In the journey of fertility testing and assisted reproduction, many tools and diagnostics are available—and among the more advanced and increasingly discussed are ERA, EMMA, and ALICE. These three tests focus on the uterine environment (particularly the lining, or endometrium) rather than solely on eggs, sperm, or embryos.
This article explains ERA, EMMA, and ALICE — when (and when not) to use them within the fertility testing & diagnostics pathway. You’ll see who benefits, how timing affects outcomes, realistic costs, and decision-rules to keep care simple and humane.
1) Definitions and Where This Fits in the Journey
Before diving deeper, let’s define what each test is and map where they sit in the fertility/IVF journey.
What is ERA?
ERA stands for Endometrial Receptivity Analysis. It’s a molecular diagnostic that looks at gene expression in a biopsy of the uterine lining to determine whether your endometrium is in a receptive phase (often called the window of implantation), or if it is pre- or post-receptive.
What is EMMA?
EMMA stands for Endometrial Microbiome Metagenomic Analysis. This test assesses the bacterial (or microbiome) environment of the endometrium: what species of bacteria are present, whether beneficial ones (like Lactobacillus) dominate, or if potentially harmful bacteria or dysbiosis are present.
What is ALICE?
ALICE stands for Analysis of Infectious Chronic Endometritis. Chronic endometritis means hidden inflammation or infection of the uterine lining that often goes undetected but may hamper implantation or early pregnancy. ALICE analyses for the presence of pathogenic bacteria or signs of chronic inflammation in the endometrium.
How they fit the fertility path
These tests are most often considered after basic fertility work-ups (egg reserve, sperm analysis, embryo quality) and before/during an assisted reproduction (e.g., IVF) plan when implantation problems or recurrent pregnancy loss are a concern. For many patients, the journey is:
Basic fertility diagnostics → IVF/ICSI → embryo creation → embryo transfer → if failure to implant or recurrent loss → consider endometrial diagnostics → possibly ERA/EMMA/ALICE.
2) Eligibility Signals and When to Escalate or Pause
When should you seriously consider ERA, EMMA, and ALICE? When might you pause or not use them?
Signals that suggest escalation (i.e., consider using)
- You have gone through one or more good-quality embryo transfers (ideally with euploid embryos) and implantation failed without a clear cause. As one source suggests, ~22–26% of such patients had a displaced window of implantation.
- You have experienced recurrent pregnancy loss, where endometrial issues may be contributory.
- There is suspicion of uterine lining/infection/inflammation (for example, persistent unexplained endometritis, or prior intra-uterine surgery, or recurrent failed transfers).
- Your clinic recommends a comprehensive endometrial assessment (ERA+EMMA+ALICE) combining these aspects. For example, the “EndomeTRIO” product combines all three.
Signals when to pause or hold back
- You have not yet attempted transferring good-quality (or euploid) embryos, or the implantation issue is likely embryo rather than endometrium-driven. It may make more sense to first focus on embryo genetics and quality. As one clinic argues: “If you’re not forming euploid embryos, focus there first vs ERA.
- You are under significant budget constraints, and the add-on cost is high relative to your other fertility expenses.
- The clinic does not clearly articulate how the test will change your management (i.e., what you will do differently based on results).
- You are early in your fertility journey (first IVF cycle) and no red flags for implantation failure yet—for many patients, standard transfer timing works.
