Understanding what insurance actually covers—and what it doesn’t—is often more confusing than the medical steps themselves. This guide explains insurance and financing in plain English, showing where coverage fits into the donor options pathway, what it can change for your budget and timing, and how early decisions influence downstream costs. The goal: remove surprises and give you a clear, predictable plan.
What It Is
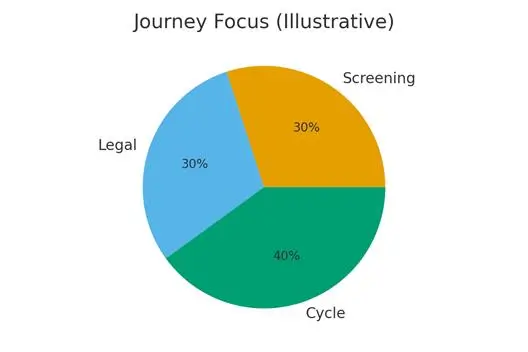
Insurance & Financing — What Can Be Covered means understanding:
- What parts of donor options may be covered vs always out-of-pocket
- How insurance rules, authorizations, and diagnosis codes shape your total cost
- Why timing matters (labs, imaging, consultations, cycle day cutoffs)
- How coverage differs for donor sperm vs donor eggs vs donor embryos
- How smart sequencing reduces denials and unnecessary cash payments
In short: line up coverage and financing early so medical steps stay smooth later.
Who It Helps
Strong Fit
This guide is especially helpful for:
- Anyone unsure which parts of treatment their insurance will support
- Those working within a fixed budget or limited savings
- Patients 35–38+ who need clarity before committing to donor pathways
- Individuals/couples with complex history (low response, poor labs, abnormal imaging)
- Families using donor sperm, eggs, or embryos who need predictable cash-flow planning
- People navigating employer fertility benefits or new reimbursement programs
Consider a Different Path (or Adjusted Strategy) If
- Your insurance excludes all donor-related services and cash cost is prohibitive
- You need urgent treatment and cannot wait for authorization timelines
- Imaging or baseline labs require correction before coverage applies
- A donor is limited and may sell out before approval is finalized
- Financing terms increase total cost beyond what cycle timing permits
Step-by-Step: A Clear Sequence to Avoid Denials & Stress
1. Verify “What Is Covered” Before Anything Else
Ask for written confirmation on:
- Diagnostic testing
- Monitoring
- Medications
- Retrieval and transfer fees
- Donor materials (usually not covered)
- PGT or storage
2. Secure Correct Diagnosis Codes
Insurance often hinges on coding:
- Without the correct infertility diagnosis, claims can be denied.
- Donor-related codes may require additional documentation.
3. Complete All Required Testing First
Many insurers require:
- Day 3 labs
- AMH
- Semen analysis
- Uterine imaging
- Standard infectious disease tests
Coverage may start only after these are documented.
4. Obtain Prior Authorizations Early
Authorizations can take 1–4 weeks, depending on:
- Your insurer
- Medical complexity
- Donor pathway chosen
5. Align Medical Steps With Coverage Windows
For example:
- Some plans require all monitoring within a single cycle window
- Some limit the number of ultrasounds or blood draws
- Some require medications to be filled through a specific pharmacy
6. Plan Cash Components Separately
Typical out-of-pocket items:
- Donor eggs / embryo cohorts
- Donor sperm vials
- Storage fees
- PGT
- Embryo shipping
Plan these early so they don’t collide with insurance timing.
7. Recheck Coverage Before Transfer
Insurance rules can change annually.
