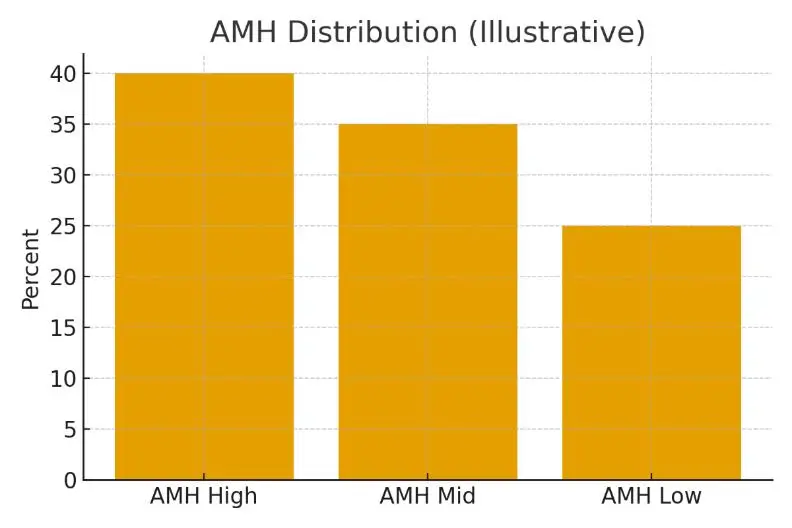
- AMH (Anti-Müllerian Hormone): Indicates the size of the remaining egg pool.
- FSH (Follicle-Stimulating Hormone): Higher levels suggest the ovaries are working harder to mature eggs.
- Antral Follicle Count (AFC): A simple ultrasound count showing how many follicles are visible in the ovaries.
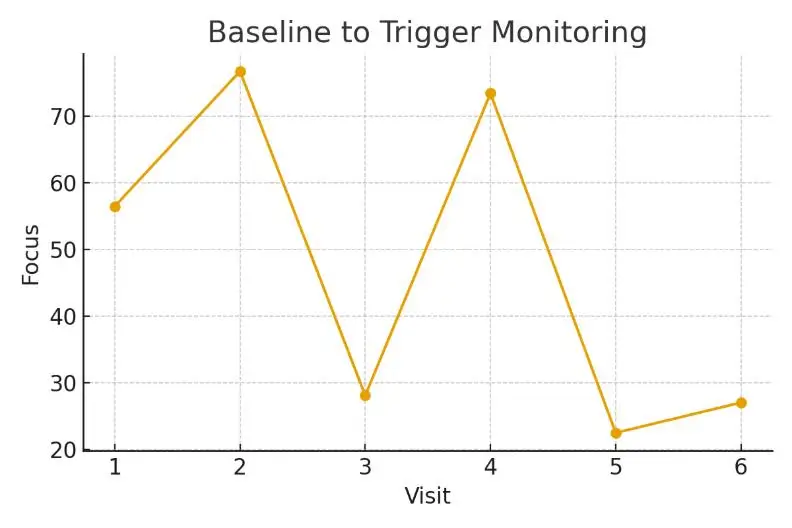
Building the right lab picture means combining these data points into a coherent plan — not reacting to a single number. It’s about seeing the trend over time, not just the result from one month.
2. Who Benefits from Early Testing
Early testing benefits women over 32, those with irregular cycles, or anyone with a family history of early menopause. It also supports couples beginning IVF or egg freezing in NYC, helping to set realistic expectations about success rates and timelines.
Eligibility signals to begin evaluation include:
- Periods becoming shorter or irregular
- Prior ovarian surgery or endometriosis
- Low AMH or elevated FSH
- Poor response to stimulation in past IVF cycles
Knowing when to escalate or pause testing can save both money and emotional energy. Sometimes, repeating a lab test after a recovery cycle can offer clearer data.
