Ethical questions in donor conception arise because decisions made early—such as whether a donor remains anonymous, whether a child will have the right to future contact, and how much medical and genetic information is shared—affect families for decades.
- Autonomy means respecting the choices of donors, parents, and eventually the child born from donation.
- Privacy involves how much identifying information is shared or protected at different stages.
- Future contact deals with whether a donor or donor-conceived child may reach out later in life.
These choices are not only personal but also influenced by clinic policies, legal frameworks, and cultural expectations.
Who It Helps
This guidance is most useful for:
- Parents considering donor conception who want clarity before treatment.
- Donors who seek to understand their rights and obligations.
- Children and families who will live with the outcomes of these choices.
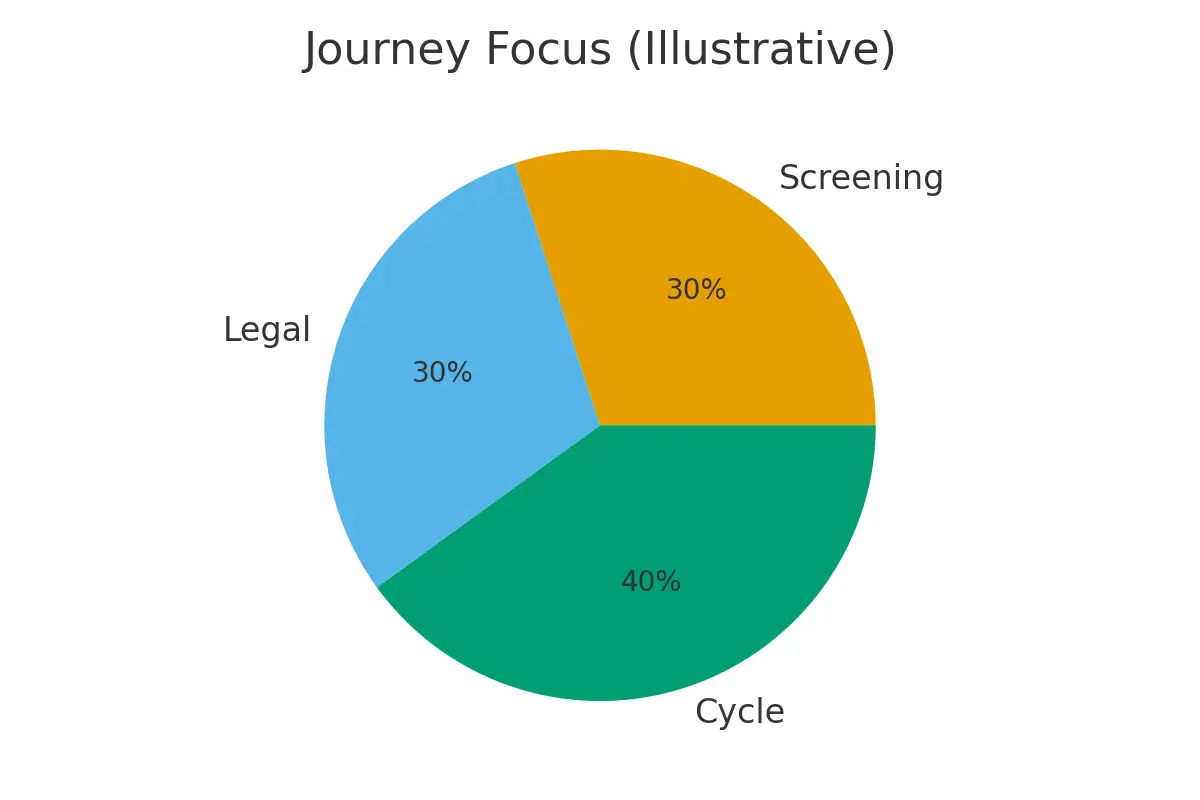
Signals that suggest a good fit for one donor pathway over another include medical history, lab results, age, imaging, and response to treatment. For example, families choosing embryos may face different privacy and contact considerations than those using sperm or eggs.
Step-by-Step:
A structured approach helps reduce stress and avoid surprises:
- Consent & Legal Steps – Define autonomy and privacy clearly in contracts. Decide whether donation is anonymous, open, or identity-release.