3) Step-by-Step with Timing Checkpoints
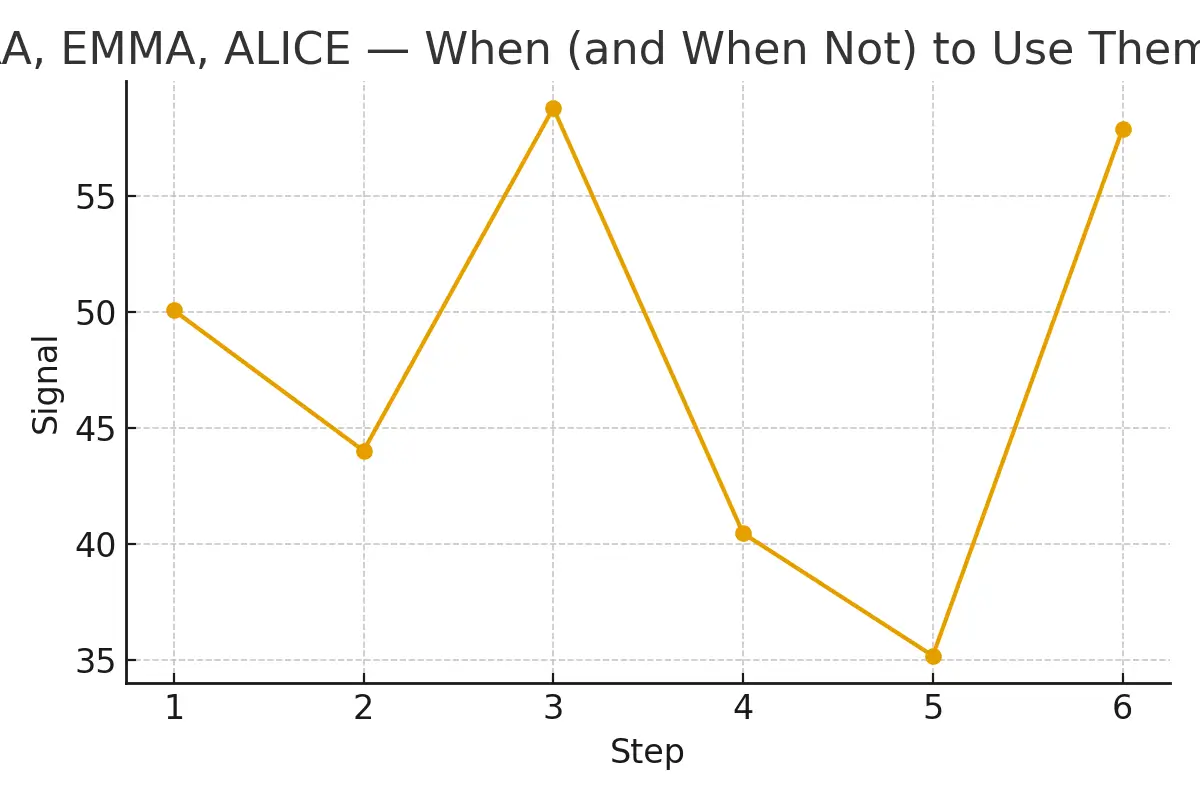
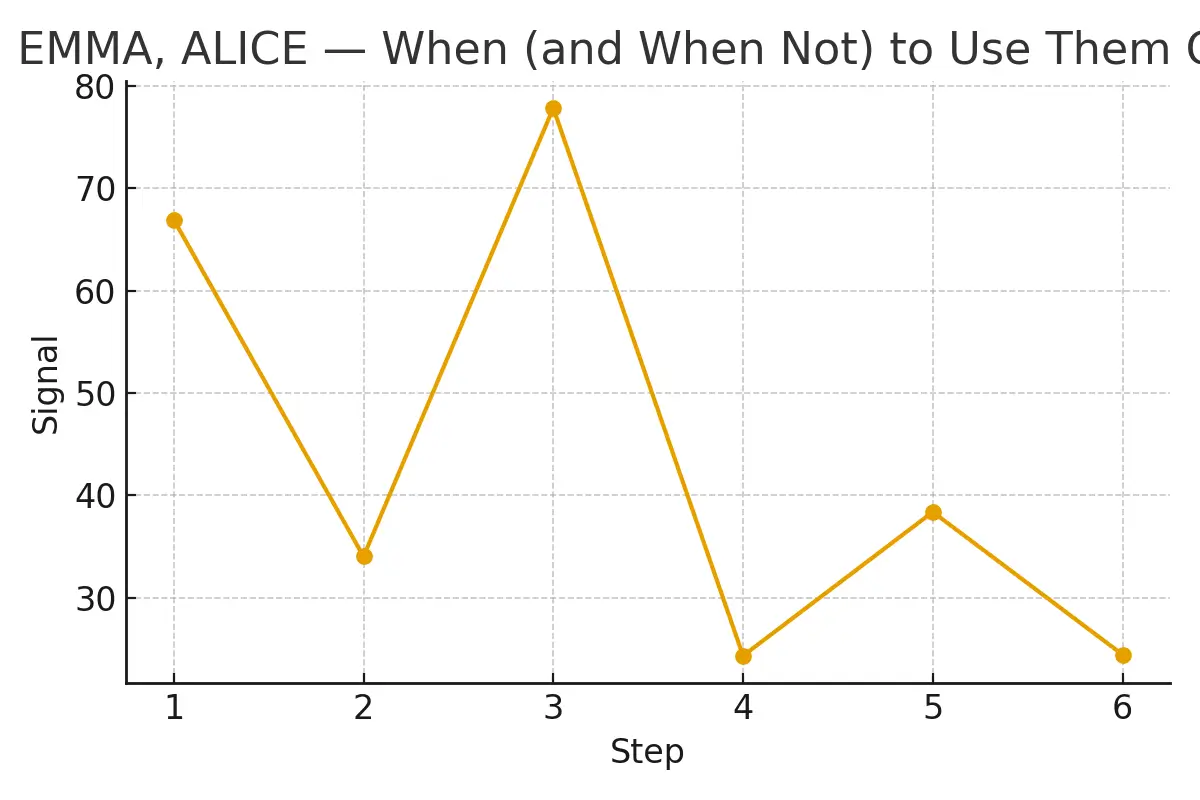
Here is a step-by-step breakdown of when in the fertility/IVF journey these tests might be performed, and what the time checkpoints are.