3. Step-by-Step Testing and Timing
The right testing sequence builds around your menstrual cycle:
- Day 2-3: FSH, LH, Estradiol, and AMH draw
- Day 8-12: Ultrasound for antral follicle count and uterine lining
- Mid-cycle: Ovulation check, optional progesterone test
- Post-cycle: Review with your clinician to define next steps
For IVF patients, these checkpoints align treatment timing, medication dosing, and lab scheduling to maximize egg quality. Consistency in test timing reduces variability, which can significantly affect success rates.
4. Realistic Costs and Line-Item Examples
Fertility care in NYC can vary widely, but transparency helps patients plan. Typical IVF with diminished ovarian reserve may include:
- Initial fertility consult $250–$500
- Hormone and ovarian reserve testing $400–$800
- IVF cycle (base package) $10,000–$15,000
- Medications $3,000–$7,000
- Genetic testing (PGT-A) $2,000–$4,000
- Anesthesia & retrieval fees $1,000–$2,000
Total estimate: $16,000–$28,000 per cycle (varies by clinic and protocol).
Patients Medical NYC helps patients understand what each cost means — separating medical necessity from optional add-ons, so care remains humane and predictable.
5. Controlling What You Can
Certain outcome drivers are within your control, while others are purely biological.
You can control:
- Lifestyle factors (sleep, nutrition, stress management)
- Lab timing and adherence to medication schedules
- Selection of experienced fertility teams
You monitor:
- Egg response to stimulation
- Embryo quality and genetic results
- Endometrial receptivity
- Expert advice remains simple:
“Protect timing and keep plans simple—quality improves when noise goes down.” — Clinical Team, Patients Medical NYC.
6. Real Patient Journey
A Manhattan couple came to the clinic after multiple inconclusive tests. Their care team repeated AMH and AFC tests using consistent timing, revealing a mild diminished reserve rather than a severe decline. By aligning logistics, expectations, and costs, they improved both predictability and emotional balance — and achieved pregnancy within two cycles.
Patients often say that once the steps were explained clearly, the process felt less overwhelming and more empowering.
7. Questions to Ask Your Clinic
- How do you confirm diminished ovarian reserve before recommending IVF?
- What lab values guide protocol changes?
- How do you handle medication dosing for low responders?
- What are your cumulative IVF success rates for my age group?
- How can I plan financially for multiple cycles?
Being proactive turns uncertainty into clarity — and helps patients focus on what truly matters: timing, trust, and transparency.
Next Steps with Patients Medical NYC
If you’re navigating fertility testing or IVF in NYC, Patients Medical NYC offers a free 15-minute nurse consultation, lab upload review, and a custom cost breakdown for your case. Understanding diminished ovarian reserve isn’t about chasing numbers — it’s about building a clear, evidence-based picture that supports your next decision.
For patients exploring advanced options such as egg donation or gestational surrogacy, our partner network Surrogacy4All provides seamless coordination and transparent cost structures to keep your family-building journey on track. Contact us today!
Frequently Asked Questions (FAQs)
Q: Can IVF work with diminished ovarian reserve?
Ans. Yes. IVF success rates depend on age, egg quality, and protocol customization. Many patients with DOR conceive using tailored stimulation or donor options.
Q: How long should I try before considering IVF?
Ans. If you’re under 35, consider testing after 12 months; over 35, after 6 months. DOR may shorten this window.
Q: Does IVF cost more in NYC?
Ans. Typically, yes — due to higher overhead and advanced lab infrastructure. However, transparent pricing and cycle bundling can manage total costs.
Q: What affects IVF success rates the most?
Ans. Age, embryo genetics, lab precision, and uterine health are key factors. Managing stress and optimizing timing also play measurable roles.
Q: Is surrogacy an option if ovarian reserve is very low?
Ans. Absolutely. When egg quality or response is limited, surrogacy with donor eggs — through programs like Surrogacy4All — can significantly increase live-birth success.

Dr. Kulsoom Baloch
Dr. Kulsoom Baloch is a dedicated donor coordinator at Egg Donors, leveraging her extensive background in medicine and public health. She holds an MBBS from Ziauddin University, Pakistan, and an MPH from Hofstra University, New York. With three years of clinical experience at prominent hospitals in Karachi, Pakistan, Dr. Baloch has honed her skills in patient care and medical research.