When beginning your fertility journey, understanding the right diagnostic tests can make all the difference in identifying the best treatment plan. Two commonly used uterine tests — HSG (Hysterosalpingogram) and Sonohysterogram (SHG) — play a vital role in evaluating reproductive health before or during IVF and other fertility treatments.
This article breaks down the differences between HSG and Sonohysterogram, who benefits most, when to schedule each test, realistic costs, and how these diagnostics fit within your patient journey in NYC’s fertility landscape.
Understanding the Tests
What Is an HSG (Hysterosalpingogram)?
An HSG is a specialized X-ray procedure that assesses the fallopian tubes and uterine cavity. A contrast dye is gently injected into the uterus through the cervix, and X-ray imaging captures how the dye flows through the reproductive tract.
Purpose:
- Detects blockages in the fallopian tubes.
- Evaluates the shape and contour of the uterus.
- Helps determine readiness for conception or IVF cycles.
What Is a Sonohysterogram (Saline Infusion Sonography)?
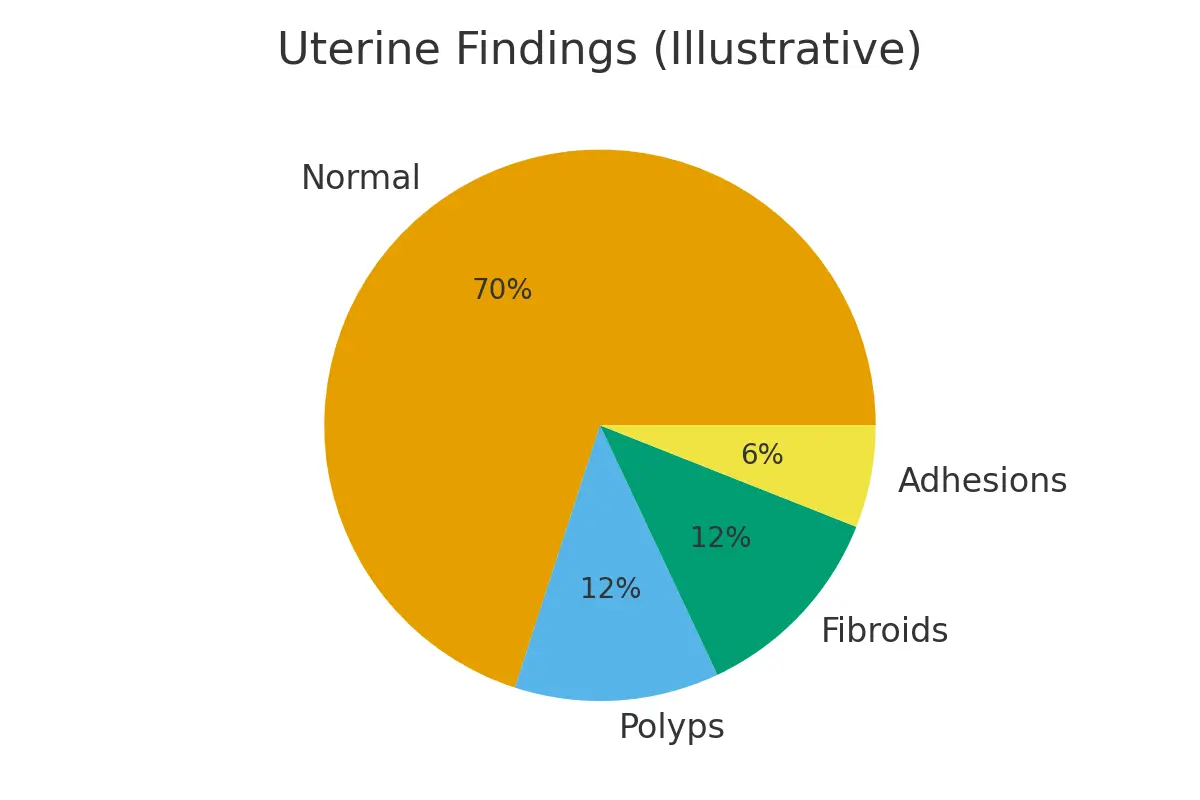
A Sonohysterogram, or SHG, uses ultrasound imaging combined with sterile saline to visualize the uterine lining in detail. It helps identify uterine abnormalities such as polyps, fibroids, or scarring.
Purpose:
- Assesses uterine lining health.
