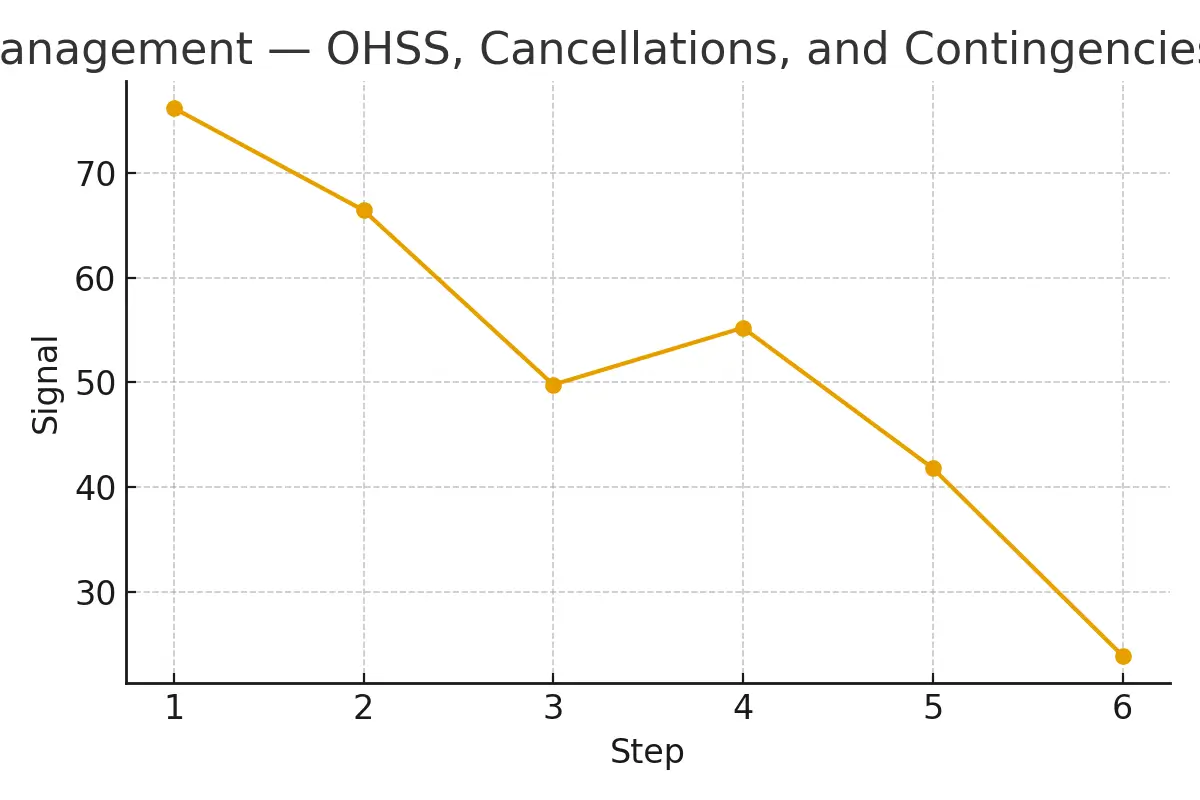
Managing risks such as OHSS (Ovarian Hyperstimulation Syndrome), cycle cancellations, and treatment contingencies is one of the most important—yet least understood—parts of the donor egg journey. This guide breaks everything down into simple, human-friendly language so intended parents, donors, and care teams can stay informed, aligned, and calm throughout the cycle.
You’ll learn what to expect, how decisions are made, what costs look like, and how timing affects outcomes. Everything here is written to help you prepare better questions, avoid unnecessary stress, and maintain clarity at every checkpoint.
What Risk Management Really Means in the Egg Donation Journey
Risk management in fertility care refers to monitoring, predicting, and preventing complications during a donor or IVF cycle. The three key areas include:
What Is OHSS?
OHSS (Ovarian Hyperstimulation Syndrome) is a medical reaction where a patient (usually a donor) responds too strongly to fertility medications. Symptoms range from bloating and discomfort to severe fluid shifts requiring medical care.
What Are Cycle Cancellations?
A cycle cancellation occurs when treatment is paused or stopped because continuing might compromise safety or success. Reasons include poor response, overly strong response, logistical problems, or unexpected medical findings.
What Are Contingencies?
Contingencies are backup plans, including timing adjustments, medication changes, retrieval day shifts, financial safeguards, or alternative cycle strategies.
This risk-management layer fits into the middle of the Egg Donation 101 pathway, usually between ovarian stimulation and retrieval.
Eligibility Signals: When to Continue, Pause, or Escalate Care
Understanding eligibility signals keeps expectations realistic and protects outcomes.
