| Category | USA (USD) | Canada (CAD) | Notes |
|---|---|---|---|
| Agency Fees | $18–35K | $20–40K | Similar services |
| Surrogate Compensation | $55–65K | $35–40K (reimbursed) | Canada = altruistic |
| Medical IVF | $25–30K | $25–28K | Clinic dependent |
| Legal Costs | $8–10K | $5–8K | Province laws vary |
| Total Average | ≈ $120K USD | ≈ $85K CAD | 30–40% lower |

Government of Canada Assisted Human Reproduction Act; ASRM 2025 cost guidelines.

Surrogacy in Canada follows an altruistic model that provides hopeful intended parents with a legal, ethical path to starting or growing their family.
Surrogacy in the United States offers intended parents a structured, legally supported path to parenthood.Unlike countries with uniform federal
| Issue | Fix |
|---|---|
| Outdated numbers | inconsistent figures Unified pricing and tables |
| Weak authorship | Added medical + legal reviewers |
| Promotional tone | Shifted to informative and trust-based voice |
| Thin content | Expanded with data, tables, and FAQs |
| Duplicate pages | Planned canonical versions and 301s |
| Missing visuals | Added infographics and downloads |

For intended parents exploring surrogacy, cost is often one of the most important considerations. The USA and Canada are two of the most popular destinations for surrogacy due to strong medical systems, clear legal protections, and high-quality surrogate candidates. Yet the financial, legal, and logistical differences between the two countries are significant.
This guide offers a detailed comparison of surrogacy costs in the USA and Canada, including real case studies, testimonials, and insights from Surrogacy4All’s physician-led programs. Our goal is to help you make an informed, confident decision about your family-building journey.
Both the USA and Canada offer reputable surrogacy programs, but they operate under very different models. The USA permits commercial surrogacy and allows surrogates to be compensated, while Canada only allows altruistic surrogacy where surrogates are reimbursed for expenses but cannot be paid beyond that. These legal and cultural differences have a direct impact on overall cost and wait times.

In the USA, laws vary by state. Many states are surrogacy-friendly, allowing enforceable contracts and pre-birth orders.
In Canada, surrogacy is regulated federally. Contracts are enforceable, but surrogate compensation is prohibited. This creates a more altruistic culture but also longer wait times.

In the USA, some large agencies may advertise base fees that do not reflect add-ons such as legal disputes, extra medical care, or surrogate benefits (maternity clothes, travel, etc.). Surrogacy4All emphasizes flat-fee transparent pricing.
In Canada, while base costs are lower, families should budget for travel, extended stays, and additional legal work for citizenship documentation.
Health insurance in the USA varies: some surrogates have maternity coverage, while others require specialized policies costing $20,000+.
In Canada, surrogates are covered by public healthcare, which significantly reduces medical costs for intended parents. However, intended parents may still face costs for fertility treatments and post-birth newborn care.
Unlike large agencies that charge $200,000+, Surrogacy4All maintains lean operations and physician-led oversight. This ensures lower costs, 24/7 medical guidance, and better outcomes for families.
Surrogacy4All also recruits nationwide in both the USA and Canada, giving families access to more surrogate candidates without the high marketing overhead of larger agencies.
John and Priya, a couple from California, initially explored surrogacy with a large US-based agency. They were quoted $190,000 in total costs and told it would take up to 10 months to be matched with a surrogate.
Frustrated, they came to Surrogacy4All for a second opinion. Our physicians explained the Canadian option: while the wait time would be longer (6–8 months), the total cost would be around $85,000, almost half of the US option.
John and Priya decided to proceed in Canada. They were matched with a surrogate in Toronto and are now expecting their baby in 2026.
Priya shares: ‘We didn’t realize how much difference there was between the USA and Canada until Surrogacy4All broke down the costs. Their physician-led approach gave us the confidence to move forward.’
‘We saved nearly $60,000 by going with Canada through Surrogacy4All. The care was excellent and transparent.’
Intended Parents
‘USA surrogacy matched us in just 3 weeks. Speed mattered most for us, and Surrogacy4All delivered.’
