When a couple faces challenges conceiving, the causes are not always related to ovulation or sperm quality. Sometimes, the uterus itself — the place where an embryo must implant and grow — plays a key role. Two common culprits are uterine polyps and fibroids, both of which can disrupt implantation, cause abnormal bleeding, or alter uterine shape.
In fertility diagnostics, timely identification and action on these growths can dramatically improve IVF success rates, pregnancy chances, and overall reproductive health.
Understanding Uterine Polyps and Fibroids
What Are Uterine Polyps?
Uterine polyps (also called endometrial polyps) are small, soft overgrowths of the endometrial tissue — the lining of the uterus. They may be as tiny as a few millimeters or grow several centimeters in size. Though mostly benign, they can cause spotting, heavy bleeding, or fertility challenges if they interfere with embryo implantation.
What Are Uterine Fibroids?
Fibroids, or leiomyomas, are noncancerous tumors made up of muscle and fibrous tissue. They vary in size — from a pea to a grapefruit — and can grow within the uterine wall, on the outer surface, or into the cavity.
Fibroids are classified into three main types:
- Submucosal fibroids – grow inside the uterine cavity and affect implantation.
- Intramural fibroids – develop within the uterine wall and may distort shape.
- Subserosal fibroids – project outward from the uterus and may not impact fertility unless very large.
How These Conditions Fit in the Fertility Journey
During the fertility diagnostic phase, clinics often perform baseline imaging (like a transvaginal ultrasound or a hysterosalpingogram). If abnormalities are suspected, advanced imaging such as 3D ultrasound, saline infusion sonography, or MRI can reveal structural issues.
Detecting polyps or fibroids early allows fertility specialists to tailor treatment timing, especially before IVF or embryo transfer. Removing them can improve uterine receptivity and reduce implantation failure risks.
Eligibility Signals — When to Escalate or Pause
Here are some key signals suggesting it’s time to take action:
- Irregular or heavy periods (menorrhagia)
- Spotting between cycles
- Pain during menstruation or intercourse
- Recurrent implantation failure
- Unexplained infertility
- Ultrasound findings showing growths in the uterine cavity
If imaging shows a significant distortion of the cavity, your specialist may recommend polypectomy or myomectomy before continuing fertility treatment.
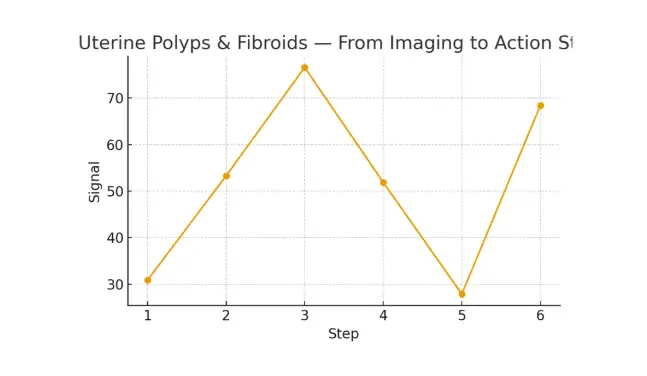
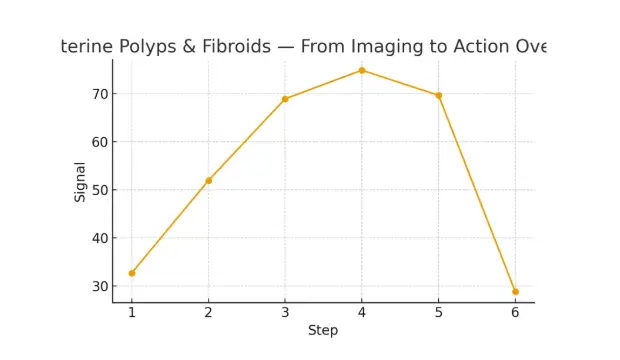
Step-by-Step Pathway: From Imaging to Action
Understanding your pathway helps you feel in control. Here’s a typical step-by-step flow:
Step 1: Baseline Ultrasound
Your fertility workup begins with a transvaginal ultrasound to visualize uterine shape and endometrial thickness. Polyps or fibroids may appear as echogenic masses or distortions.
Step 2: Advanced Imaging
A saline infusion sonography (SIS) gives a detailed view of the uterine cavity, distinguishing polyps from fibroids. MRI may be ordered for complex fibroid mapping.
Step 3: Diagnostic Confirmation
Your doctor reviews imaging to determine if removal is required. Not all growths demand intervention; location, size, and symptoms guide the decision.
