When it comes to egg donation, one of the most significant decisions intended parents face is choosing between a known donor and an anonymous donor. This decision influences not only the medical and emotional journey but also legal rights, privacy, and long-term family dynamics. Understanding the trade-offs and safeguards in each option helps ensure a smooth, transparent, and ethical fertility journey.
In this comprehensive guide, we’ll explore everything you need to know about known vs anonymous donors—from definitions and eligibility signals to practical costs, timing checkpoints, and expert insights. You’ll also discover how clinics like support intended parents in making clear, informed, and humane decisions.
Understanding the Basics: Known vs Anonymous Donors
Before diving deeper, let’s define these two paths clearly:
- Known Donor: This is someone the recipient already knows—perhaps a friend, relative, or acquaintance. The relationship allows direct interaction and communication, often making the process more personal.
- Anonymous Donor: The identity of the donor remains confidential. The recipient typically selects from a database based on physical traits, medical background, or educational qualifications.
Both options have their benefits, but also distinct emotional, ethical, and legal considerations. Understanding where each fits in your fertility journey is key to making an empowered choice.
Where This Decision Fits in the Egg Donation Journey
The known vs anonymous donor choice typically arises after the recipient and their fertility team confirm that egg donation is medically necessary. This step comes after initial fertility testing, failed IVF cycles, or a diagnosis affecting egg quality or quantity.
At this point, patients discuss donor options with:
- Their reproductive endocrinologist,
- A fertility lawyer, and
- Often, a psychologist specializes in third-party reproduction.
This multidisciplinary approach ensures that every aspect—biological, emotional, and legal—is handled with care.
Eligibility Signals: When to Escalate or Pause
Not everyone qualifies to become or use a donor right away. Both donors and recipients must meet specific medical and psychological benchmarks.
For Donors:
- Age typically between 21 and 32 years
- Good overall health with no genetic or infectious diseases
- Stable mental health