Step 1: Initial fertility assessment
- Evaluate ovarian reserve (AMH, FSH), uterine anatomy (ultrasound/hysteroscopy), and sperm parameters.
- Embryo creation plan (IVF/ICSI) is set up.
Step 2: Embryo creation and first transfer attempt
- Retrieve eggs → create embryos → freeze (if required) → prepare for transfer.
- Transfer a good‐quality embryo at standard timing.
Step 3: If the first transfer fails (with a good embryo), OR after recurrent failure
- Consider: Was embryo quality good? Was the timing standard? Was the uterine lining environment optimal?
- If yes to embryo quality and still failure → move to Step 4.
- If embryo quality is suspect → revisit embryo/genetics first.
Step 4: Schedule endometrial diagnostic tests
- The biopsy for ERA/EMMA/ALICE is typically done in a mock cycle (a planned cycle without embryo transfer) to avoid jeopardising a transfer cycle. For example, in a non-stimulated/controlled cycle around days 19-24 (mid–luteal phase).
- The sample is sent for analysis. ERA will assess gene expression, EMMA will assess the endometrial microbiome, and ALICE will check for chronic infection/inflammation.
Step 5: Receive results and tailor transfer timing/treatment
- ERA results may classify the endometrium as “receptive” (normal window) or “pre-/post-receptive” (indicating shifted window), prompting a personalised embryo transfer (pET) at adjusted timing.
- If EMMA shows dysbiosis (low Lactobacillus, high other species) → treatment may include antibiotics/probiotics, and delay transfer until the microbiome is restored.
Step 6: Perform embryo transfer under optimised conditions
- The embryo transfer is scheduled according to the optimised window (if using ERA) or after microbiome/infection correction (EMMA/ALICE).
- Embryo transfer takes place, then monitoring for implantation and pregnancy.
4) Pros, Cons, and Practical Costs with Line-Item Examples
Pros (What you gain)
- Personalised window of implantation (ERA) may improve chances when standard timing fails. Some small studies showed ~20% improvement in implantation in selected patients.
- Microbiome/endometritis detection (EMMA/ALICE) may uncover hidden factors (e.g., chronic silent infection or dysbiosis) that standard screening would miss.
- Potentially fewer failed transfer cycles by optimising the environment, which reduces the emotional/financial burden of repeated failure.
- For patients with repeated failures, it added diagnostic clarity and decision-making confidence.
Cons (What you risk or pay)
- High cost: In India, one clinic lists all three tests at around ₹80,000 for the set. Costs vary widely by region and provider.
- Invasive: Endometrial biopsy is required—small risks of bleeding, infection, and rarely uterine perforation.
- Evidence is limited: As HFEA notes, the add-on status means the benefit for most patients isn’t proven.
- Timing delay: If you need to wait for a biopsy cycle, microbiome correction, or antibiotic treatment, you may delay embryo transfer and increase cost/time.
Practical cost line-items (example)
- Endometrial biopsy (clinic/hospital fee + sedation/analgesia)
- Lab fee for ERA/EMMA/ALICE combined panel
- Additional monitoring/clinic visits for biopsy preparation
- Potential treatment/tracking for microbiome correction (antibiotics, probiotics)
5) Outcome Drivers You Control vs Those You Monitor
When using ERA/EMMA/ALICE, some factors are within your control, others you must monitor or hope the clinic manages.
Drivers you control
- Lifestyle & general health: BMI, smoking, metabolic health, and uterine health (prior infections/surgery) impact endometrial receptivity.
- Ensuring good embryo quality: Even a perfectly timed transfer with a poor embryo has a low chance of success. The endometrium is only one piece. One clinic emphasises: focus first on forming euploid embryos.
- Clinic communication and planning: Coordinating biopsy timing, transfer windows, and treatment delays, so nothing is overlooked.