- Clinic Calendar & Logistics – Align medical steps like ovarian stimulation, oocyte retrieval, and embryo culture with family values.
- Transparency in Communication – Keep records and ensure consistency in how donor conception is described to children.
- Future Contact Checkpoints – Establish clear agreements about when and how donor-conceived children may reach out.
- Review & Update – Revisit agreements as laws, technologies, or family needs evolve.
Pros & Cons
Pros:
- Protects the child’s right to identity and family history.
- Gives donors clarity on their role and boundaries.
- Reduces future conflict by setting clear expectations.
Cons / Trade-offs:
- Too much privacy may prevent children from accessing important genetic history.
- Open-identity donations can create emotional complexity for families.
- Legal variations across countries complicate international donor use.
A balanced approach considers the values of all parties while protecting long-term outcomes.
Costs & Logistics
Ethical choices carry hidden costs:
- Legal contracts: $500–$3,000 depending on complexity.
- Counseling sessions: $150–$250 each for donor and intended parents.
- Travel & coordination: International donation may require visas, storage fees, and shipping logistics.
- Insurance & authorizations: Delays or denials may impact embryo competency and cycle predictability.
Simple tracking—such as budgeting for pharmacy logistics, frozen embryo transfer timing, and luteal support—prevents surprise bills and cycle cancellations.
What Improves Outcomes
Certain actions make a measurable difference:
- Endometrial preparation: Optimizes implantation odds by aligning embryo transfer with uterine readiness.
- Oocyte retrieval & lab quality: Reduces variability and increases the chance of healthy embryos.
- Single-embryo transfer policies: Minimize multiples risk while protecting maternal health.
- Male-factor optimization: Improves cumulative success with targeted supplements and counseling.
- Cycle cancellation criteria: Protect budgets and patient experience by setting clear thresholds.
What rarely changes outcomes? Add-ons without evidence, delaying disclosure, or assuming privacy agreements never evolve.
Case Study
A couple in their late 30s chose embryo donation overseas. Their primary concern was privacy; they wanted to limit identifying information. With guidance, they signed an agreement allowing anonymous donation but with optional medical updates. Later, their child asked questions about genetic history. Because they had planned ahead, the family accessed non-identifying donor health updates, balancing privacy with the child’s autonomy. The steady communication and clear thresholds prevented conflict and financial surprises.
Mistakes to Avoid
- Avoiding the topic: Not discussing privacy or future contact until after treatment leaves families unprepared.
- Relying on verbal promises: Always secure agreements in writing.
- Assuming anonymity is permanent: DNA testing and social media make total anonymity nearly impossible.
- Neglecting logistics: Ignoring pharmacy coordination, travel planning, or insurance approvals can derail a cycle.
FAQs
Q. What is the difference between anonymous, open, and identity-release donation?
Ans. Anonymous means no identifying details are shared. Open donation allows contact from the beginning. Identity-release means the donor’s identity may be revealed to the child at a set age (often 18).
Q. How does donor privacy affect children later in life?
Ans. Children may want genetic or medical history for identity, health, or family reasons. Too much privacy may limit access, while openness supports autonomy.
Q. What if laws in my country differ from the donor’s country?
Ans. International donations may follow the donor’s country laws, not the parents’. Always seek legal advice before cross-border arrangements.
Q. Can agreements about future contact change later?
Ans. Yes. While contracts provide structure, circumstances and technologies (like DNA testing) may evolve. Ongoing dialogue and legal updates are recommended.
Q. Does considering ethics slow down treatment timelines?
Ans. Not necessarily. Addressing autonomy, privacy, and contact early often streamlines the process by reducing future disputes or cycle cancellations.
Schedule a free 15-minute nurse consult, upload your labs, and receive a personalized cost breakdown. By aligning ethical decisions with medical planning, you safeguard both family trust and treatment success.
Next Steps
- Free 15‑min nurse consult
- Upload labs
- Cost breakdown for your case.
Related Links

Dr. Kulsoom Baloch
Dr. Kulsoom Baloch is a dedicated donor coordinator at Egg Donors, leveraging her extensive background in medicine and public health. She holds an MBBS from Ziauddin University, Pakistan, and an MPH from Hofstra University, New York. With three years of clinical experience at prominent hospitals in Karachi, Pakistan, Dr. Baloch has honed her skills in patient care and medical research.