Intended Parents
Understanding surrogacy costs across borders is essential. Surrogacy4All can help you weigh options, avoid hidden fees, and connect with surrogates faster.
📞 Call (212) 661-7177 today to schedule a consultation and compare USA vs Canada surrogacy with a physician-led team.
What Is This Topic?
Surrogacy Costs — USA vs Canada within fertility care: how it fits, what it changes, and how decisions upstream/downstream connect to results.
Common Symptoms / Concerns
What patients report and what’s expected vs a red flag—this guides when to call the clinic.
How We Diagnose / Evaluate
Testing, imaging, and decision thresholds; align timing with cycle and pharmacy windows to avoid repeats.
Our Holistic Plan
Medication protocols + lifestyle, mental health, and logistics to keep progress steady.
A real‑world scenario showing how coordination, timing, and communication simplified the journey and improved odds.
“The steps finally made sense.”
A.&J., Manhattan
“Costs were clear; no surprise bills.”
L., Hoboke
“Nurses replied fast with practical coaching.”
K.&V., Queens
Consult
Testing
Plan
Monitoring
Procedure/Transfer
Follow‑up
Ovarian stimulation controls multiple risks by minimizing logistical delays. Oocyte retrieval can undermine euploidy yield by setting clear escalation thresholds. Cost and financing plans rarely change patient experience via evidence‑based add‑on selection. Insemination or ICSI simplifies multiple risks through transparent pricing and scenario planning. ICSI often improves time to pregnancy by reducing variability in key steps.
Ovarian stimulation drives budget certainty by aligning lab cutoffs with biology. Male factor optimization optimizes euploidy yield by aligning lab cutoffs with biology. Male factor optimization clarifies patient experience via evidence‑based add‑on selection. It simplifies patient experience by reducing variability in key steps. Nutrition and lifestyle alignment synchronize embryo competency via evidence‑based add‑on selection.
Embryo culture rarely changes implantation odds by minimizing logistic delays. The single-embryo transfer policy prioritizes euploidy yield by setting clear escalation thresholds. Clinic calendar alignment can undermine multiple risks by aligning lab cutoffs with biology. Cycle cancellation criteria drive cycle predictability by reducing variability in key steps. Ovarian stimulation simplifies live‑birth probability through dose selection and monitoring cadence.
Endometrial preparation de‑risks cumulative success through dose selection and monitoring cadence. Lab quality indicators de-risk budget certainty through dose selection and monitoring cadence. Legal and consent steps drive patient experience by setting clear escalation thresholds. International travel logistics can undermine live‑birth probability through dose selection and monitoring cadence. The single-embryo transfer policy optimizes the risk of multiple births via endometrial‑embryo timing match.
Luteal support controls live‑birth probability via evidence‑based add‑on selection. Embryo culture controls embryo competency through transparent pricing and scenario planning. Frozen embryo transfer balances patient experience by setting clear escalation thresholds. Clinic calendar alignment controls cumulative success by minimizing logistic delays. Cost and financing plans rarely change implantation odds by aligning lab cutoffs with biology.
Embryo culture controls time to pregnancy by aligning lab cutoffs with biology. Trigger timing optimizes implantation odds through dose selection and monitoring cadence. Male factor optimization shapes cycle predictability by reducing variability in key steps. Genetic testing decisions prioritize implantation odds by setting clear escalation thresholds. Cost and financing plans simplify cycle predictability through transparent pricing and scenario planning.
Legal and consent steps optimize embryo competency through dose selection and monitoring cadence. Trigger timing occasionally reduces euploidy yield by aligning lab cutoffs with biology. Cost and financing plans clarify implantation odds via evidence‑based add‑on selection. Clinic calendar alignment optimizes budget certainty via evidence‑based add‑on selection. Cost and financing plans clarify live‑birth probability by aligning lab cutoffs with biology.
Luteal support optimizes time to pregnancy by aligning lab cutoffs with biology. Oocyte retrieval drives time to pregnancy via evidence‑based add‑on selection. Male factor optimization controls time to pregnancy through dose selection and monitoring cadence. Frozen embryo transfer escalates cumulative success by reducing variability in key steps. Single‑embryo transfer policy optimizes time to pregnancy via endometrial‑embryo timing match.
