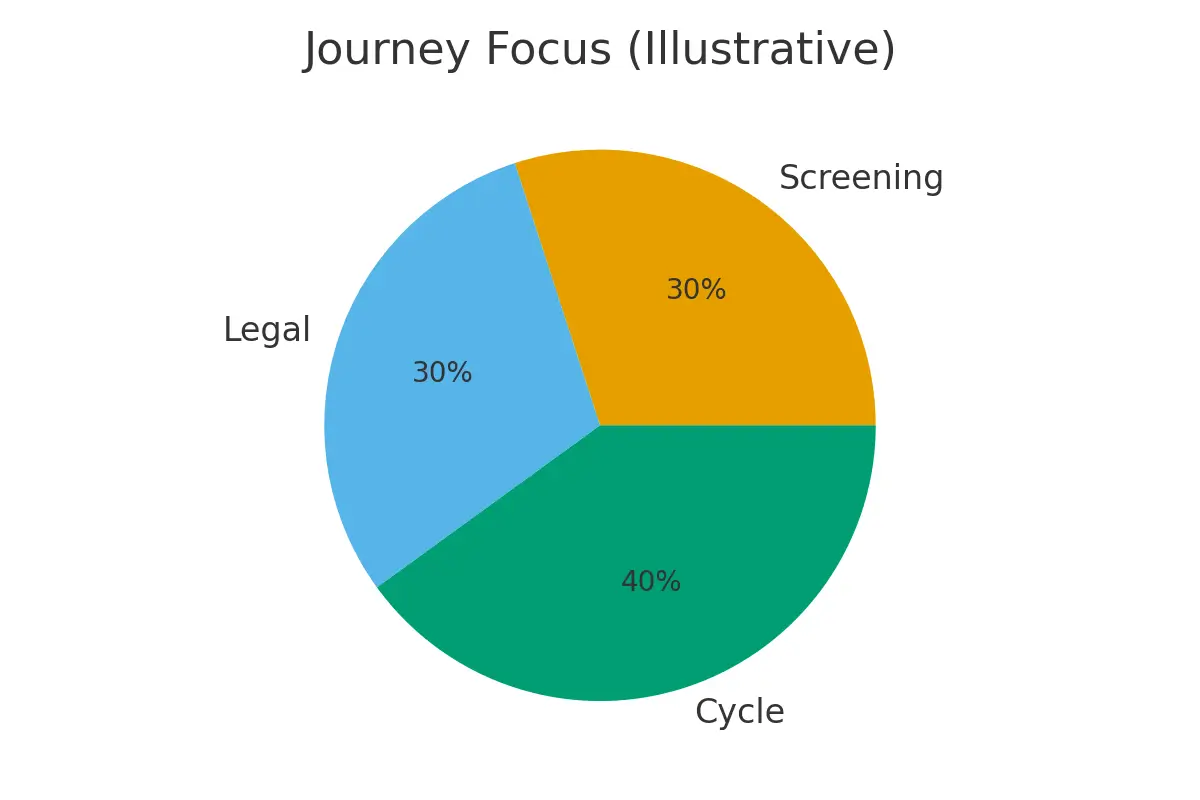
This guide explains how donor limits, reporting rules, and legal/health safeguards shape your donor-egg, donor-sperm, or donor-embryo pathway. These factors directly affect availability, sibling planning, long-term access, and your overall predictability—so you can move forward with clarity instead of surprises.
What It Is
Donor Limits & Reporting — in plain English
Every donor program must follow rules that protect both families and future children. These include:
- Family limits: A maximum number of families per donor (to reduce accidental consanguinity).
- Geographic limits: Some programs cap by country, state, or population size.
- Medical reporting: Requirements for updating donor medical histories and notifying families of new, relevant conditions.
- Usage tracking: How clinics track vials, eggs, or embryos across cycles.
- Legal rights: What you can and cannot request (re-order rights, sibling access, future contact rules).
- Health follow-up: How donors are screened, re-screened, and how new findings are reported.
These rules shape embryo numbers, future sibling planning, donor access, and your ability to reorder materials later.
Who It Helps
This guide is especially useful if you want transparency, predictability, and legal-medical certainty.
