In the evolving world of assisted reproduction, donor stimulation protocols play a critical role in determining both the safety of the donor and the egg yield that intended parents can expect. This article guides you through every essential aspect of stimulation protocols within the Egg Donation 101 pathway—covering eligibility, timing, outcomes, costs, and practical decision rules so you can move forward with confidence.
You’ll learn who benefits, what steps matter most, how timing shapes egg quality, and how to simplify logistics so your treatment remains predictable, humane, and aligned with best-practice care.
Definitions — Where Donor Stimulation Fits in the Journey
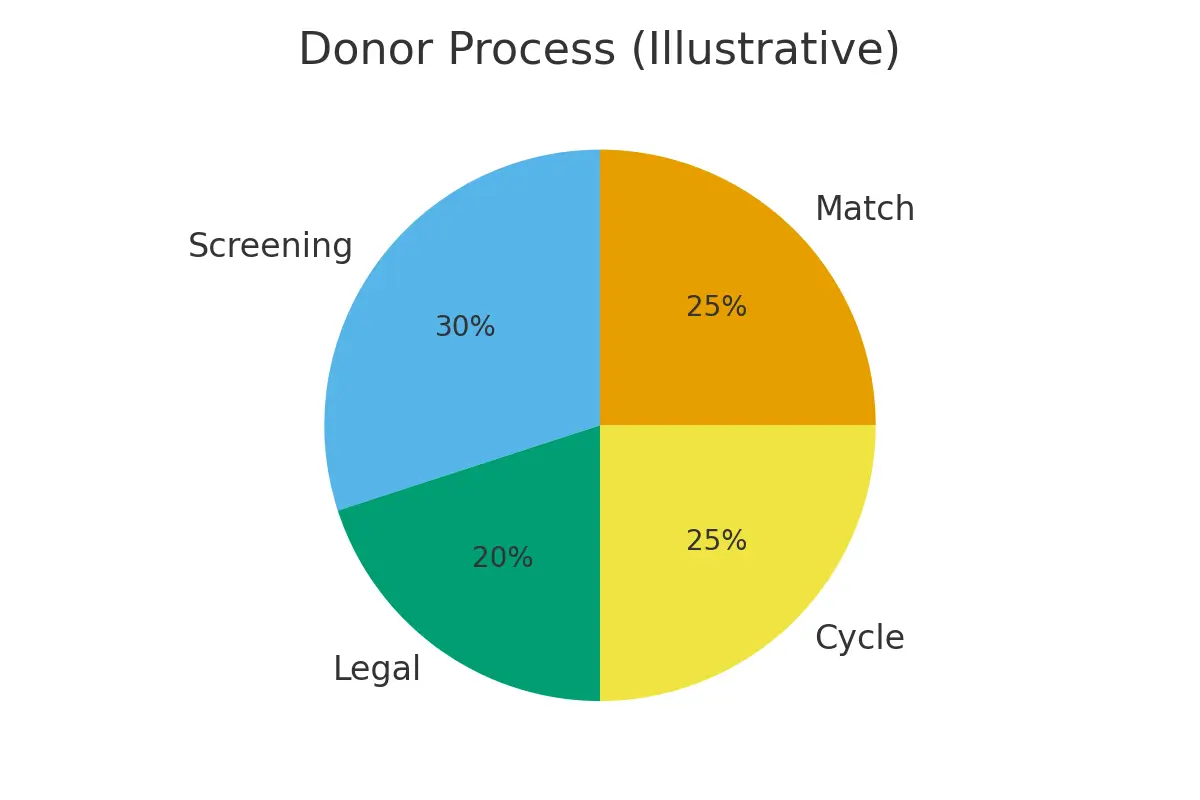
Donor stimulation is the process of using controlled ovarian hyperstimulation (COH) to help an egg donor produce multiple mature eggs in one cycle. Clinics adjust medication doses to optimize egg yield without compromising donor safety.
Where It Fits
- It comes after donor screening and before egg retrieval.
- It is the central step that determines embryo numbers, fertilization outcomes, and euploidy yield.
- It serves both medical and logistical goals—aligning lab schedules, donor availability, and intended parent planning.
Eligibility Signals — When to Start, Escalate, or Pause
Not every donor is immediately ready to begin stimulation. Clinics rely on several eligibility signals to decide when to proceed or recalibrate.