Confirm:
- Medication approvals
- Transfer fees
- Updated lab requirements
- Storage-to-clinic transfer documentation
Pros & Cons
Pros
- Reduces overall treatment cost when coverage applies
- Decreases financial stress mid-cycle
- Allows smarter sequencing of diagnostics and treatment
- Makes donor-pathway budgeting more predictable
- Helps prevent surprise bills and retroactive denials
Cons
- Coverage is inconsistent and varies by employer/state
- Donor components are often excluded
- Authorizations can delay treatment timelines
- Incorrect coding can lead to denied claims
- Financing may increase total cost if stretched long-term
Costs & Logistics
Line Items to Track
- Consultation and diagnostic testing
- Monitoring visits
- Retrieval and transfer fees
- IVF lab procedures (ICSI, PGT, cryopreservation)
- Medications (cycles and prep meds)
- Donor materials (eggs, embryos, sperm)
- Storage and shipping fees
- Legal/documentation costs for third-party reproduction
Prior Authorizations
Common items requiring PA:
- Stimulation medications
- Trigger shots
- IVF procedures
- PGT
- Cycle monitoring
- Uterine preparation protocols
Cash-Flow Scenarios
- Insurance covers diagnostics + monitoring; donor materials paid out of pocket
- Insurance covers IVF procedures; donor products + storage paid separately
- No insurance → financing options, fixed payment plans, or clinic bundles
- Mixed coverage → sequencing steps to maximize benefits
Tracking to Prevent Surprise Bills
Create a simple grid:
- Covered vs not covered
- Prepaid vs billed later
- PA needed vs not needed
- Annual limits and lifetime caps
- Out-of-network penalties
- Pharmacy restrictions
What Improves Outcomes
High-Impact Actions
- Completing all baseline testing early to activate coverage
- Using correct, clinic-approved diagnosis codes
- Timing cycles to match coverage windows
- Obtaining multiple authorizations at once (when allowed)
- Confirming donor availability before finalizing PA timelines
- Keeping copies of all approvals and benefits summaries
Low-Impact Actions
- Calling insurance repeatedly without documentation
- Paying cash for items that insurers would cover with correct coding
- Overbuying meds before knowing what is reimbursable
- Relying on verbal statements from insurers—not enough for appeals
Case Study: From Confusion to a Clear Financial Plan
A couple planning donor egg IVF assumed nothing would be covered.
After reviewing their plan:
What they discovered:
- Diagnostics, monitoring, retrieval, and transfer were fully covered
- Donor eggs + PGT + storage were cash pay
- Medications required prior authorization through a specialty pharmacy
What they did:
- Completed all required labs and imaging to activate coverage.
- Submitted authorizations 4 weeks before stimulation.
- Sequenced billing so insurance covered medical portions while they prepaid donor eggs.
- Tracked all costs using a simple covered/out-of-pocket table.
Outcome:
Their out-of-pocket cost dropped by 40%, timelines were predictable, and no surprise bills arrived mid-cycle.
Mistakes to Avoid
- Starting cycles before confirming coverage
- Assuming donor pathways are 100% self-pay (many components are covered)
- Skipping required testing and losing eligibility for benefits
- Not verifying diagnosis codes on every claim
- Allowing donor selection to stall while authorizations expire
- Ignoring annual insurance changes
- Not planning for storage fees long-term
FAQs
Q: Are donor eggs or donor embryos covered by insurance?
Ans : Usually no—but many plans cover the medical procedures around them.
Q: Are medications covered?
Ans : Often yes, but require prior authorization and specific pharmacies.
Q: Can insurance cover monitoring and transfer even if donor gametes are self-pay?
Ans : Yes—this is common.
Q: What if insurance denies a claim?
Ans : Appeals are frequently successful with correct diagnosis coding and documentation.
Q: Is financing available for donor cycles?
Ans : Most clinics offer payment plans, third-party lenders, or bundled treatment packages.
Next Steps
- Free 15‑min nurse consult
- Upload labs
- Cost breakdown for your case.
Related Links

Dr. Kulsoom Baloch
Dr. Kulsoom Baloch is a dedicated donor coordinator at Egg Donors, leveraging her extensive background in medicine and public health. She holds an MBBS from Ziauddin University, Pakistan, and an MPH from Hofstra University, New York. With three years of clinical experience at prominent hospitals in Karachi, Pakistan, Dr. Baloch has honed her skills in patient care and medical research.