Signals That It’s Safe to Continue
- Stable estrogen (E2) rise
- Consistent follicle growth (1–3 mm/day)
- No symptoms of OHSS
- Donor hydration and comfort stable
- Ultrasound showing synchronized follicle cohort
Signals to Pause or Adjust
- Rapid estrogen jump
- Too many follicles > 18 mm
- Complaints of abdominal tightness
- Need to check new labs
- Medication timing misalignment
Signals to Escalate or Stop
- Severe OHSS symptoms
- Unable to safely monitor
- Medical contraindications
- Follicles are growing too unevenly
- High thrombotic risk markers
This escalation framework keeps the cycle safe while protecting euploid embryo yield, the key driver of eventual pregnancy.
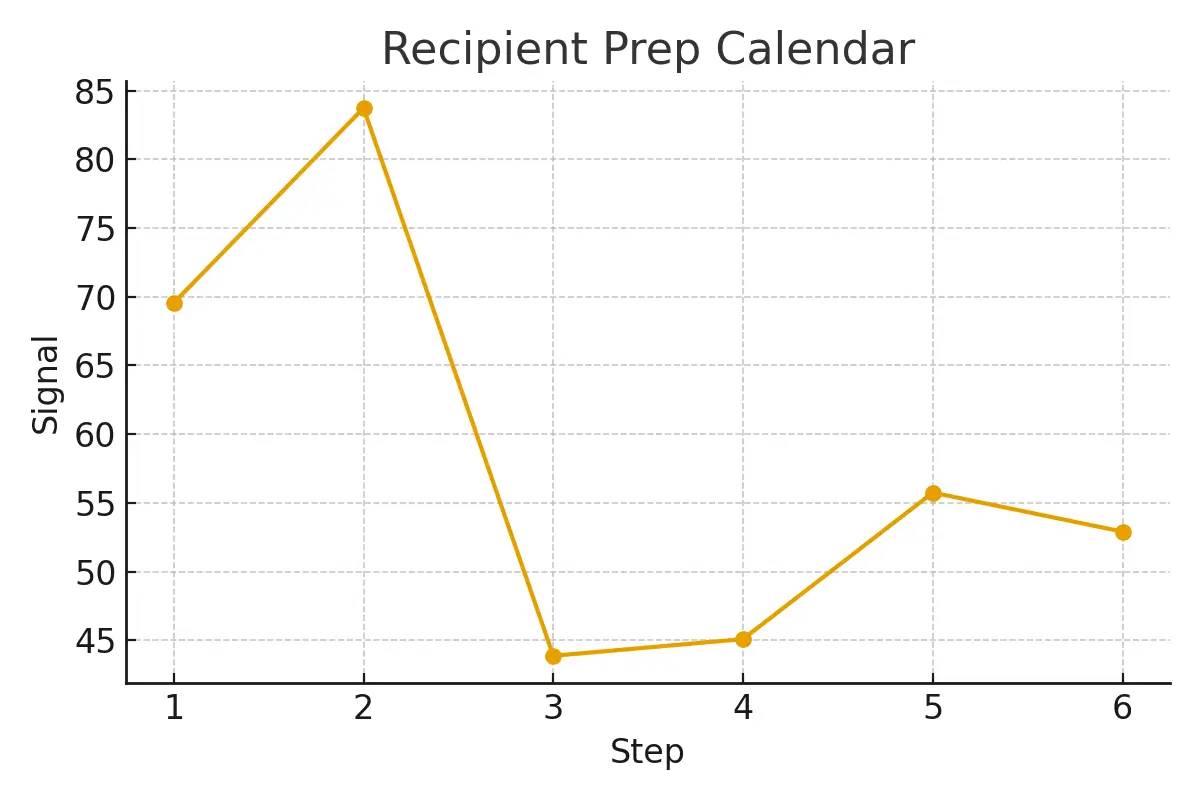
Step-by-Step Management With Timing Checkpoints
Risk-management timing shapes success rates. This is where transparency matters most.
1. Baseline Check (Day 1–3)
- Ultrasound
- Hormone panel
- Green-light decision
- Medication schedule assigned
2. Early Monitoring (Day 4–6)
- First response check
- Dose adjustment
- Hydration guidance
- Predict OHSS likelihood
3. Mid-Stimulation (Day 7–9)
- Daily or every-other-day monitoring
- Contingency planning for retrieval
- Check follicle uniformity
- Confirm trigger medication options
4. Trigger Decision (36 Hours Before Retrieval)
Trigger choice controls OHSS risk:
- HCG trigger → higher risk
- Dual trigger → moderate risk
- Lupron-only trigger → significantly reduces OHSS risk
5. Retrieval Day
- Safety checklist
- Anesthesia team sign-off
- OHSS prevention hydration protocol
- Donor discharge plan
6. Post-Retrieval Management
- Daily symptom watch
- Guidance for bloating
- Medication taper
- Alert triggers
Timing is everything. The clinic’s monitoring cadence directly affects both safety and egg quality.