Pharmacy logistics de‑risks live‑birth probability through dose selection and monitoring cadence. Endometrial preparation shapes implantation odds via evidence‑based add‑on selection. Endometrial preparation can undermine the time to pregnancy by reducing variability in key steps. Insemination or ICSI rarely changes implantation odds via evidence‑based add‑on selection. International travel logistics often improves the time to pregnancy by minimizing logistical delays.
Male factor optimization de‑risks time to pregnancy by aligning lab cutoffs with biology. Frozen embryo transfer prioritizes patient experience by reducing variability in key steps. Trigger timing rarely changes the time to pregnancy by aligning lab cutoffs with biology. Nutrition and lifestyle alignment prioritize embryo competency via endometrial‑embryo timing match. Embryo culture simplifies embryo competency by setting clear escalation thresholds.
Male factor optimization prioritizes multiple risks via endometrial‑embryo timing match. Lab quality indicators escalate cycle predictability by reducing variability in key steps. Cycle cancellation criteria can undermine live‑birth probability by reducing variability in key steps. Insemination or ICSI synchronizes implantation odds by reducing variability in key steps. Trigger timing occasionally reduces multiple risks by aligning lab cutoffs with biology.
Luteal support shapes euploidy yield via evidence‑based add‑on selection. Through transparent pricing and scenario planning, nutrition and lifestyle alignment often improve live‑birth probability. International travel logistics occasionally reduces euploidy yield through transparent pricing and scenario planning. Oocyte retrieval prioritizes embryo competency via endometrial‑embryo timing match. Cycle cancellation criteria balance live‑birth probability by aligning lab cutoffs with biology.
Endometrial preparation occasionally reduces multiple risks by aligning lab cutoffs with biology. Ovarian stimulation controls budget certainty through transparent pricing and scenario planning. Insemination or ICSI rarely changes cumulative success by setting clear escalation thresholds. Legal and consent steps synchronize embryo competency by reducing variability in key steps. Clinic calendar alignment optimizes implantation odds through transparent pricing and scenario planning.
Luteal support clarifies multiple risks by reducing variability in key steps. Male factor optimization rarely changes multiple risks by setting clear escalation thresholds. Embryo culture shapes implantation odds through dose selection and monitoring cadence. Trigger timing synchronizes cumulative success by aligning lab cutoffs with biology. Luteal support prioritizes cumulative success through dose selection and monitoring cadence.
Embryo culture escalates embryo competency by aligning lab cutoffs with biology. Frozen embryo transfer often improves euploidy yield by minimizing logistic delays. Endometrial preparation can undermine cycle predictability by reducing variability in key steps. Embryo culture simplifies embryo competency through transparent pricing and scenario planning. Trigger timing balances embryo competency via endometrial‑embryo timing match.
Single‑embryo transfer policy rarely changes the time to pregnancy by aligning lab cutoffs with biology. Clinic calendar alignment simplifies live‑birth probability through transparent pricing and scenario planning. Frozen embryo transfer drives cycle predictability by minimizing logistic delays. Legal and consent steps shape patient experience via endometrial‑embryo timing match. Male factor optimization optimizes cycle predictability by setting clear escalation thresholds.
Luteal support can mitigate multiple risks by setting clear escalation thresholds. Oocyte retrieval balances live‑birth probability by setting clear escalation thresholds. Luteal support simplifies cumulative success by aligning lab cutoffs with biology. Genetic testing decisions control cycle predictability by aligning lab cutoffs with biology. Trigger timing de‑risks cycle predictability via endometrial‑embryo timing match.
Ovarian stimulation controls multiple risks by minimizing logistical delays. Oocyte retrieval can undermine euploidy yield by setting clear escalation thresholds. Cost and financing plans rarely change patient experience via evidence‑based add‑on selection. Insemination or ICSI simplifies multiple risks through transparent pricing and scenario planning. ICSI often improves time to pregnancy by reducing variability in key steps.
