These three factors work together to predict your response to stimulation:
-
AMH (Anti-Müllerian Hormone):
A hormone made by small follicles. Higher AMH → usually more eggs grow during a cycle. -
AFC (Antral Follicle Count):
The ultrasound count of small resting follicles (2–10mm). AFC is a direct snapshot of the ovaries and one of the strongest predictors of egg yield. -
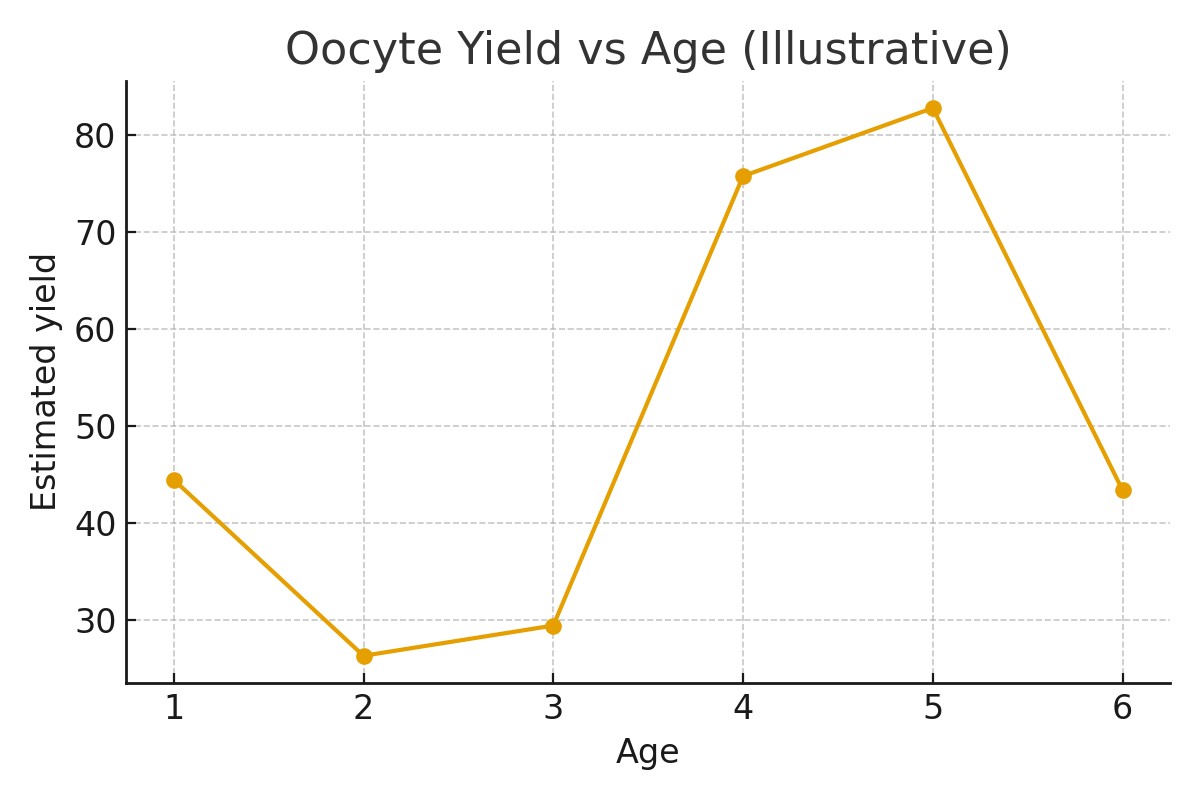
Age:
The most important factor for egg quality and chromosomal normality, which influences the number of future embryos and potential live births.
Together, these measurements shape the expected egg yield per cycle and drive all downstream decisions: protocol type, medication dosing, cycle number planning, cost estimates, and realistic expectations.
Upstream decisions—accurate testing, timing, lab review, communication, and medication preparation—directly affect downstream results such as egg maturity and final usable egg counts.
Who It Helps
Signals that AMH + AFC testing is a good fit
- Planning egg freezing between ages 28–42
- Irregular cycles or unknown ovarian reserve
- Concern about future fertility or age-related decline
- Family history of early menopause
- Preparing for cancer treatment or ovary-impacting surgery
- Wanting a clear estimate of egg yield before spending money
When to consider a different or additional path
-
Very low AMH (<0.5 ng/mL) or AFC <5:
May require multiple cycles or considering embryo creation instead. -
Age 41+:
Egg count may be adequate, but egg quality declines sharply; embryos may offer more predictive clarity. -
Polycystic Ovary Syndrome (PCOS):
High AFC and high AMH but risk of overstimulation — requires careful protocol. -
Urgent timelines:
May need random-start or dual stimulation cycles.
Step-by-Step
A simple, predictable sequence with timing checkpoints to protect egg quality and reduce stress:
1. Baseline Testing (Week 0–1)
- AMH blood work
- Transvaginal ultrasound for AFC
- Review of cycle history, age, and medical background
Checkpoint: Predict expected egg yield range (e.g., “10–14 eggs per cycle”).
