PGT-A with donor eggs is one of the most commonly debated decisions for intended parents using egg donation. Some clinics recommend it for every cycle, while others emphasize that donor-egg embryos already have high success rates without additional testing. This article helps you understand when PGT-A adds value, when it does not, and how to protect timing, clarity, and cost within your Egg Donation 101 pathway.
You’ll see who benefits, how timing affects outcomes, realistic cost examples, and simple decision rules that keep care humane rather than overwhelming.
What Is PGT-A? (Definition & Where It Fits in Your Journey)
PGT-A (Preimplantation Genetic Testing for Aneuploidy) is a lab procedure performed on embryos to identify those with the correct number of chromosomes. Embryos with chromosomal abnormalities are less likely to implant and more likely to miscarry.
PGT-A fits in after fertilization and before embryo transfer, typically on day 5–7 blastocysts.
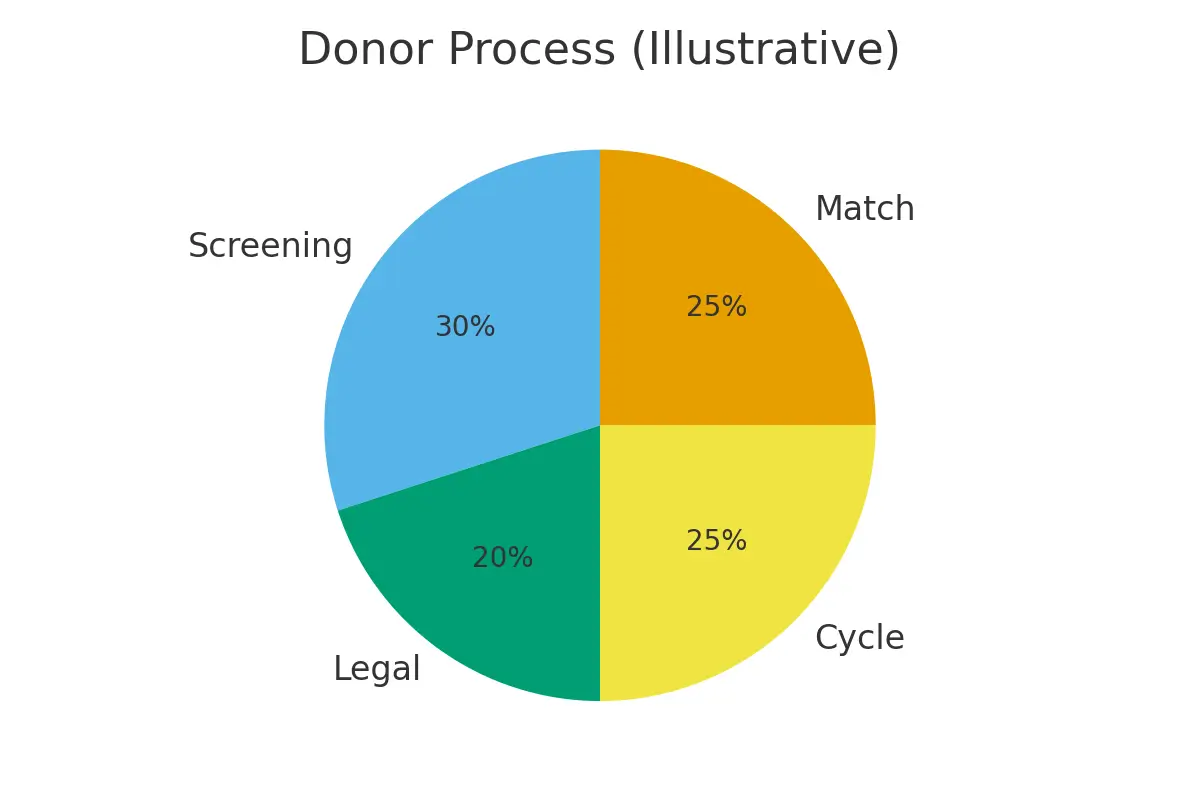
Where This Step Appears in the Donor-Egg Journey:
- Donor screening and selection
- Retrieval and fertilization
- Embryo culture to blastocyst
- PGT-A biopsy (optional)
- Embryo freezing
- Frozen embryo transfer
Key point: With donor eggs—especially from young, medically screened donors—embryo quality is already higher than average. So the question becomes: When does PGT-A provide a meaningful clinical advantage?