Strong Fit
- Families who want genetically linked siblings and need to ensure future donor access
- Individuals using donor sperm where vial supply is limited or selling out quickly
- Anyone using donor eggs where cohort size affects embryo numbers and family planning
- Users of donor embryos who need clarity on cohort limits and legal structure
- Parents who want long-term medical reporting for genetic conditions
Consider a Modified Path If
- You’re flexible about donors and don’t require the same donor for siblings
- You cannot commit to long-term storage or future purchase rights
- The donor program cannot guarantee reporting or follow-up
- There are signs the donor may reach family limits soon
- Your clinic cannot track donor usage across multiple sites
Step-by-Step
A simple sequence with timing checkpoints to protect outcomes and reduce stress
-
Confirm the Donor’s Current Status
-
Families created so far
-
Remaining slots before family limits
-
Reorder availability (vials, eggs, embryos)
-
-
Secure Future Access (If Sibling Planning Matters)
-
Buy extra sperm vials
-
Purchase a full donor-egg cohort
-
Choose donor-embryo sets with enough embryos upfront
-
-
Review Medical Reporting Policies
-
How new donor medical issues are reported
-
How often donors are re-screened
-
Whether updates are guaranteed (and for how long)
-
-
Clarify Legal Agreements
-
Rights to purchase more material later
-
Use of stored embryos if the donor retires
-
Disclosure and identity-release rules
-
-
Document Everything
-
Storage terms
-
Transfer rights
-
Embryo disposition options
-
Timeline for reporting obligations
-
-
Reassess Before Transfer
-
Updated donor health updates (if available)
-
Confirm compliance with ICMR/FDA rules
-
Check donor status for family limits if using additional materials
-
Pros & Cons
A balanced, realistic view to set expectations
Pros
- Protects long-term sibling planning
- Limits genetic-related risks (via family caps)
- Provides ongoing medical updates that improve child health guidance
- Avoids donor sell-outs that disrupt future cycles
- Strengthens legal clarity and reduces future disputes
Cons
- Some donors hit family limits quickly → reduced access
- Reporting systems vary greatly across programs
- Upfront purchase may be required to secure future rights
- Geographic limits may restrict transfers or moving embryos
- Legal and storage paperwork can feel heavy or complex
Costs & Logistics
What to expect, what needs authorization, and how to avoid surprise bills
Typical Line Items
- Donor material (eggs, sperm vials, embryo cohort)
- Legal fees for donor agreements
- Storage fees (annual or multi-year)
- Shipping/transport of gametes or embryos
- Additional screening if required by new clinics or regulators
- Admin charges for record retrieval or reports
Prior Authorizations
Some insurers require:
- Proof of medical necessity
- Donor consent documentation
- Lab certifications
- Updated infectious-disease panels
Cash-Flow Scenarios
- Buy donor material now + delay treatment
- Bank embryos first, store for sibling planning
- Spread purchases over multiple cycles
- One-time cohort purchase vs. vials-as-you-go
Tracking to Prevent Surprise Bills
Make a simple list of:
- What is prepaid (donor lot, cohort fee)
- What renews annually (storage)
- What is per-cycle (retrievals, ICSI, PGT)
- What increases over time (storage or transport fees)
What Improves Outcomes
What actually changes results vs. what rarely helps
Actions That Truly Move the Needle
- Securing donor material early before limits are reached
- Choosing programs with strong reporting and transparent family caps
- Banking enough embryos upfront if sibling genetics matter
- Checking storage, legal rights, and transfer permissions early
- Reviewing donor medical updates before each new pregnancy
Actions That Rarely Help
- Hoping donor availability remains stable without securing material
- Assuming donors stay under limits indefinitely
- Buying too few vials or too small an egg cohort
- Excessive add-on tests without clear indication
- Switching clinics mid-process without understanding reporting portability
Case Study
From uncertainty to a clear plan using steady communication and defined thresholds
A single parent using donor sperm had one child and wanted a second in a few years. The donor bank reported that the donor was close to the family limit.
What they did:
- Requested donor usage numbers and limit thresholds.
- Purchased additional vials to secure future access.
- Banked embryos now to avoid donor sell-out.
- Documented the donor’s reporting obligations and long-term medical update policy.
- Stored embryos at a facility with transparent transfer rights.
Outcome:
A predictable sibling plan with the same donor, no risk of family-limit closure, and clear medical reporting for future health decisions.
Mistakes to Avoid
- Assuming donor material will always be available
- Not checking family limits early
- Ignoring medical-update policies
- Failing to secure re-order rights in writing
- Banking too few embryos for sibling goals
- Changing clinics without confirming reporting compatibility
- Waiting until after the first child to think about donor access
FAQs
Q: What is a family limit?
Ans : A cap on the number of families a donor can contribute to. Once reached, no new purchases are allowed.
Q: Why do donors sell out even if limits aren’t reached?
Ans : Some donors have limited batches or retire early; limits don’t guarantee availability.
Q: Will I be notified if the donor develops a new health condition?
Ans : Only if the program has a structured medical-update policy—ask for this in writing.
Q: Can I reserve materials for a second child?
Ans : Yes. Many programs allow buying vials/cohorts upfront or holding them in storage.
Q: Do limits differ for sperm vs eggs vs embryos?
Ans : Yes. Sperm donors often have stricter limits; egg donors are limited by cohort size; donor embryos are fixed.
Next Steps
- Free 15‑min nurse consult
- Upload labs
- Cost breakdown for your case.
Related Links

Dr. Kulsoom Baloch
Dr. Kulsoom Baloch is a dedicated donor coordinator at Egg Donors, leveraging her extensive background in medicine and public health. She holds an MBBS from Ziauddin University, Pakistan, and an MPH from Hofstra University, New York. With three years of clinical experience at prominent hospitals in Karachi, Pakistan, Dr. Baloch has honed her skills in patient care and medical research.





