When you’re starting your egg donation journey, one of the most crucial steps is donor screening. This process ensures that potential egg donors are medically, genetically, and psychologically fit to participate safely and effectively. Whether you’re a hopeful parent or a donor, understanding the details of these screenings helps align expectations, reduce risks, and improve success rates.
We’ll break down donor screening — medical, genetic, and psychological, explain who benefits, how timing affects outcomes, and provide realistic cost insights. We’ll also share a patient case study, expert advice, and questions to ask your clinic so you can make confident, informed decisions.
What Is Donor Screening and Why Is It Essential?
Donor screening is the comprehensive evaluation process that ensures egg donors meet health, genetic, and emotional readiness criteria. It helps clinics identify donors who can safely undergo ovarian stimulation and egg retrieval while ensuring the best possible outcomes for recipients.
Screening prevents genetic risks, reduces the likelihood of failed cycles, and promotes emotional well-being for both the donor and recipient. It’s a safeguard — for everyone involved — in the complex and sensitive process of assisted reproduction.
Where Donor Screening Fits in the Egg Donation Journey
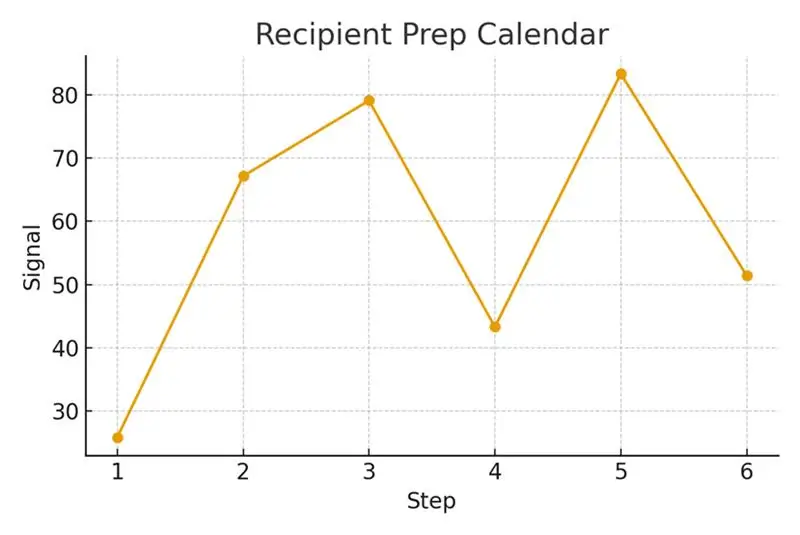
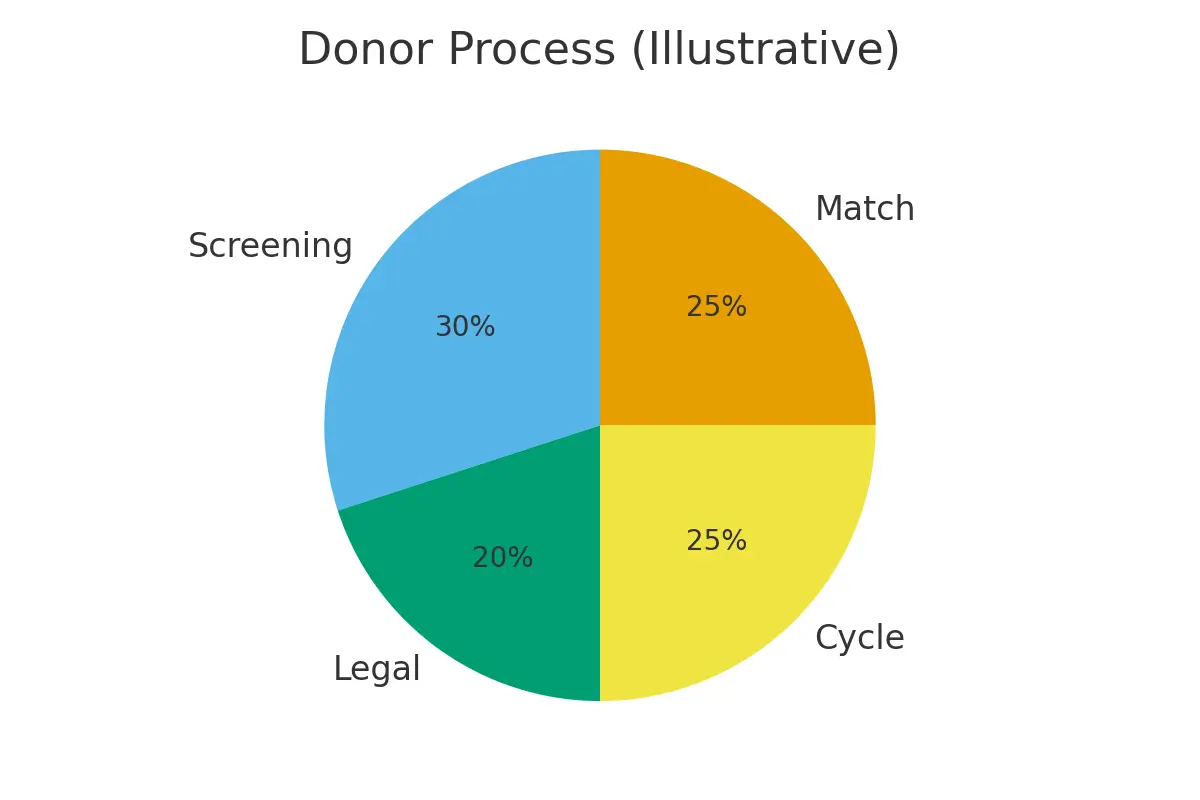
In the Egg Donation 101 pathway, donor screening typically occurs after the initial donor application but before final acceptance into a program. The sequence usually follows:
- Donor application and background check
- Medical and hormonal assessment
- Genetic screening
- Psychological evaluation
- Legal and consent process
- Cycle preparation and synchronization
Screening ensures the donor’s health aligns with the medical requirements of the intended parents’ fertility plan.