Eligibility Signals — When PGT-A Helps, and When to Pause
PGT-A is not one-size-fits-all. The decision depends on medical history, embryo numbers, risk tolerance, and budget.
Below are the strongest signals that PGT-A may help:
When PGT-A Does Help
- Recurrent miscarriage
- Implantation failure after >1 transfer
- One intended parent has a structural chromosomal issue
- You want a single embryo transfer with maximum predictability
- You’re reducing travel cycles and want fewer transfer attempts
- You’re managing a tight timeline or medical window for transfer
When PGT-A Usually Does Not Add Value
- First-time donor-egg cycle with no miscarriage history
- Donor age < 32 and screened
- Only 1–3 blastocysts available
- You plan to transfer embryos sequentially and are comfortable with uncertainty
- Budget is constrained, and testing would reduce the available embryos
Rule of thumb:
PGT-A adds the most value when the goal is predictability, not merely pregnancy chances.
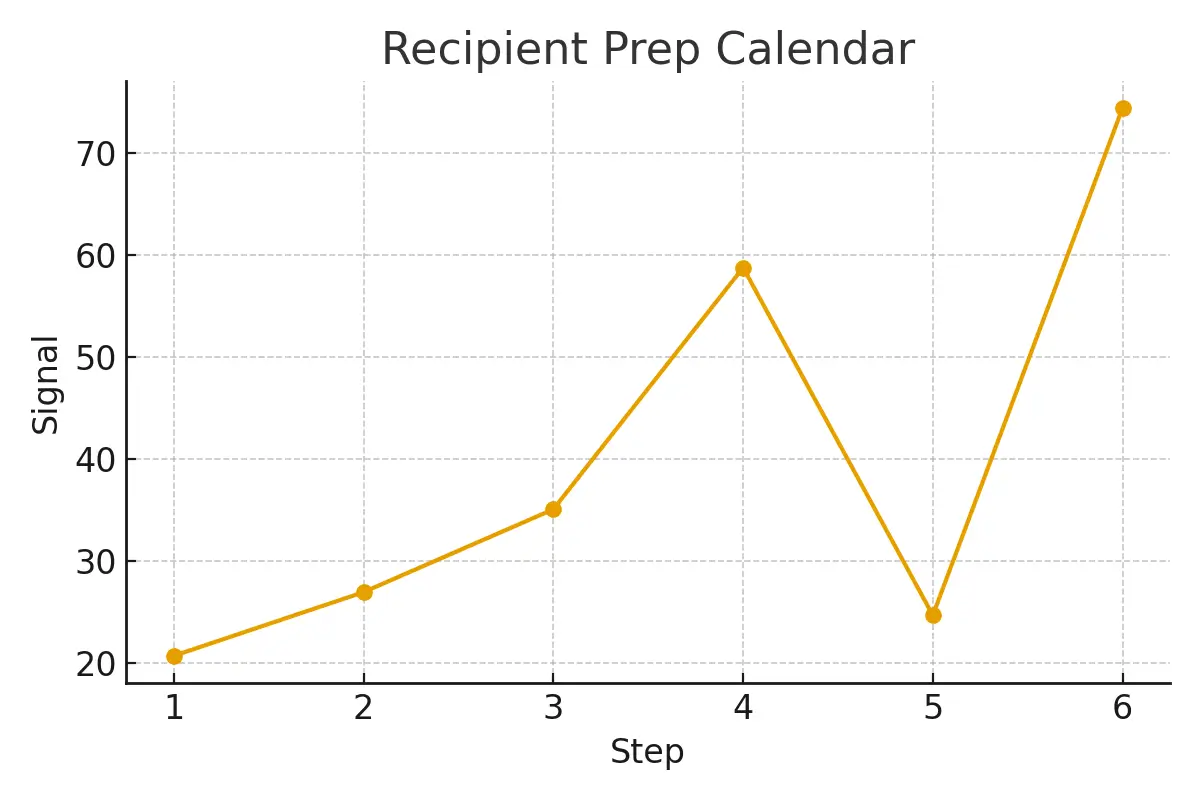
Step-by-Step Process with Timing Checkpoints
Below is a simple timing map so you know what happens and when to watch for key decisions.