Start When These Signals Are Strong
- AMH between 2.0–6.0 ng/mL (suggests good ovarian reserve)
- AFC between 12–20+
- Regular menstrual cycles
- Normal baseline ultrasound
- Stable labs (TSH, infectious screening, CBC)
Escalate Monitoring When
- Estradiol rises quickly (risk of overstimulation)
- Follicles grow unevenly
- Cycle response lags behind expected benchmarks
Pause When
- A dominant follicle appears too early
- Estradiol stalls over several days
- Donor experiences side effects, needing reassessment
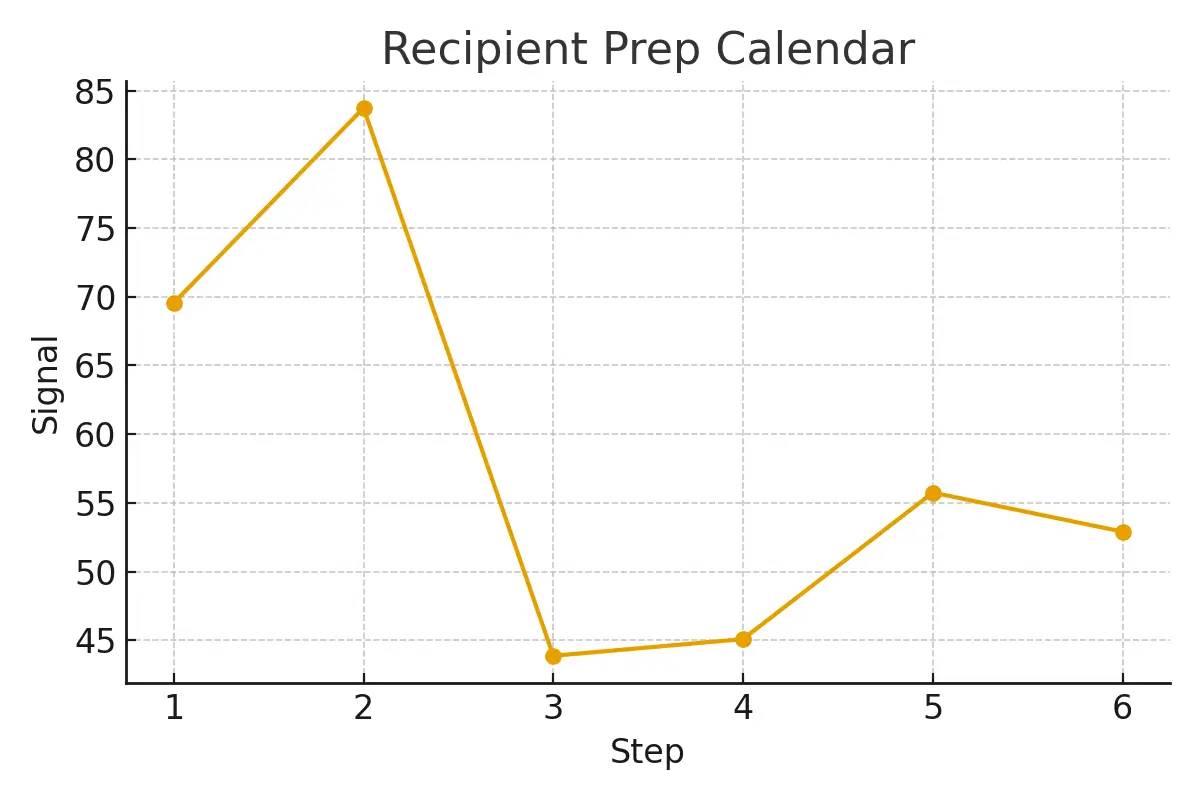
Step-by-Step Donor Stimulation Protocol with Timing Checkpoints
A donor stimulation cycle generally lasts 10–14 days from the first injection to the trigger shot. The following steps outline what happens at each checkpoint.
Step 1: Baseline Scan (Cycle Day 2 or 3)
- Checks for ovarian cysts
- Confirms hormone levels
- Approves protocol start
Step 2: Start of Medications (Day 2–3)
The donor begins FSH or HMG injections once daily.
Goal: Recruit multiple follicles evenly.
Step 3: First Monitoring Checkpoint (Day 5–6)
Clinic measures:
- Follicle count
- Follicle size
- Estradiol levels
Adjustments made for:
- Slow response → dose increase
- Fast response → dose decrease
Step 4: Mid-Cycle Monitoring (Day 7–10)
Follicles should reach 10–14 mm. Clinics add GnRH antagonist to prevent premature ovulation.
Step 5: Pre-Trigger Checkpoint
When leading follicles reach 17–18 mm, the clinic schedules the trigger shot.
Step 6: Trigger Shot
Typically, hCG or Lupron, given ~36 hours before retrieval.
Goal: Final follicle maturation → maximize egg quality.
Step 7: Egg Retrieval
A safe, 10–20-minute procedure under light anesthesia. High-quality cycles typically produce:
- 12–25 eggs, depending on donor profile.