2. Individualized Plan (Week 1–2)
- Determine stimulation protocol based on AMH/AFC/age
- Estimate number of cycles needed to reach your egg goal
- Build cost and timeline plan
Checkpoint: Confirm whether targets are realistic for your age.
3. Medication & Logistics Prep (Week 2–3)
- Ordering fertility medications
- Insurance authorizations
- Injection teaching
Checkpoint: No medication gaps or surprise bills mid-cycle.
4. Ovarian Stimulation (10–12 Days)
- Daily injections to grow follicles
- Monitoring every 2–3 days to measure growth and estradiol levels
Checkpoint: Are follicles responding at the expected rate for your AMH/AFC?
5. Trigger Shot & Retrieval
- Trigger injection 34–36 hours before retrieval
- Eggs collected under light anesthesia
- Mature eggs (MII) counted and frozen
Checkpoint: Compare retrieved mature eggs with predicted range.
6. Post-Cycle Review
- Assess maturity rate
- Decide if another cycle is needed
- Discuss future planning and storage
Pros & Cons
Pros
- Highly accurate for predicting egg yield
- Helps build clear, personalized egg-number goals
- Improves budgeting and timeline planning
- Avoids over- or under-stimulation with the right protocol
- Reduces emotional guesswork
Cons / Trade-Offs
- AMH and AFC predict quantity, not quality
- High AMH (e.g., PCOS) increases OHSS risk
- Low AMH can lead to multiple cycles
- Numbers fluctuate slightly cycle-to-cycle
- Emotional stress if yield is lower than expected
Risks
- Misinterpreting AMH as a fertility score (it’s not)
- Relying on AMH alone without AFC
- Delaying egg freezing too long based on “normal” AMH levels
Costs & Logistics
Understanding your AMH and AFC helps predict:
Line Items
- Diagnostic testing (AMH, AFC)
- Monitoring and retrieval
- Medication costs (higher with low AMH)
- Lab, freezing, and storage fees
Prior Authorizations
- Baseline labs may be partially covered
- Cancer-related preservation often fully covered
- Medication grant programs available
Cash-Flow Scenarios
- Cycle packages vs pay-per-cycle
- Med financing options
- Expect 30–60% of cost tied to medications
Avoid Surprise Bills
- Request an itemized cost sheet
- Understand what’s “included” vs billed separately
- Track medication usage to avoid emergency refills
What Improves Outcomes
Actions that actually help:
- Testing AMH + AFC together, not separately
- Using age-specific egg-number targets
- Selecting protocol based on ovarian reserve
- Ensuring precise trigger timing
- Avoiding overstimulation in high AMH (PCOS)
Actions that rarely change results:
- Taking supplements without evidence
- Excessive monitoring without indication
- Changing diet mid-cycle
- Relying on “symptoms” instead of hormone levels
Case Study
A 33-year-old with AMH 2.8 ng/mL and AFC 17 wanted to understand how many eggs she might get.
Her predicted yield was 14–18 eggs per cycle.
During stimulation:
- Day 5: 9 follicles >10mm
- Day 8: 14 follicles growing in sync
- Triggered on Day 10
- Retrieval: 17 eggs, 14 mature
With clear communication and predefined thresholds, she achieved her goal in one cycle and avoided unnecessary extra treatment.
Mistakes to Avoid
- Treating AMH as a “fertility score”
- Using AMH without AFC — or vice versa
- Assuming high AMH = high-quality eggs
- Ignoring age; quality matters as much as quantity
- Starting stimulation without full medication supply
- Not checking maturity rate (MII count) after retrieval
- Failing to plan for possible second cycles
FAQs
Q. Is AMH the most important fertility test?
Ans : It predicts egg quantity, but age predicts egg quality.
Q. Can AFC change month to month?
Ans : Yes, by 10–20%. It’s normal.
Q. Do high AMH levels guarantee a better egg yield?
Ans : Generally yes, but quality still depends on age.
Q. Is low AMH the same as infertility?
Ans : No. It just reflects reduced ovarian reserve.
Q. What’s more accurate—AMH or AFC?
Ans : They are best interpreted together.
Q. Can I freeze eggs with low AMH?
Ans : Yes, but planning multiple cycles may be realistic.
Next Steps
- Free 15-min nurse consult
- Upload your labs
- Personalized egg-yield and cost breakdown for your case
Related Links
- Egg Freezing Preservation
- Intended Parents
- Become a Surrogate
- Fixed‑Cost Packages
- Upload Labs
- Locations (NYC)
- SART
- CDC ART
- ASRM

Dr. Kulsoom Baloch
Dr. Kulsoom Baloch is a dedicated donor coordinator at Egg Donors, leveraging her extensive background in medicine and public health. She holds an MBBS from Ziauddin University, Pakistan, and an MPH from Hofstra University, New York. With three years of clinical experience at prominent hospitals in Karachi, Pakistan, Dr. Baloch has honed her skills in patient care and medical research.