Pros, Cons, and Realistic Costs (With Line-Item Examples)
Here is what most patients wish they knew at the start.
Pros of Strong Risk-Management Systems
- Higher predictability
- Reduced OHSS incidents
- Fewer cancellations
- Clearer financial planning
- Improved embryo program euploidy yield
Potential Cons
- More monitoring visits
- Higher upfront planning time
- Occasional last-minute schedule shifts
- Additional medication costs
Typical Line-Item Costs
(These vary widely by clinic and region, but this sample helps estimate ranges.)
| Item | Estimated Range |
| Monitoring labs & ultrasounds | $800–$1,800 |
| Medication dose changes | $300–$1,200 |
| Trigger medication alternatives | $50–$350 |
| OHSS monitoring/urgent care | $200–$600 |
| Cycle cancellation fees | $800–$2,500 |
| Extra retrieval support | $100–$500 |
Transparent risk planning prevents surprise bills and helps patients focus on care instead of logistics.
Outcome Drivers You Control vs. Those You Only Monitor
Certain elements in the egg-donation cycle are controllable—and others are not.
You Can Control:
- Medication adherence
- Timing of injections
- Hydration and nutrition
- Reporting symptoms early
- Choosing a clinic with strong monitoring
You Can Only Monitor:
- Biological response to medication
- Number of follicles
- Egg maturity rate
- Embryo euploidy rate
- Genetic outcomes
Understanding the difference reduces stress and helps patients stay grounded.
Top Questions to Ask Your Clinic
Being proactive reduces both risk and confusion. Ask your clinic:
- How do you prevent OHSS in donors?
- What is your cancellation criteria?
- How many monitoring visits do you expect?
- Who decides medication doses—and when?
- What is your average egg maturity rate?
- What contingency plans do you use if scheduling shifts?
- How do you handle unexpected cost changes?
- Can I see a sample timeline for my case?
Expert Insight
“Protect timing and keep plans simple—quality improves when noise goes down.” — Clinical Team
Real Patient Case Study
A couple from NYC began with inconclusive test results, inconsistent timing, and logistical concerns. After reviewing their monitoring cadence and aligning their schedule with the clinic’s lab calendar, they moved from uncertainty to a clear, predictable plan.
Testimonials
“The steps finally made sense.” — A.&J., Manhattan
“Costs were clear; no surprise bills.” — L., Hoboken
“Nurses replied fast with practical coaching.” — K.&V., Queens
Frequently Asked Questions (FAQs)
Q: Is this medical advice?
Ans : No. This guide helps you prepare better questions and understand your clinic’s process.
Q: How many cycles should I plan for?
Ans : Think in ranges. Cumulative success rates matter more than single-cycle outcomes.
Q: What drives cost most?
Ans : Medication, anesthesia, genetics, and the total number of cycles.
Additional Insights That Improve Success
- Cycle Cancellation Criteria: Clear criteria protect euploid embryo yield by preventing unsafe cycles.
- Oocyte Retrieval Strategy: Dose selection + monitoring cadence → better maturity rates.
- Genetic Testing Decisions: Evidence-based embryo testing improves implantation odds.
- Clinic Calendar Alignment: Matching biology to lab hours improves live-birth probability.
- Cost & Financing Plans: Fewer delays = higher emotional and logistical stability.
- Frozen Embryo Transfer (FET): Often shortens time-to-pregnancy with better timing control.
Often shortens time-to-pregnancy with better timing control.
Next Steps — Surrogacy4All
- Free 15-minute nurse consult (212) 661-7673
- Upload your labs for a second opinion
- Get a personalized cost breakdown for your exact case
Conclusion
Effective risk management during a donor-egg cycle isn’t about fear—it’s about clarity, timing, and simplicity. When OHSS prevention, cancellation criteria, and contingency plans are transparent, patients stay safer, cycles stay predictable, and success rates improve. By understanding the steps, asking informed questions, and partnering with a clinic that prioritizes communication, you give yourself the best possible chance at a smooth, humane, and successful journey.
If you’re ready for clearer guidance and a smarter treatment plan, the next step is simple: connect with a care team that treats timing, safety, and communication as core pillars—not afterthoughts.

Dr. Kulsoom Baloch
Dr. Kulsoom Baloch is a dedicated donor coordinator at Egg Donors, leveraging her extensive background in medicine and public health. She holds an MBBS from Ziauddin University, Pakistan, and an MPH from Hofstra University, New York. With three years of clinical experience at prominent hospitals in Karachi, Pakistan, Dr. Baloch has honed her skills in patient care and medical research.