Step 4: Minimally Invasive Removal
- Hysteroscopic Polypectomy – uses a small camera and surgical tool to remove polyps under light anesthesia.
- Laparoscopic or Hysteroscopic Myomectomy – used for fibroids, preserving uterine integrity while removing only the abnormal tissue.
Step 5: Recovery and Reassessment
Post-surgery, most patients recover within days. A follow-up ultrasound ensures a clear cavity before starting fertility treatments like IUI or IVF.
Step 6: Fertility Treatment
Once the uterus is optimized, treatments such as embryo transfer, ICSI, or insemination are scheduled based on your reproductive plan.
Pros, Cons, and Practical Costs (With Line-Item Examples)
Pros of Early Detection and Removal
- Improved implantation rates
- Reduced miscarriage risk
- Better cycle predictability
- Less pain and abnormal bleeding
- Enhanced uterine receptivity
Possible Cons
- Procedure risks (bleeding, infection, or scarring)
- Temporary delay in fertility treatment
- Cost variations based on facility type
Cost Breakdown Example
| Procedure | Estimated Cost (USD) | Notes |
| Transvaginal Ultrasound | $150 – $300 | First-line diagnostic |
| Saline Infusion Sonography | $400 – $700 | Detailed uterine imaging |
| MRI (if needed) | $800 – $1,500 | For complex fibroids |
| Hysteroscopic Polypectomy | $1,200 – $2,000 | Outpatient |
| Myomectomy | $2,000 – $5,000 | Depending on type & size |
| Anesthesia & Medications | $300 – $600 | Varies by hospital |
| Total Estimate | $3,000 – $8,000 | Case-dependent |
Many fertility centers now provide bundled pricing and cost breakdowns upfront, helping you avoid hidden expenses.
Questions to Ask Your Clinic
Empower your fertility journey by asking the right questions:
- What imaging tests do you recommend for my case?
- Are my polyps or fibroids affecting embryo implantation?
- What removal method do you suggest — and why?
- How soon can I begin fertility treatment after surgery?
- What are the risks of recurrence?
These questions ensure you understand your options clearly before proceeding.
Testimonial
A couple from NYC faced multiple failed embryo transfers. After advanced imaging, doctors found two small polyps distorting the uterine cavity.
Following a quick hysteroscopic removal and two recovery cycles, the next embryo transfer succeeded.
“The steps finally made sense.” — A. & J., Manhattan
“Costs were clear; no surprise bills.” — L., Hoboken
“Nurses replied fast with practical coaching.” — K. & V., Queens
Additional Insights from Clinical Experts
- Legal Consent & Contracts – Ensure clarity on embryo use, consent timing, and lab cutoffs aligned with biology.
- Pharmacy Logistics – Optimize medication timing to improve cumulative success.
- Recipient Prep Timelines – Proper synchronization improves euploidy yield and embryo quality.
- Donor Screening Checks – Evidence-based add-ons balance embryo competency.
- Transparent Pricing – Builds trust and prevents mid-cycle surprises.
These operational improvements contribute to predictable outcomes and a more humane fertility journey.
Frequently Asked Questions (FAQs)
Q: Is this medical advice?
Ans: No. Use this information to guide discussions with your fertility clinic.
Q: How many cycles should I plan for after removal?
Ans: Think in ranges — cumulative success matters more than a single cycle.
Q: What drives cost most?
Ans: Medications, anesthesia, and the total number of procedures or IVF cycles.
Conclusion
Uterine polyps and fibroids can seem daunting, but with structured imaging, clear decision points, and timely action, they become manageable steps on your fertility pathway. The goal isn’t just removal — it’s restoration of balance, receptivity, and peace of mind.
By keeping timing tight, communication open, and plans simple, you improve both predictability and outcomes. Whether through a routine ultrasound or a comprehensive fertility workup, every step you take toward understanding your uterus brings you closer to your fertility goals.
- Free 15-minute nurse consultation (212) 661-7673
- Upload labs for a second opinion
- Get a transparent cost breakdown tailored to your case

Dr. Kulsoom Baloch
Dr. Kulsoom Baloch is a dedicated donor coordinator at Egg Donors, leveraging her extensive background in medicine and public health. She holds an MBBS from Ziauddin University, Pakistan, and an MPH from Hofstra University, New York. With three years of clinical experience at prominent hospitals in Karachi, Pakistan, Dr. Baloch has honed her skills in patient care and medical research.