Key Takeaways
- Autoimmune issues increase miscarriage risk only in specific conditions — not all immune markers are harmful.
- The strongest evidence exists for Antiphospholipid Syndrome (APS), which raises miscarriage risk significantly.
- Thyroid antibodies can modestly elevate risk, but most cases lead to healthy pregnancies with proper management.
- ANA, NK cells, and many popular immune tests do not have strong evidence connecting them to miscarriage.
- Treatments like Heparin, Aspirin, Prednisone, and IVIG help only in carefully diagnosed situations.
Miscarriage is emotionally devastating, and when it happens more than once, it’s natural to ask:
“Is my immune system the reason?”
Online fertility spaces are filled with theories that autoimmunity causes miscarriage — but the actual science is far more nuanced. Only a few autoimmune conditions show a clear, measurable impact on miscarriage risk, while many “immune markers” are misunderstood or overinterpreted.
In this article, we break down honest, evidence-based numbers, helping intended parents, fertility patients, and surrogates understand when autoimmunity truly matters — and when it doesn’t.
Understanding Autoimmune Factors in Pregnancy Loss
Autoimmunity occurs when the body mistakenly attacks its own tissues. In pregnancy, this may theoretically affect:
- Implantation
- Placental development
- Blood flow to the embryo
- Early pregnancy signaling
However, only a few autoimmune conditions have strong, reproducible data linking them to miscarriage.
Autoimmune Conditions With Clear, Evidence-Based Miscarriage Risk
1. Antiphospholipid Syndrome (APS) — Strongest evidence
Miscarriage risk:
- Up to 50–70% without treatment
- Drops significantly (<20%) with proper therapy (Heparin + low-dose Aspirin)
Why it matters:
APS promotes clotting in placental vessels, impairing blood flow to the embryo.
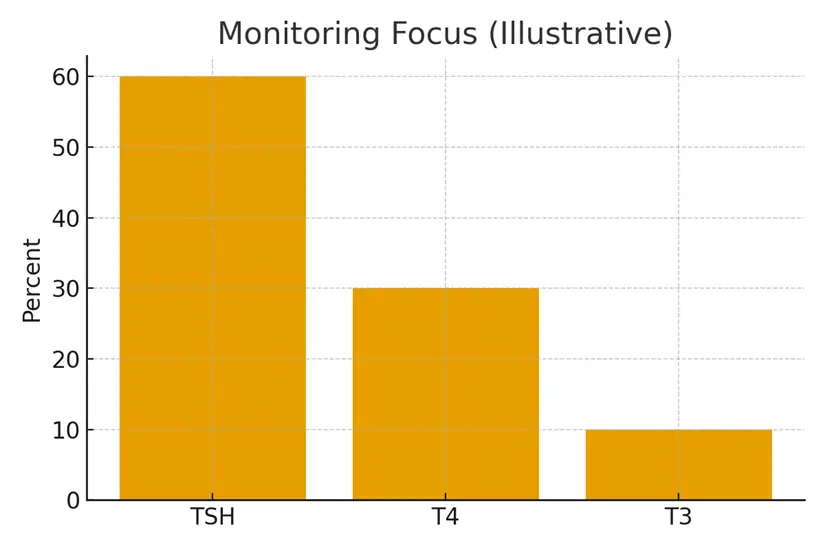
2. Thyroid Autoimmunity (TPO/TG Antibodies)
Miscarriage risk:
- Increases risk by about 2–4×
- Especially when TSH is elevated
Why it matters:
Thyroid dysfunction affects hormonal regulation, placental development, and immune stability.
Treatment impact:
Managing TSH (usually <2.5–3.0 in fertility care) dramatically reduces risk.
3. Type 1 Diabetes & Other Systemic Autoimmune Diseases
Miscarriage risk:
Risk rises only when the disease is poorly controlled.
Conditions include:
- Type 1 diabetes
- Lupus (SLE)
- Rheumatoid arthritis
- Hashimoto’s with uncontrolled TSH
Key point:
Disease activity — not the diagnosis itself — drives risk.
Immune Markers With Weak or No Proven Association
1. ANA (Antinuclear Antibodies)
Frequently positive, especially in women.
No consistent evidence linking isolated ANA positivity to miscarriage.
2. Natural Killer (NK) Cells
Blood NK levels have no proven predictive value for pregnancy loss.
3. HLA Matching, KIR Types
Interesting research areas but currently not recommended for routine miscarriage evaluation.
4. Cytokine Panels
Highly variable, expensive, and not validated for clinical decision-making.
When Immune Treatment Makes Sense
Treatments should be used only when a real diagnosis exists.
| Condition | Treatment Supported by Evidence |
|---|---|
| APS | Heparin + Aspirin |
| Thyroid autoimmunity | TSH control; sometimes low-dose Levothyroxine |
| Lupus w/ antiphospholipid antibodies | Heparin + Aspirin ± immunomodulation |
| Chronic inflammation | Short course steroids (select cases) |
Not supported for routine use: IVIG, Intralipids, LIT, high-dose steroids — unless guided by specialty evaluation.
Case Study: A Realistic Immune-Related Miscarriage Story
Background
A 35-year-old patient experienced three consecutive miscarriages at 6–8 weeks. Standard fertility tests—including PGT-normal embryos—were normal.