- Detects structural issues affecting fertility.
- Guides decisions for surgery or pre-IVF optimization.
Where These Tests Fit in the Fertility Journey
Both HSG and Sonohysterogram are typically performed early in the fertility testing and diagnostics process — often before beginning IVF or other assisted reproductive treatments.
- HSG: Determines if egg and sperm can meet naturally by assessing tubal openness.
- SHG: Determines if the uterine environment can successfully host an embryo.
Together, these tests provide a complete view of reproductive readiness — from pathways of conception to implantation potential.
Eligibility and When to Schedule
Who Should Get an HSG?
Women who’ve been trying to conceive for over a year (or six months if over 35) often start with an HSG to rule out tubal blockages. It’s also recommended after pelvic infections, surgeries, or miscarriages.
Who Should Get a Sonohysterogram?
An SHG is ideal if you experience irregular bleeding, recurrent miscarriages, or failed IVF attempts. It’s also used to verify that the uterine lining is receptive before embryo transfer.
Timing Tips:
Both tests are best performed after menstruation but before ovulation (typically cycle days 6–10).
This timing reduces infection risk and ensures accurate imaging.
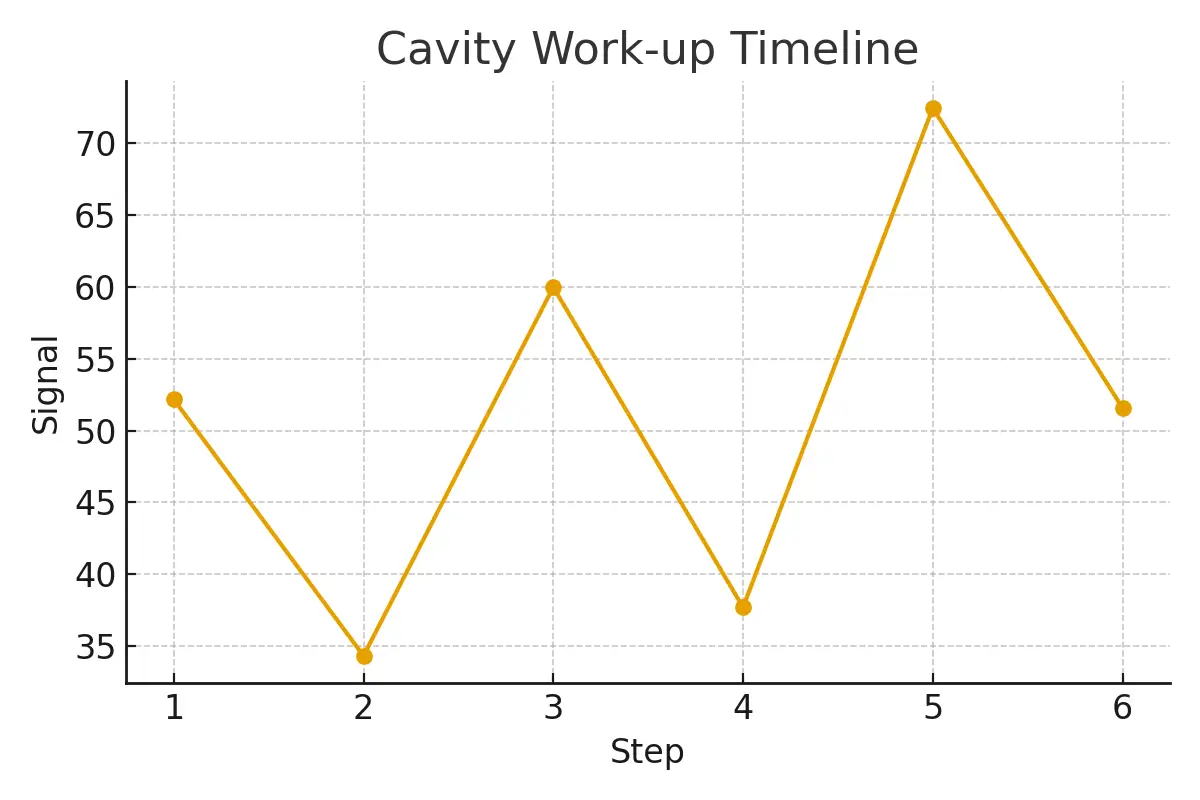
Step-by-Step: What to Expect
HSG Procedure
- Scheduled in a radiology suite.