Step 1 — Donor Screening (Weeks 1–3)
The donor undergoes infectious disease panels, ovarian reserve measurement, and genetic testing.
Checkpoint:
Confirm your clinic’s lab success rates with donor cycles.
Step 2 — Stimulation & Retrieval (Weeks 4–6)
The donor undergoes ovarian stimulation and egg retrieval.
Checkpoint:
Request the expected egg count based on donor history.
Step 3 — Fertilization (Week 6)
Eggs are fertilized through IVF or ICSI.
Checkpoint:
Ask how many embryos typically reach the blastocyst stage with this lab.
Step 4 — PGT-A Biopsy (Day 5–7)
If chosen, a few trophectoderm cells are biopsied from each blastocyst.
Checkpoint:
Confirm the lab uses validated biopsy equipment and provides uniform grading criteria.
Step 5 — Embryo Freezing & Storage
Biopsied embryos are frozen while PGT-A results are processed (usually 10–14 days).
Checkpoint:
Check cryostorage fees and reporting timeline.
Step 6 — Frozen Embryo Transfer (FET) Cycle
Once results return, the clinic schedules your FET based on your lining and hormone response.
Checkpoint:
Ensure lining monitoring cadence is clear (estrogen start, mid-cycle scan, trigger timing).
Pros, Cons & Practical Costs (with Realistic Line-Item Examples)
PGT-A offers advantages, but also trade-offs. Below is a balanced view.
Advantages of PGT-A with Donor Eggs
1. Higher confidence in selecting a healthy embryo
Even though young donor eggs are of high quality, about 20–30% of embryos may still be abnormal.
2. Reduced risk of miscarriage
A major reason people choose PGT-A after miscarriages is.
3. Improved planning
Patients traveling for transfers gain reliability and fewer canceled cycles.
4. Supports elective single embryo transfer (eSET)
This reduces twin risks while maintaining high success likelihood.
Limitations of PGT-A
1. It does not increase the total embryo number
Biopsy doesn’t “fix” abnormalities.
2. You may lose transferable embryos
Sometimes embryos labeled “mosaic” are still healthy—but some clinics discard them.
3. Added cost and time
Testing delays transfer and adds expense (discussed below).
4. False positives or labeling issues
The accuracy is high, but not perfect.
Realistic Cost Examples (Line-Item Style)
Below is a typical U.S. donor-egg cycle cost breakdown, including PGT-A.
Donor Cycle Cost Breakdown
| Cost Item | Typical Range |
| Donor compensation | $8,000–$12,000 |
| Donor screening & meds | $4,000–$6,000 |
| Cycle management & retrieval | $6,000–$10,000 |
| Embryology + ICSI | $3,500–$5,000 |
| PGT-A biopsy | $3,000–$5,000 |
| PGT-A genetic testing (per embryo) | $250–$400 each |
| Embryo freezing/storage | $800–$1,200 |
| Frozen embryo transfer | $3,500–$5,000 |
Example Scenario:
If you have 6 blastocysts and test all, the PGT-A portion might cost:
- Biopsy: $3,500
- 6 embryos × $325 = $1,950
Total PGT-A cost ≈ $5,450
Outcome Drivers — What You Control vs What You Monitor
Success rates with donor eggs rely on a combination of controllable actions and biological factors.
