Understanding donor egg success rates is essential for anyone navigating fertility care, especially within the Egg Donation 101 pathway. Whether you’re a patient, partner, or support person, decoding the data empowers you to make thoughtful decisions. This guide is designed to help you read real-world outcomes, understand timing, spot eligibility signals, assess practical costs, and ask the right questions. The goal: keep care simple, humane, predictable, and effective.
In this comprehensive word guide, we go deep into how success rates work, what truly influences them, and how you can use this information to confidently plan your journey.
Understanding Donor Egg Success Rates: Definitions and Where This Fits in Your Journey
Before reading the numbers, it’s essential to understand what success rate actually means in donor-egg cycles.
What Is a Donor Egg Success Rate?
A donor egg success rate refers to the likelihood that a cycle using donated eggs results in:
- A high-quality embryo
- A successful embryo transfer
- A confirmed pregnancy
- A live birth
Different clinics report different points along this chain. The most reliable metric is live birth rate per embryo transfer, but cumulative success across multiple transfers is even more meaningful.
Where Does This Fit in the Egg Donation Journey?
Your pathway includes:
- Eligibility and pre-cycle evaluation
- Donor selection
- Egg retrieval
- Fertilization and embryo culture
- Embryo transfer
- Pregnancy monitoring
Eligibility Signals and When to Escalate or Pause
Success begins before the first medication dose.
Who Typically Benefits Most From Donor Eggs?
You may be a strong candidate if you have:
- Diminished ovarian reserve (very low AMH, high FSH)
- Repeated failed IVF cycles with your own eggs
- Genetic conditions that make using your own eggs risky
- Advanced maternal age
- Primary ovarian insufficiency
- Cancer treatment-related fertility decline
When to Escalate to Donor Eggs
Clinicians typically recommend moving to donor eggs when:
- Repeated stimulation cycles produce few or no usable eggs
- Embryo quality remains poor despite optimized protocols
- Genetic screening repeatedly identifies abnormalities
- You need predictability in success odds and timelines
When to Pause or Reassess
A pause may be wise if:
- Lab results are incomplete or inconsistent
- You are uncertain about the emotional implications
- Financial planning isn’t set
- You feel rushed or overwhelmed
Clear eligibility signals improve success rates because they simplify decision-making.