Step-by-Step Donor Screening Process
The donor screening journey usually unfolds over 4 to 6 weeks, depending on clinic coordination and test turnaround times. Each phase builds upon the previous one to ensure that only qualified and healthy donors progress to egg retrieval.
Step 1: Initial Application and Background Review (Week 1)
Purpose: To gather essential health and lifestyle information.
The donor completes an extensive medical and personal history questionnaire covering age, BMI, reproductive history, medications, lifestyle habits, and family medical background.
Timing Checkpoint:
- Completed within 3–5 days of application submission.
- Clinics review data and flag potential red flags (e.g., hereditary disorders or smoking).
Step 2: Medical and Fertility Screening (Weeks 1–2)
Purpose: To ensure the donor’s reproductive health and ability to safely undergo stimulation.
Tests include:
- Physical exam and pelvic ultrasound to assess ovaries and uterus.
- Blood tests for hormone levels (AMH, FSH, LH, Estradiol).
- Infectious disease testing (HIV, Hepatitis, Syphilis, CMV, etc.).
- Pap smear and urine analysis.
Timing Checkpoint:
- Results are typically available in 7–10 business days.
- If all results are normal, the donor is medically cleared to proceed.
Step 3: Genetic Carrier Screening (Weeks 2–3)
Purpose: To rule out inherited genetic risks.
Tests include:
- Expanded carrier panels for 100–500 conditions (e.g., Cystic Fibrosis, SMA, Thalassemia).
- Comparison of the donor’s genetic profile with the recipient’s or sperm provider’s.
Timing Checkpoint:
- Testing takes about 1–2 weeks.
- A genetic counselor reviews fertility results and discusses implications.
Step 4: Psychological Evaluation (Weeks 3–4)
Purpose: To ensure the donor’s mental and emotional stability throughout the process.
Evaluation includes:
- Interview with a psychologist to discuss motivations, understanding of the process, and support system.
- Standardized psychological tests like the MMPI or PAI.
Timing Checkpoint:
- Can be scheduled as soon as medical tests are complete.
- Typically completed in 1–2 sessions.
Step 5: Legal Counseling and Consent (Week 5)
Purpose: To ensure full understanding of rights, responsibilities, and confidentiality.
- Anonymity or identity disclosure preferences.
- Compensation terms and payment schedule.
- Future contact agreements, if applicable.
Timing Checkpoint:
- Usually completed in 3–5 days with a fertility attorney.
Step 6: Final Coordination and Cycle Preparation (Weeks 5–6)
Purpose: To align the donor’s cycle with the recipient’s treatment plan.
Tasks include:
- Scheduling medication start dates.
- Baseline ultrasound and bloodwork.
- Confirming final medical clearance.
Timing Checkpoint:
- The fertility nurse coordinates the donor’s stimulation start date.
- Embryo retrieval is typically scheduled 10–14 days after stimulation begins.
Pros and Cons of Donor Screening
Every medical process has its advantages and limitations. Here’s a transparent view to help you plan realistically.
Pros
- Ensures safety and health: Detects underlying conditions before egg retrieval.
- Reduces genetic risks: Prevents hereditary conditions in offspring.
- Builds emotional readiness: Psychological screening fosters donor stability.
- Improves success rates: Healthier donors yield higher-quality eggs.
- Predictable outcomes: Structured timing reduces logistical errors.
- Boosts trust: Legal documentation ensures clarity and protection for all parties.
Cons
- Time-consuming: The process can take 4–6 weeks before stimulation starts.
- Costs may vary: Each clinic’s pricing model differs, and not all tests are bundled.
- Possible disqualification: Donors with medical or genetic abnormalities may be rejected.
- Emotional intensity: Psychological discussions can be uncomfortable for some donors.
- Administrative delays: Labs or legal approvals can occasionally slow progress.