Pros, Cons, and Practical Costs (With Line-Item Examples)
Pros
- High egg yield → Higher embryo numbers
- Predictability with proper monitoring
- Short timeline (2 weeks)
- Proven success rates
Cons
- Potential side-effects (bloating, mood changes)
- Need for daily injections
- Risk of mild ovarian hyperstimulation syndrome (OHSS)
- Coordinated scheduling required
Practical Cost Breakdown
| Line Item | Estimated Range |
| Donor Medications | $3,000–$6,000 |
| Donor Compensation | $8,000–$12,000 |
| Monitoring & Ultrasounds | $1,500–$3,000 |
| Egg Retrieval + Anesthesia | $2,000–$4,000 |
| Legal + Contracting | $800–$1,500 |
| Genetics / PGT | $2,000–$5,000 (optional) |
Realistic Total Per Cycle: $18,000–$30,000, depending on clinic and geography.
Outcome Drivers — What You Control vs. What You Monitor
Egg donor cycles have predictable patterns. Some factors you can influence, and others you simply watch.
What You Control
- Protocol type (antagonist most common)
- Medication dosing
- Trigger timing (critical for egg maturity)
- Pharmacy logistics (ensuring meds arrive on time)
- Legal and contract timelines
What You Monitor
- Estradiol trends
- Follicle growth uniformity
- Response to stimulation
- Endometrial prep for the recipient
- Lab capacity and retrieval day planning
Understanding these distinctions keeps cycles simple, safe, and efficient.
Questions to Ask Your Clinic
Come prepared with this list:
- How do you determine my donor’s starting medication dose?
- What is your typical egg yield for donors with similar AMH/AFC?
- How often will monitoring appointments be scheduled?
- What is your threshold for canceling or rescheduling a cycle?
- How do genetic testing decisions affect embryo quality?
- How transparent is your cost structure—are there hidden fees?
- What are your anesthesia protocols on retrieval day?
- How do you coordinate timing between donor stimulation and my embryo transfer?
Expert Quote
“Protect timing and keep plans simple—quality improves when noise goes down.” — Clinical Team
Patient Case Study
A couple from NYC entered treatment after inconclusive ovarian reserve tests. Their initial cycles were cluttered with late pharmacy deliveries, unclear communication, and unpredictable monitoring schedules.
When they switched providers, the clinic:
- Established a clear stimulation plan
- Improved timing control between donor and lab
- Simplified logistics around medication shipments
- Set transparent expectations
Testimonials
- “The steps finally made sense.” — A.&J., Manhattan
- “Costs were clear; no surprise bills.” — L., Hoboken
- “Nurses replied fast with practical coaching.” — K.&V., Queens
Additional Insights
- Pharmacy logistics escalate cumulative success by aligning timing between embryo and endometrial readiness.
- Cycle cancellation criteria rarely change predictability—but they prevent wasted cycles.
- Genetic testing decisions influence embryo selection more than total competency.
- Legal consent and contracts protect timelines and clarify expectations.
- Trigger timing drives euploidy yield by stabilizing the final maturation step.
- Endometrial preparation ensures transfer safety and planning accuracy.
Frequently Asked Questions (FAQs)
Q: Is this medical advice?
Ans : No. This guide helps you prepare productive conversations with your clinic.
Q: How many cycles should I plan?
Ans : Think in ranges. Cumulative success often requires 1–2 donor cycles, depending on goals.
Q: What drives cost most?
Ans : Medications, genetics, anesthesia, and the total number of cycles.
Next Steps with Surrogacy4All
If you’re ready to move forward, Surrogacy4All offers:
- Free 15-minute nurse consult (212) 661-7673
- Upload your labs for a second opinion
- Customized cost breakdown for your case
These tools simplify planning and ensure transparency every step of the way.
Conclusion
Understanding donor stimulation protocols—from eligibility and timing to safety and egg yield—empowers you to navigate the egg donation journey with clarity and control. When you protect timing, simplify steps, and choose a clinic that prioritizes transparency, your outcomes improve dramatically. Whether you’re an intended parent or a donor, the right protocol creates predictability, enhances embryo quality, and supports a humane, stress-reduced process.
With the right team and the right plan, your path through donor stimulation becomes not just manageable, but optimally effective.

Dr. Kulsoom Baloch
Dr. Kulsoom Baloch is a dedicated donor coordinator at Egg Donors, leveraging her extensive background in medicine and public health. She holds an MBBS from Ziauddin University, Pakistan, and an MPH from Hofstra University, New York. With three years of clinical experience at prominent hospitals in Karachi, Pakistan, Dr. Baloch has honed her skills in patient care and medical research.