- Willingness to undergo medical and legal screening
For Recipients:
- Confirmed medical need for donor eggs
- Stable psychological readiness
- Financial preparedness for multiple cycle possibilities
If a donor doesn’t meet the above standards, it’s best to pause and re-evaluate, rather than rush into an uncertain arrangement.
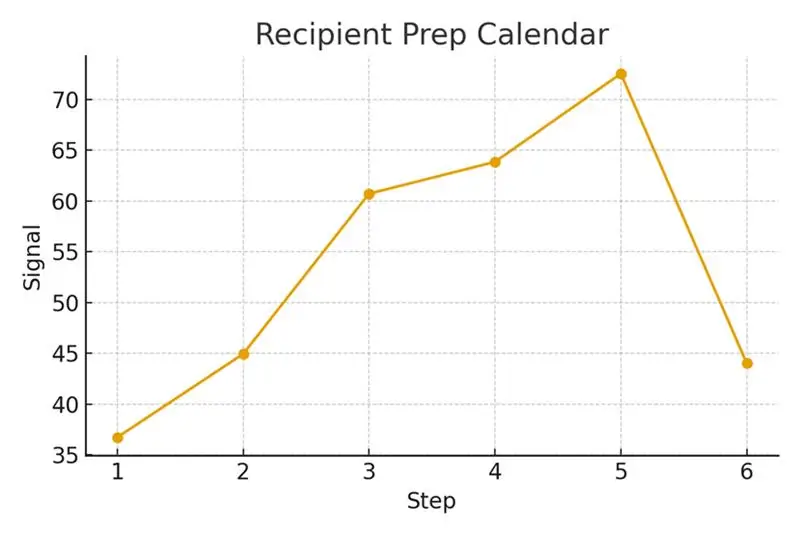
Step-by-Step Process with Timing Checkpoints
Timing plays a crucial role in achieving predictable outcomes. Here’s how the process usually unfolds:
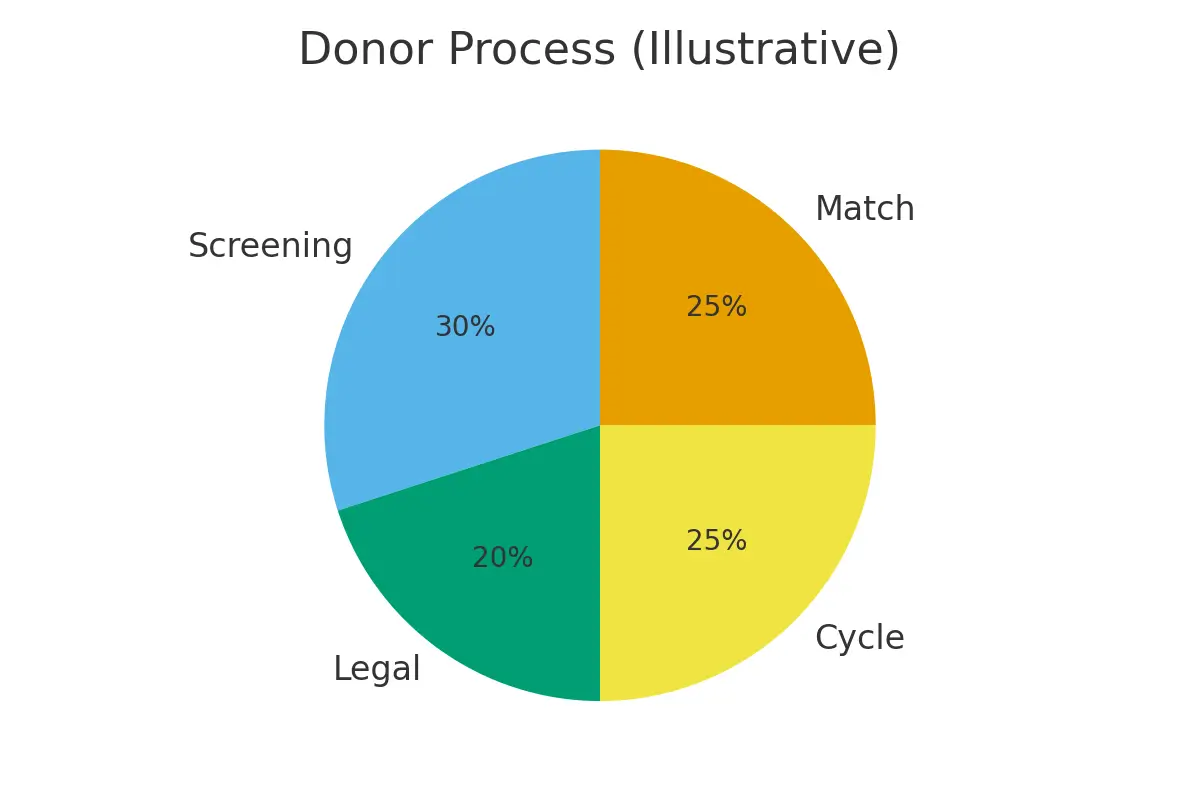
- Initial Consultation & Screening: Medical tests, genetic panels, and mental health evaluations for both donor and recipient.
- Legal Agreements: Contracts outlining compensation, privacy, and parental rights are drafted and signed.
- Cycle Synchronization: The donor’s and recipient’s cycles are synchronized through hormonal medications.
- Ovarian Stimulation: The donor undergoes controlled ovarian stimulation for 10–14 days.
- Egg Retrieval & Fertilization: Eggs are retrieved, fertility in the lab, and embryos are cultured.
- Embryo Transfer: The healthiest embryos are transferred to the recipient’s uterus.
Each checkpoint includes safeguards to protect both donor and recipient—ensuring informed consent, timing accuracy, and medical safety.
Pros, Cons, and Practical Costs with Line-Item Examples
Known Donors
Pros:
- Greater transparency and trust
- Access to full family and medical history
- Potential for ongoing contact (if desired)
- Emotional connection for the child
Cons:
- Possible future emotional or boundary challenges
- Complex legal documentation
- Risk of disagreements about future contact or parental roles
Cost Range:
- Medical & lab fees: $15,000–$25,000
- Legal contracts: $3,000–$5,000
- Psychological evaluation: $1,000–$2,000
Anonymous Donors
Pros:
- Complete privacy and confidentiality
- Streamlined medical and legal process
- Professional donor pool with screened candidates
- Less emotional complexity
Cons:
- Limited access to long-term health updates
- Future curiosity or identity questions from the child
- Legal limitations on donor contact
Cost Range:
- Donor compensation: $8,000–$15,000
- IVF and lab fees: $15,000–$25,000
- Agency and legal fees: $5,000–$10,000
When comparing, consider not just immediate costs but also emotional continuity, future relationships, and transparency needs.