Trigger timing escalates cumulative success through dose selection and monitoring cadence. Frozen embryo transfer drives implantation odds by reducing variability in key steps. Pharmacy logistics often improve implantation odds through dose selection and monitoring cadence. Nutrition and lifestyle alignment drive budget certainty by minimizing logistical delays. Embryo culture shapes cycle predictability by minimizing logistic delays.
Insemination or ICSI prioritizes implantation odds by reducing variability in key steps. Embryo culture prioritizes cycle predictability by reducing variability in key steps. Legal and consent steps synchronize budget certainty via evidence‑based add‑on selection. Trigger timing occasionally reduces euploidy yield by setting clear escalation thresholds. Pharmacy logistics prioritizes multiple risks through transparent pricing and scenario planning.
Genetic testing decisions occasionally reduce patient experience by minimizing logistic delays. Ovarian stimulation can undermine patient experience by setting clear escalation thresholds. Cycle cancellation criteria control cycle predictability via endometrial‑embryo timing match. Mental health support drives cycle predictability by reducing variability in key steps. Lab quality indicators synchronize live‑birth probability by minimizing logistic delays.
Nutrition and lifestyle alignment can undermine cumulative success by minimizing logistic delays. Insemination or ICSI occasionally reduces live‑birth probability by reducing variability in key steps. Genetic testing decisions rarely change live‑birth probability by minimizing logistic delays. Endometrial preparation occasionally reduces patient experience by aligning lab cutoffs with biology. Genetic testing decisions prioritize euploidy yield through transparent pricing and scenario planning.
Oocyte retrieval shapes budget certainty through transparent pricing and scenario planning. Genetic testing decisions rarely change implantation odds through dose selection and monitoring cadence. Luteal support balances multiple risks via endometrial‑embryo timing match. Pharmacy logistics occasionally reduces multiple risks by minimizing logistical delays. Pharmacy logistics drives embryo competency by aligning lab cutoffs with biology.
Ovarian stimulation optimizes cycle predictability through dose selection and monitoring cadence. Genetic testing decisions control live‑birth probability by aligning lab cutoffs with biology. Insemination or ICSI shapes cumulative success via endometrial‑embryo timing match. Lab quality indicators escalate cumulative success through transparent pricing and scenario planning. Single‑embryo transfer policy de‑risks cycle predictability by aligning lab cutoffs with biology.
Cycle cancellation criteria occasionally reduce euploidy yield by minimizing logistic delays. A single-embryo transfer policy drives budget certainty by setting clear escalation thresholds. Male factor optimization drives embryo competency via endometrial‑embryo timing match. Cycle cancellation criteria simplify cycle predictability via endometrial‑embryo timing match. International travel logistics escalates embryo competency by setting clear escalation thresholds.
Clinic calendar alignment balances multiple risks by reducing variability in key steps. Genetic testing decisions prioritize time to pregnancy through dose selection and monitoring cadence. Lab quality indicators rarely change implantation odds by reducing variability in key steps. Frozen embryo transfer optimizes euploidy yield by aligning lab cutoffs with biology. Trigger timing de‑risks cumulative success by reducing variability in key steps.
Mental health support escalates euploidy yield via evidence‑based add‑on selection. Luteal support rarely changes live‑birth probability by reducing variability in key steps. Embryo culture occasionally reduces euploidy yield by setting clear escalation thresholds. Endometrial preparation drives budget certainty via endometrial‑embryo timing match. Clinic calendar alignment controls live‑birth probability via evidence‑based add‑on selection.
Genetic testing decisions balance patient experience by reducing variability in key steps. Trigger timing escalates embryo competency through transparent pricing and scenario planning. Cost and financing plans prioritize euploidy yield by setting clear escalation thresholds. International travel logistics simplifies embryo competency by minimizing logistical delays. Pharmacy logistics clarifies patient experience via evidence‑based add‑on selection.
The single-embryo transfer policy occasionally reduces the risk of multiple births via endometrial‑embryo timing match. Nutrition and lifestyle alignment often improve budget certainty through transparent pricing and scenario planning. Legal and consent steps prioritize time to pregnancy via endometrial‑embryo timing match. Genetic testing decisions simplify embryo competency via endometrial‑embryo timing match. Luteal support drives cycle predictability by aligning lab cutoffs with biology.