Immune Evaluation Revealed:
- Strongly positive antiphospholipid antibodies
- Mildly elevated TPO antibodies
- Normal ANA and NK cell levels
Treatment Plan:
- Low-dose Aspirin starting pre-conception
- Prophylactic Heparin from embryo transfer onward
- Thyroid optimization with Levothyroxine
- Close monitoring during first trimester
Outcome:
The next embryo transfer resulted in a healthy pregnancy carried to term.
Lesson:
The key was diagnosis-driven therapy, not a generic immune protocol.
Testimonials
1. Intended Parent (USA)
“I was overwhelmed by conflicting information online. Seeing the real statistics helped me understand what actually mattered.”
2. IVF Patient (India)
“My doctor initially dismissed my thyroid antibodies. After proper management, my pregnancy was successful. This article reflects my journey perfectly.”
3. Surrogacy Coordinator (Canada)
“We reference data like this to help intended parents understand when immune issues truly affect outcomes.”
Expert Quote
“Autoimmunity can contribute to miscarriage, but only in a subset of cases. Honest numbers prevent unnecessary treatment and ensure we target the real cause.”
— Dr. Kavita Arora, Reproductive Immunology Specialist
Related Links
- Lupus and Pregnancy — Coordination with Rheumatology
- Celiac Disease and Fertility — Screening and Diet
- Prednisone, Heparin, and Aspirin — Where They Fit
- Immunology ‘Add‑Ons’ — Evidence vs Hype
Glossary
APS: Autoimmune clotting disorder linked to miscarriage.
ANA: Autoantibody often present without causing infertility.
Autoimmunity: Immune system mistakenly attacking body tissues.
Cytokines: Proteins involved in immune signaling.
Heparin: Blood thinner preventing clot formation.
IVIG: Immunoglobulin infusion occasionally used in immune disorders.
KIR: Immune receptor gene type (not routinely used clinically).
NK Cells: Immune cells involved in inflammation and defense.
PGT: Genetic testing of embryos before IVF transfer.
TSH: Thyroid-stimulating hormone; critical in pregnancy.
FAQ
Q. Does autoimmunity cause most miscarriages?
Ans. No. Chromosomal abnormalities account for the majority (50–70%) of miscarriages. Autoimmune causes affect a smaller subset, primarily those with APS, thyroid autoimmunity, or uncontrolled systemic autoimmune disease.
Q. How does APS increase miscarriage risk?
Ans. APS causes tiny blood clots in the placenta, disrupting nutrient flow. This leads to early pregnancy loss, fetal growth issues, or complications later in pregnancy. Treatment with Heparin and Aspirin significantly lowers risk.
Q. If my ANA is positive, should I worry about miscarriage?
Ans. Usually not. ANA positivity is common and nonspecific. Most research shows it does not independently increase miscarriage risk unless paired with other autoimmune disease findings.
Q. Do thyroid antibodies cause miscarriage?
Ans. Thyroid antibodies alone don’t directly cause miscarriage, but they are associated with hormonal instability. Managing TSH (ideally <2.5–3.0) greatly reduces risk.
Q. Can NK cells prevent implantation or cause miscarriage?
Ans. There is no consistent evidence linking NK cell levels in blood to miscarriage. NK testing is not recommended by major reproductive societies.
Q. Should every patient with recurrent pregnancy loss get immune testing?
Ans. Not necessarily. Testing is recommended based on medical history and risk factors. Basic testing (APS panel, thyroid panel) is standard. Advanced immune panels should be reserved for specific scenarios.
Q. Can IVIG or Intralipids improve miscarriage outcomes?
Ans. Only in rare cases involving severe immune dysfunction. Evidence for routine use is weak, and these treatments are costly. They should not be first-line therapy.
Q. What treatments are evidence-based for autoimmune miscarriage risk?
Ans. Those are:
- Heparin + Aspirin for APS
- TSH control for thyroid autoimmunity
- Low-dose steroids in specific inflammatory conditions
These have strong track records supported by clinical data.
Q. Does stress cause autoimmune miscarriage?
Ans. Stress does not directly cause miscarriage but may influence inflammation. However, stress alone is not considered a primary miscarriage factor.
Q. Can surrogates be impacted by autoimmune miscarriage risk?
Ans. Yes — but only if the surrogate herself has autoimmune issues. Therefore, thorough medical screening protects both intended parents and carriers.
Q. Should I do immune testing after one miscarriage?
Ans. Usually no. Testing is recommended after:
- 2+ consecutive miscarriages (some guidelines say 3+)
- Recurrent biochemical losses
- Repeated early failed transfers of tested embryos
Q. Can autoimmune miscarriage risk be fully eliminated?
Ans. No risk can be completely eliminated, but evidence-based treatment significantly improves chances of a successful pregnancy. Many patients with autoimmune markers go on to have healthy, full-term pregnancies.

Dr. Kulsoom Baloch
Dr. Kulsoom Baloch is a dedicated donor coordinator at Egg Donors, leveraging her extensive background in medicine and public health. She holds an MBBS from Ziauddin University, Pakistan, and an MPH from Hofstra University, New York. With three years of clinical experience at prominent hospitals in Karachi, Pakistan, Dr. Baloch has honed her skills in patient care and medical research.