- A small catheter is inserted into the uterus.
- Dye is injected, and X-ray images are taken.
- The procedure takes about 10–15 minutes.
Mild cramping or spotting may occur afterward. Most patients return to daily activities the same day.
Sonohysterogram Procedure
- Conducted in a fertility clinic using ultrasound.
- Sterile saline is infused into the uterus.
- Ultrasound images are captured in real time.
- Completed in 15–20 minutes.
Discomfort is minimal, and recovery is immediate
Pros, Cons, and Practical Costs
HSG Advantages:
- Provides tubal patency results instantly.
- May slightly increase fertility chances afterward (the “tubal flushing” effect).
Cons:
- Uses radiation and contrast dye.
- Can be mildly uncomfortable.
Average Cost in NYC: $500–$1,200 (depending on insurance coverage and imaging center).
Sonohysterogram Advantages:
- No radiation exposure.
- Detects uterine abnormalities with high accuracy.
- More comfortable than an HSG.
Cons:
- Does not evaluate fallopian tubes completely.
- May require follow-up imaging for certain findings.
Average Cost in NYC: $300–$900, depending on clinic and insurance benefits.
Outcome Drivers: What You Control vs. What You Monitor
You Control:
- Timing of the test.
- Selecting a trusted fertility clinic.
- Following pre-procedure instructions.
You Monitor:
- Results interpretation.
- Next diagnostic or treatment steps (like IVF or IUI).
- Cumulative success rates after testing and optimization.
The key to improving success lies in simplifying your plan — focusing on data, timing, and consistency.
Expert Insight
“Protect timing and keep plans simple—quality improves when noise goes down.”
— Clinical Team, Surrogacy4All
Our fertility experts emphasize that clarity, not complexity, leads to better outcomes. When diagnostic steps are clear, patients experience smoother progress through their fertility journey.
Patient Case Study
A couple in their mid-30s faced inconclusive results after multiple cycles elsewhere. At Surrogacy4All, they underwent an HSG and a Sonohysterogram, revealing a minor uterine adhesion. After a simple outpatient correction and one optimized IVF cycle, they achieved a successful pregnancy.
Aligning logistics, test timing, and expectations made their care predictable — and outcomes more successful.
Testimonials
“The steps finally made sense.” — A.&J., Manhattan
“Costs were clear; no surprise bills.” — L., Hoboken
“Nurses replied fast with practical coaching.” — K.&V., Queens
Additional Insights
- Pharmacy logistics can influence embryo quality and overall IVF success rates.
- Donor screening and transparent pricing help patients plan with confidence.
- Frozen embryo transfer protocols improve outcomes by aligning dose schedules.
- Legal and consent planning ensures emotional and financial stability throughout the patient journey.
- Oocyte retrieval timing impacts implantation success and long-term results.
Next Steps with Surrogacy4All NYC
At Surrogacy4All, we guide you through every step of your fertility journey — from diagnostics to treatment — with personalized care, transparent costs, and data-driven solutions.
Whether you’re preparing for IVF, comparing success rates, or seeking clarity on next steps, our team is here to simplify your path to parenthood.
Book your free 15-minute nurse consult, upload your lab results for a second opinion, or request a custom cost breakdown for your fertility plan today.
Frequently Asked Questions (FAQs)
Q. Is this medical advice?
Ans. No. This content is for educational purposes only. Always consult your fertility specialist before making clinical decisions.
Q. How many IVF cycles should I plan for?
Ans. Success often builds over multiple cycles. Focus on cumulative success rates rather than single-cycle outcomes.
Q. What drives fertility treatment costs in NYC?
Ans. Medication, anesthesia, genetics, and the total number of IVF cycles are key cost factors.
Q. How can I improve IVF success rates?
Ans. Timing, embryo quality, uterine health, and consistent follow-up care greatly influence outcomes.
Q. What makes the fertility patient journey smoother?
Ans. Transparent pricing, clear communication, and realistic planning help reduce stress and improve the overall experience.

Dr. Kulsoom Baloch
Dr. Kulsoom Baloch is a dedicated donor coordinator at Egg Donors, leveraging her extensive background in medicine and public health. She holds an MBBS from Ziauddin University, Pakistan, and an MPH from Hofstra University, New York. With three years of clinical experience at prominent hospitals in Karachi, Pakistan, Dr. Baloch has honed her skills in patient care and medical research.