Outcome Drivers You Control vs Those You Monitor
Success in donor egg cycles depends on both controllable and uncontrollable factors.
You Control:
- Selecting a clinic with proven outcomes
- Adhering to treatment schedules
- Maintaining emotional readiness and realistic expectations
- Choosing evidence-based add-ons rather than experimental ones
You Monitor:
- Donor’s response to stimulation
- Embryo development
- Implantation success and live birth outcomes
Trigger timing, for instance, is one of the most critical variables under the clinic’s control. It helps synchronize cycle predictability, minimizes logistic delays, and increases the chance of successful fertilization.
Questions to Ask Your Clinic
When navigating donor options, these are essential questions to ask:
- What medical and psychological screening do donors undergo?
- How are donor identities protected or disclosed?
- What are the success rates for known vs anonymous donors?
- How do you handle donor-recipient matching logistics?
- What are the total estimated costs, including medications and legal fees?
- Can I switch from an anonymous to a known donor mid-process?
Expert Quote
Protect timing and keep plans simple—quality improves when noise goes down.
Real Patient Case Study
A couple from NYC began their fertility journey after inconclusive IVF results. Initially overwhelmed by choices, they collaborated closely with their fertility nurse and legal advisor.
By aligning their expectations early, they chose a known donor who met all medical and emotional criteria. This decision streamlined logistics, reduced delays, and improved embryo quality. The couple appreciated having a clear, predictable roadmap, and ultimately, they achieved a successful pregnancy on their second cycle.
Testimonials
- “The steps finally made sense.” — A.&J., Manhattan
- “Costs were clear; no surprise bills.” — L., Hoboken
- “Nurses replied fast with practical coaching.” — K.&V., Queens
These testimonials highlight how structured planning and transparent communication simplify what can otherwise feel like an overwhelming process.
Additional Clinical Insights
Fertility experts emphasize several high-impact practices that improve outcomes in both known and anonymous donor cycles:
- Trigger Timing: Synchronizes cycle predictability and minimizes logistical delays.
- Ovarian Stimulation: Enhances live-birth probability when tailored to individual response patterns.
- Luteal Support: Aligns with lab cutoffs to maximize embryo viability and euploidy yield.
- Donor Screening Checks: Optimize patient experience by reducing risk and ensuring ethical compliance.
- Legal Consent and Contracts: Minimize multiple birth risks and protect all parties involved.
Each of these steps, when coordinated effectively, helps maintain simplicity, safety, and success.
Frequently Asked Questions (FAQs)
Q: Is this medical advice?
Ans: No. This information is educational and should guide your discussions with your fertility clinic.
Q: How many cycles should I plan?
Ans: Think in ranges. Cumulative success rates—rather than single-cycle results—offer a more realistic view.
Q: What drives cost most?
Ans: Medications, genetic testing, anesthesia, and the total number of cycles are the primary cost drivers.
Next Steps with Surrogacy4All
At Surrogacy4All, you can take the next step confidently with:
- Free 15-minute nurse consultation (212) 661-7673
- Option to upload lab results for a second opinion
- Personalized cost breakdown for your unique case
Their patient-first approach ensures every step—from donor selection to legal consent—is transparent, ethical, and tailored to your needs.
Conclusion
Choosing between a known and an anonymous donor is a deeply personal decision that shapes your fertility experience. Each option carries unique advantages, responsibilities, and emotional nuances. The key is to combine timing discipline, legal clarity, and compassionate clinical guidance to achieve the best possible outcome.
Whether you prioritize privacy, transparency, or emotional connection, what matters most is making an informed, humane choice—one that aligns with your values and long-term family goals. With the right safeguards and expert support, your path to parenthood can remain both predictable and profoundly meaningful.

Dr. Kulsoom Baloch
Dr. Kulsoom Baloch is a dedicated donor coordinator at Egg Donors, leveraging her extensive background in medicine and public health. She holds an MBBS from Ziauddin University, Pakistan, and an MPH from Hofstra University, New York. With three years of clinical experience at prominent hospitals in Karachi, Pakistan, Dr. Baloch has honed her skills in patient care and medical research.