What You Control
1. Lining preparation
- Estrogen dosing
- Timing of progesterone
- Scan cadence
- Avoiding missed windows
2. Transfer logistics
- Travel
- Scheduling
- Medication adherence
3. Lab selection
- Blastocyst development rate
- Freezing survival rate
- Biopsy experience
What You Monitor
1. Embryo development
You cannot directly change embryo growth, but your choice of lab heavily influences outcomes.
2. Mosaicism rates
Some labs report more mosaics, which affects decision-making.
3. Hormone response
Your lining thickness and progesterone levels determine the transfer day.
Questions to Ask Your Clinic
Here are essential questions that keep your plan simple and reduce surprises:
- How many donor-egg embryos typically reach blastocyst in your lab?
- What percentage of donor-egg embryos test normal with PGT-A here?
- How many embryos do you recommend testing—and why?
- What is your policy for mosaic embryos?
- Do your biopsy results delay my transfer cycle?
- Are there added fees for storage or re-biopsy?
- What is your clinic’s single-embryo transfer success rate?
Expert Quote
“Protect timing and keep plans simple—quality improves when noise goes down.” — Clinical Team
Patient Case Study
A couple in their early 40s from Brooklyn had two previous miscarriages using their own eggs. When shifting to donor eggs, they were unsure whether PGT-A was necessary.
What happened:
- Their donor produced 18 eggs → 11 fertilized → 7 blastocysts
- The clinic recommended PGT-A due to a miscarriage history
- 5 embryos tested normal
- Transfer #1 led to a healthy pregnancy
Why PGT-A helped here:
- History of miscarriage
- Strong embryo numbers
- Need for predictability due to work schedules
For them, testing reduced uncertainty and emotional burden.
Patient Testimonials
“The steps finally made sense.” — A. & J., Manhattan
“Costs were clear; no surprise bills.” — L., Hoboken
“Nurses replied fast with practical coaching.” — K. & V., Queens
Additional Insights That Improve Your Journey
Below are simplified explanations of additional fertility concepts referenced in the Egg Donation 101.
Cycle Cancellation Criteria
Clear rules for cancelling a cycle prevent wasted transfers and speed time to pregnancy.
Ovarian Stimulation Predictability
When stimulation is controlled well, embryo development and lining timing match more precisely.
Pharmacy Logistics
Medication timing is one of the top drivers of embryo competency. Transparent pricing and planning reduce stress.
Lab Quality Indicators
Blastocyst rate, freezing survival rate, and mosaicism reporting thresholds determine cumulative success.
Frozen Embryo Transfer Optimization
FET success depends on correct progesterone exposure, not just lining thickness.
Oocyte Retrieval Strategy
Using the donor’s best cycle—rather than splitting cycles—improves cumulative success for intended parents.
Next Steps — Surrogacy4All
- Free 15-minute nurse consult (212) 661-7673
- Upload your labs for a second opinion
- Get a personalized cost breakdown for your exact case
Conclusion
PGT-A with donor eggs can be extremely useful in specific situations—especially for individuals seeking predictability, those with a miscarriage history, and those who want to minimize transfer attempts. But it is not automatically required for every donor-egg cycle. When used thoughtfully, PGT-A simplifies planning, reduces emotional strain, and helps ensure the first transfer has the highest chance of success.
Your decisions should focus on clarity, timing, and lab quality, not anxiety or pressure. With the right information—and the right clinic partnership—you can move through the Egg Donation pathway with confidence and calm.

Dr. Kulsoom Baloch
Dr. Kulsoom Baloch is a dedicated donor coordinator at Egg Donors, leveraging her extensive background in medicine and public health. She holds an MBBS from Ziauddin University, Pakistan, and an MPH from Hofstra University, New York. With three years of clinical experience at prominent hospitals in Karachi, Pakistan, Dr. Baloch has honed her skills in patient care and medical research.