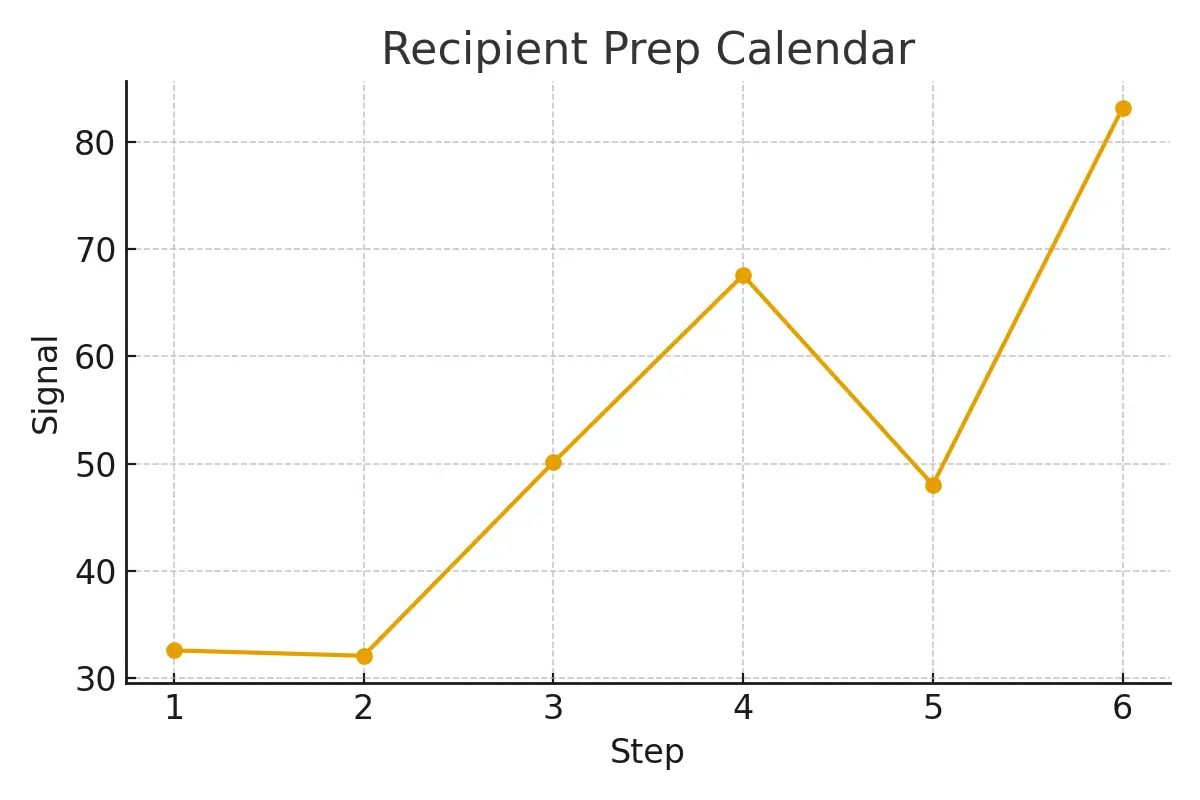
Step-by-Step Process With Timing Checkpoints
Knowing exactly what happens—and when—helps reduce stress and miscommunications.
Step 1: Consultation & Diagnostic Review
Timeline: 1–2 weeks
You’ll review labs, past cycle data, genetic history, donor options, and your care plan.
Step 2: Donor Selection
Timeline: 1–4 weeks
Choose from:
- Fresh donor cycles
- Frozen donor eggs
- Known donors
The timing depends on donor availability and your clinic’s matching protocol.
Step 3: Cycle Synchronization (For Fresh Donor Eggs)
Timeline: 2–4 weeks
Your uterus and the donor’s retrieval timeline must align.
Step 4: Donor Stimulation & Egg Retrieval
Timeline: 10–14 days
The donor takes medications, undergoes monitoring, and completes retrieval.
Step 5: Fertilization & Embryo Culture
Timeline: 5–7 days
Your eggs are fertilized, usually via ICSI, and embryos grow to the blastocyst stage.
Step 6: PGT-A Testing (Optional)
Timeline: 1–2 weeks
Embryos can be genetically screened to assess chromosomal normality.
Step 7: Uterine Preparation & Embryo Transfer
Timeline: 2–3 weeks
You begin the lining preparation and transfer a fresh or frozen embryo.
Step 8: Pregnancy Confirmation
Timeline: 10–14 days post-transfer
Timing impacts outcomes. Clinics that streamline logistics typically show higher success rates.
Pros, Cons, and Practical Costs (With Line-Item Examples)
Advantages of Donor Eggs
- Higher success rates, especially for women 40+
- Genetically normal embryos more consistently
- Predictable cycle timing
- Lower miscarriage risk
- Ability to carry the pregnancy yourself
Drawbacks to Consider
- Lack of genetic connection to the child
- Emotional and psychological adjustment time
- Costs are generally high
- Donor availability may vary
- Legal considerations if using a known donor
Typical Cost Breakdown
Costs vary by region, clinic, and donor type. Below is a realistic example:
| Cost Component | Estimated Range |
| Donor compensation | $8,000 – $20,000 |
| Donor medical screening | $1,500 – $3,000 |
| IVF cycle & monitoring | $12,000 – $20,000 |
| Egg retrieval & anesthesia | $3,000 – $8,000 |
| Medications (donor + recipient) | $5,000 – $10,000 |
| Legal agreements | $800 – $2,000 |
| Embryo culture & ICSI | $2,000 – $6,000 |
| PGT-A testing | $2,000 – $6,000 |
| Frozen embryo transfer | $3,000 – $6,000 |
Total cost range: $35,000 – $70,000+
You pay most for medications, genetic testing, anesthesia, and the number of cycles you complete.