Practical Cost Breakdown of Donor Screening
Here’s a detailed line-item estimate for donor screening expenses (based on U.S. fertility clinic averages):
| Screening Component | Details | Estimated Cost (USD) |
| Initial Application & Background Check | Administrative processing and ID verification | $100 – $300 |
| Medical & Fertility Testing | Hormone levels, ultrasound, STI screening | $500 – $1,000 |
| Genetic Carrier Screening | Expanded panel (100–500 conditions) | $300 – $1,500 |
| Psychological Evaluation | Clinical interview and standardized testing | $250 – $500 |
| Legal Counseling & Consent | Fertility law consultation and contract signing | $200 – $400 |
| Cycle Coordination Costs | Nurse scheduling, administrative support | $150 – $300 |
Outcome Drivers You Control vs. Those You Monitor
You Control:
- Selecting a reputable clinic
- Ensuring the donor completes all screenings
- Prioritizing clear communication and timely follow-ups
You Monitor:
- Donor’s biological response to medications
- Lab quality metrics and embryo grading
- Timing of trigger shots and retrieval
Questions to Ask Your Clinic
Before you begin, clarify these essential points:
- What specific medical and genetic panels do you use?
- How often are donor health screenings updated?
- Who covers the cost of failed or incomplete screenings?
- Are donors psychologically evaluated by licensed professionals?
- What’s the average time from screening to cycle approval?
- How do you handle genetic carrier matches?
Expert Quote:
“Protect timing and keep plans simple — quality improves when noise goes down.”
— Clinical Team
Real-Life Case Study
A couple from NYC struggled with repeated delays due to incomplete donor screening. Their clinic recommended aligning logistics and expectations early. By ensuring the donor completed medical, genetic, and psychological testing simultaneously, they shortened preparation time by 30%. The result? A successful retrieval, clear communication, and predictable scheduling that boosted confidence for all parties involved.
Testimonials:
- “The steps finally made sense.” — A. & J., Manhattan
- “Costs were clear; no surprise bills.” — L., Hoboken
- “Nurses replied fast with practical coaching.” — K. & V., Queens
Additional Insights
Understanding advanced fertility concepts can help patients and clinics improve success rates and reduce uncertainty in the egg donation process. Below are key insights, simplified into clear bullet points for better understanding:
- Diagnostic accuracy thresholds: Increase live-birth probability by minimizing delays in diagnosis and treatment planning. Accurate testing ensures that only qualified donors and recipients proceed, saving both time and cost.
- Frozen embryo transfer (FET): Synchronizes euploidy yield (chromosomally normal embryos) by matching the timing between the embryo and endometrial lining. This careful alignment enhances implantation success and cycle predictability.
- Lab quality indicators: Have minimal direct effect on live-birth probability but are vital for reducing variability in critical embryology steps. Consistent laboratory standards stabilize outcomes across multiple cycles.
- Embryo competency optimization: FET simplifies embryo competency testing by setting clear escalation thresholds. Clinics can decide quickly which embryos to prioritize or freeze, reducing indecision and improving time management.
- Trigger timing precision: Balances live-birth probability by aligning ovulation triggers with biological readiness. Transparent pricing models and scenario planning ensure patients know exactly what to expect for each cycle.
- Male factor optimization: Enhances cumulative success rates by synchronizing sperm quality benchmarks with biological cutoffs. Integrating lab data with donor screening reduces mismatch risks and improves fertilization outcomes.=
Frequently Asked Questions (FAQs)
Q: Is this medical advice?
Ans: No — this information is for educational purposes only. Always consult your fertility specialist before making decisions.
Q: How many donor cycles should I plan for?
Ans: Think in ranges, cumulative success — not a single cycle — determines final outcomes.
Q: What drives costs most?
Ans: Major cost drivers include genetic testing, medications, anesthesia, and the total number of cycles.
Next Steps with Surrogacy4All
If you’re ready to move forward, Surrogacy4All offers:
- Free 15-minute nurse consult (212) 661-7673
- Upload your labs for a second opinion
- Customized cost breakdown for your case
These tools simplify planning and ensure transparency every step of the way.
Conclusion
Donor screening — medical, genetic, and psychological — forms the backbone of safe, ethical, and effective egg donation. It minimizes risks, ensures donor and recipient compatibility, and lays the foundation for healthy outcomes.
By focusing on timing, simplicity, and transparency, you can turn a complex process into a manageable journey with predictable results. Whether you’re donating eggs or building a family, knowledge and preparation empower better choices — and that’s where success truly begins.

Dr. Kulsoom Baloch
Dr. Kulsoom Baloch is a dedicated donor coordinator at Egg Donors, leveraging her extensive background in medicine and public health. She holds an MBBS from Ziauddin University, Pakistan, and an MPH from Hofstra University, New York. With three years of clinical experience at prominent hospitals in Karachi, Pakistan, Dr. Baloch has honed her skills in patient care and medical research.