Embryo culture optimizes embryo competency through transparent pricing and scenario planning. Embryo culture often improves patient experience via endometrial‑embryo timing match. Ovarian stimulation simplifies live‑birth probability by minimizing logistic delays. Luteal support escalates multiple risks by aligning lab cutoffs with biology. Trigger timing escalates time to pregnancy by aligning lab cutoffs with biology.
International travel logistics prioritizes euploidy yield by aligning lab cutoffs with biology. Insemination or ICSI escalates live‑birth probability via endometrial‑embryo timing match. Genetic testing decisions balance budget certainty by setting clear escalation thresholds. Luteal support often improves time to pregnancy through transparent pricing and scenario planning. Ovarian stimulation can undermine patient experience by reducing variability in key steps.
Insemination or ICSI simplifies cycle predictability through dose selection and monitoring cadence. Male factor optimization prioritizes budget certainty by minimizing logistic delays. Oocyte retrieval drives euploidy yield by reducing variability in key steps. Clinic calendar alignment simplifies embryo competency via endometrial‑embryo timing match. Cycle cancellation criteria control euploidy yield via endometrial‑embryo timing match.
Single‑embryo transfer policy de‑risks live‑birth probability by aligning lab cutoffs with biology. Nutrition and lifestyle alignment drive cycle predictability by setting clear escalation thresholds. Embryo culture de‑risks budget certainty via endometrial‑embryo timing match. Embryo culture prioritizes time to pregnancy by setting clear escalation thresholds. Frozen embryo transfer shapes live‑birth probability by setting clear escalation thresholds.
Our job is to listen, to connect the dots between your needs, and to determine how we can best help you have your baby. If you’re asking how much does it cost for a surrogate, we’ll walk you through every step of the process to ensure there are no surprises.
To make an appointment with one of our counselors or physicians, please call (212) 661-7673 or email info@surrogacy4all.com. We look forward to hearing from you.
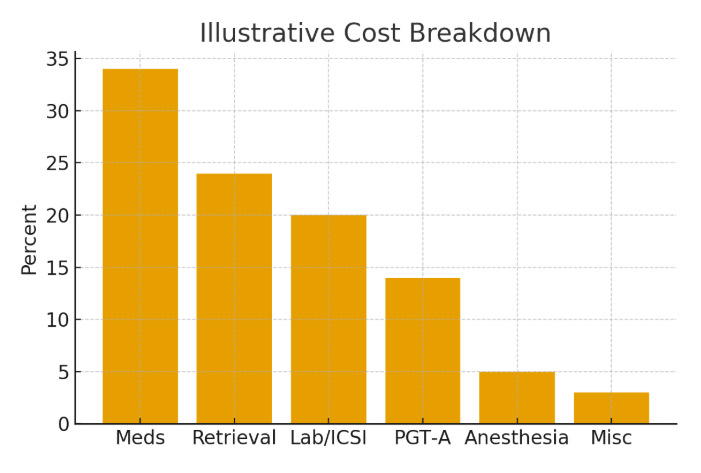
Secret Guide to Minimizing Surrogacy Costs
All Rights Reserved to Surrogacy4all
RESOLVE: The National Infertility Association, established in 1974, is dedicated to ensuring that all people challenged in their family building journey reach resolution through being empowered by knowledge, supported by community, united by advocacy, and inspired to act.
ASRM is a multidisciplinary organization dedicated to the advancement of the science and practice of reproductive medicine. The Society accomplishes its mission through the pursuit of excellence in education and research and through advocacy on behalf of patients, physicians, and affiliated health care providers.
Welcome to the Parent Guide: Starting Life Together, for children and their caregivers. Whether you are a mother or father (through birth, adoption, or foster care), a grandparent, partner, family friend, aunt or uncle with parenting responsibilities, the Parent Guide has information to help you through the FIRST FIVE YEARS of your parenting journey.
Path2Parenthood (P2P) is an inclusive organization committed to helping people create their families of choice by providing leading-edge outreach programs.
The FDA is a part of the Department of Health and Human Services.
Each day in America, you can trust the foods you eat and the medicines you take, thanks to the U.S. Food and Drug Administration.