Outcome Drivers You Control vs. Those You Monitor
Understanding what influences your success rate helps you take meaningful action.
Factors You Can Control
- Choosing a reputable clinic with verified lab data
- Ensuring complete diagnostics before starting
- Following medication instructions closely
- Lifestyle factors (sleep, stress, nutrition)
- Transfer timing—do not rush uterine preparation
- Single vs. multiple embryo transfer decisions
Factors You Only Monitor
- Donor’s egg quality
- Sperm quality
- Embryo development patterns
- Lab culture conditions
- Genetic screening results
Clinics with streamlined lab-to-transfer processes reduce delays, improving embryo survival and pregnancy outcomes.
Questions to Ask Your Clinic
Before committing to donor eggs, ask:
- What is your live birth rate per donor egg transfer?
- Do you report cumulative success per cohort of eggs?
- What standard is used for donor screening?
- How are donor medications dosed to reduce risk?
- What is the timeline from donor match to transfer?
- What is included—and not included—in your pricing?
- How often will nurses respond during the cycle?
Expert Insight
“Protect timing and keep plans simple—quality improves when noise goes down.” — Clinical Team
Patient Case Study
A couple from NYC experienced months of inconclusive diagnostics, which led to inconsistent medication plans and unpredictable results.
When they shifted to a streamlined donor-egg pathway:
- Their clinic aligned all diagnostics
- They received a clean step-by-step timeline
- Costs were pre-explained with no hidden fees
- They were matched with a donor quickly
- Their embryo transfer occurred on schedule
A successful pregnancy and a calmer, more predictable experience.
Patient Testimonials
“The steps finally made sense.” — A.&J., Manhattan
“Costs were clear; no surprise bills.” — L., Hoboken
“Nurses replied fast with practical coaching.” — K.&V., Queens
Additional Clinical Insights
Modern clinics optimize success by focusing on the following principles:
Embryo Culture Optimization
Minimizing transport and delays during culture helps maintain embryo quality.
Diagnostic Accuracy
Over-testing can undermine predictability by delaying or confusing dosing decisions.
Cycle Cancellation Criteria
Clear criteria keep risks (like multiples) controlled and let patients budget with confidence.
Single-Embryo Transfer Policies
While safer, overly strict policies may reduce implantation odds for certain cases unless properly explained and planned.
Luteal Support
Well-structured luteal support:
- Improves cumulative success
- Creates budget certainty
- Ensures clear escalation thresholds
The goal of every clinic should be to balance patient experience with high-quality outcomes.
Frequently Asked Questions (FAQs)
Q: Is this medical advice?
Ans : No. This is educational guidance to help you have informed conversations with your clinic.
Q: How many cycles should I plan?
Ans : Think in ranges. Cumulative success—often 1–3 cycles—tells the true story.
Q: What drives cost most?
Ans : Medications, genetics, anesthesia, and how many cycles you complete.
Next Steps — Surrogacy4All
- Free 15-minute nurse consult (212) 661-7673
- Upload your labs for a second opinion
- Get a personalized cost breakdown for your exact case
Conclusion
Decoding donor egg success rates is about more than numbers. It requires understanding eligibility, timing, emotional readiness, financial planning, and clinical practices that truly drive outcomes. With the right clinic, clear timelines, and informed expectations, donor egg IVF becomes predictable, humane, and scientifically grounded.
Use this guide to ask better questions, avoid unnecessary delays, and choose a plan that supports both your goals and your wellbeing.

Dr. Kulsoom Baloch
Dr. Kulsoom Baloch is a dedicated donor coordinator at Egg Donors, leveraging her extensive background in medicine and public health. She holds an MBBS from Ziauddin University, Pakistan, and an MPH from Hofstra University, New York. With three years of clinical experience at prominent hospitals in Karachi, Pakistan, Dr. Baloch has honed her skills in patient care and medical research.