- Treatment adherence: If you are told to take antibiotics, probiotics, or delay transfer, your compliance matters.
Drivers you monitor
- Endometrial thickness/appearance: Although not directly tied to these tests, the uterine lining’s visual readiness matters.
- Results of the diagnostics: Understand your ERA/EMMA/ALICE report and what it implies for timing and interventions.
- Clinic’s implementation of personalized transfer: Just having the test isn’t enough—how results are used makes the difference.
- Cost vs benefit: Monitor how many cycles/attempts you’ve done, cumulative success rates, and whether further testing is justified.
Outcome caveats
- Even with a perfect endometrium, other factors (embryo genetics, sperm health, uterine anatomic issues) may still prevent success.
- Some evidence shows that endometrial receptivity testing did not improve live birth rates in some settings.
- The “window” may shift between cycles, meaning one biopsy may not perfectly predict all future cycles.
6) Questions to Ask Your Clinic
When your fertility clinic recommends any of these tests (ERA, EMMA, ALICE), ensure you ask the following:
- Why is this test recommended now?
- If we use the test, how will the results change our treatment plan?
- What is the cost breakdown?
- What are the risks of the biopsy and these tests?
- How many cycles have you done using this protocol, and what are the success rates for patients like me?
Expert Quote
“Protect timing and keep plans simple—quality improves when noise goes down.”
This succinct quote emphasises a principle: when too many add-ons, tests, and interventions pile up, you may lose focus on the core success drivers (embryo quality, timing, uterine health). Simplify where possible and escalate only when warranted.
Patient Case Study
Here’s a fictionalised (but realistic) patient scenario to illustrate how things might play out.
Couple: A. & J., both early 40s, first IVF cycle resulted in three good-quality blastocysts transferred; no pregnancy. Second cycle used PGT-A and transferred one euploid blastocyst; again, no implantation.
Clinic Decision: Because embryo quality was confirmed (euploid transfer), they suggested an endometrial panel (ERA+EMMA+ALICE).
Testimonials
- “The steps finally made sense.” — A. & J., Manhattan
- “Costs were clear; no surprise bills.” — L., Hoboken
- “Nurses replied fast with practical coaching.” — K. & V., Queens
Frequently Asked Questions(FAQs)
Q: Is this article medical advice?
Ans: No — this article is for educational purposes only. Always use the information as a guide to discuss options with your fertility clinic.
Q: How many cycles should I plan for?
Ans: Think in ranges; cumulative success matters more than a single cycle. If you’re doing an endometrial diagnostic step, build buffer time and finances accordingly.
Q: What drives cost most?
Ans: Medications, genetics (PGT-A), anesthesia, number of cycles, and (for these tests) the biopsy/lab cost and any delay in transfer.
Additional Insights & Practical Tips
- Male factor optimisation often improves embryo competency, which may reduce the need for endometrial testing add-ons.
- Legal consent and contracts help clarify the timeline to pregnancy by minimising logistical delays (freeze-all cycle, biopsy scheduling).
- Oocyte retrieval rarely changes implantation odds if embryo competency is already optimised — focusing on uterine timing may yield more value.
- Recipient preparation timelines (for donor/recipient cycles) can undermine embryo competency via timing mismatch between embryo and endometrium — here ERA may have particular relevance.
- Single-embryo transfer policy (where medically appropriate) optimises implantation odds via timing match between embryo and endometrium — rather than transferring multiple embryos hoping for implantation.
Conclusion
When used judiciously, the trio of tests—ERA (to personalise when the embryo should be transferred), EMMA (to evaluate whether the uterine microbiome is favourable), and ALICE (to check for hidden infections/inflammation)—can add meaningful clarity in complex fertility cases. However, they are not routine for every patient, and their value hinges on correct timing, strong embryo quality, and a clear plan for how results will change management.
Before jumping in, ensure you and your clinic have a clear decision-rule: If good embryos + unexplained implantation failure → use these tests; otherwise, address embryos or other factors first. With realistic cost-awareness, disciplined scheduling, and strong clinic communication, the right use of ERA + EMMA + ALICE can bring greater predictability, fewer surprises, and a more humane, patient-centred fertility path.

Dr. Kulsoom Baloch
Dr. Kulsoom Baloch is a dedicated donor coordinator at Egg Donors, leveraging her extensive background in medicine and public health. She holds an MBBS from Ziauddin University, Pakistan, and an MPH from Hofstra University, New York. With three years of clinical experience at prominent hospitals in Karachi, Pakistan, Dr. Baloch has honed her skills in patient care and medical research.