Most miscarriages are not caused by something you did—they’re often due to genetic issues within the embryo. Understanding what to test (and what not to test) can save time, money, and emotional energy. This article focuses on tests and decisions that truly shift outcomes, budgets, and timelines, so you can move forward with clarity and confidence.
What It Is
Miscarriage Genetics — What to Test
- Which genetic evaluations help determine why a pregnancy loss happened.
- Which tests can guide your next steps (IUI, IVF, PGT-A, donor gametes, medical workup).
- How embryo, parent, and sperm factors interact.
- When testing adds value—and when it adds cost without improving results.
- How timing and sample quality can make or break the usefulness of results.
It’s a practical framework for turning painful uncertainty into a clear plan.
Who It Helps
Signals You’re a Good Fit
- Two or more miscarriages (clinical or chemical).
- Miscarriage after IVF or after transferring a “high-grade” embryo.
- Age >35 where aneuploidy risk increases rapidly.
- History of infertility with variable embryo development.
- Previous pregnancy loss with known chromosomal issue (trisomy, monosomy, mosaicism).
- Unexplained implantation failure.
When Another Path May Be Better
- First miscarriage in someone under 35 (often due to random aneuploidy).
- No embryo tissue available for testing and loss appears clearly non-genetic (e.g., uterine anomaly, infection).
- When the result will not change your next step (e.g., you plan IVF regardless).
- If cost constraints mean prioritizing treatment over diagnostics.
Step-by-Step — A Simple, Low-Stress Sequence
1. Test the Pregnancy Tissue (If Available)
- Products of conception (POC) testing via chromosomal microarray is the single most informative test.
- Clarifies whether loss was due to random aneuploidy (most common) or a structural issue.
- Avoids unnecessary parental testing if cause is already explained.
2. Review Parental Chromosomes (If Indicated)
If the POC shows a balanced/structural translocation—or if pregnancy tissue wasn’t available—
→ Parental karyotyping may identify a balanced rearrangement.
3. Screen for High-Impact, Actionable Factors
- Sperm DNA fragmentation (especially for unexplained repeat loss or blastocyst arrest).
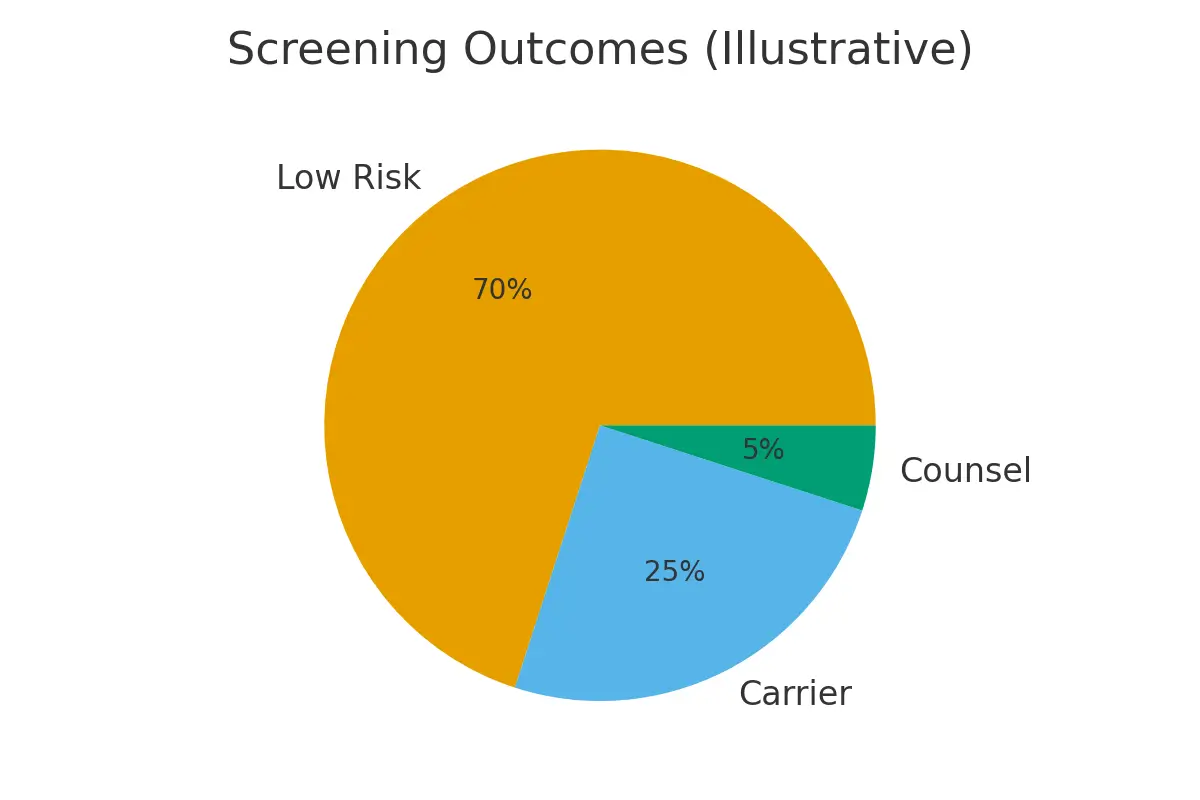
- Expanded carrier screening (ECS) if recessive risk is unknown.
4. Evaluate Embryo Strategy
If losses are due to aneuploidy → consider:
- IVF with PGT-A
- Embryo banking
- Donor eggs for age-related decline
5. Set Decision Checkpoints
Examples:
- “If ≤20% embryos reach blastocyst, adjust protocol.”
- “If POC confirms aneuploidy twice → shift strategy to IVF + PGT-A.”
Pros & Cons
Pros
- Provides a clear explanation for loss in many cases.
- Helps avoid unnecessary treatments.
- Guides whether PGT-A, IVF, or donor gametes meaningfully change odds.
- Reduces recurrence risk if a structural issue is identified.
- Allows personalized planning instead of trial-and-error.
Cons
- POC sample may be unavailable or contaminated.
- Karyotyping may detect variants with unclear significance.
- Some findings don’t change the treatment plan.
- Emotional difficulty in revisiting the loss.
- Added cost if insurance doesn’t cover diagnostics.
Costs & Logistics
Typical Line Items
- POC testing (microarray)
- Parental karyotyping
- Sperm DNA fragmentation testing
- Expanded carrier screening (if not already done)
- Preconception consult with a genetic counselor
- Potential follow-up tests based on findings
Insurance & Authorization
- Many plans cover recurrent pregnancy loss evaluation, including POC testing.
- Karyotyping often needs prior authorization.
- ECS and sperm testing vary widely by insurer and lab.
Simple Cash-Flow Tips
- Prioritize tests that change actions, not those that only provide information.
- Request quotes before POC collection.
- Use a tracking sheet to avoid surprise bills: ordered → billed → insurance → paid.
What Improves Outcomes
Actions That Materially Shift Results
- Testing POC from the next miscarriage to get clear direction.
- Addressing sperm DNA fragmentation (varicocele repair, lifestyle, antioxidants, testicular sperm).
- Choosing IVF+PGT-A when losses are due to recurrent aneuploidy.
- Optimizing stimulation protocols to reduce poor-quality oocytes.
- Treating uterine abnormalities identified on imaging (septum, adhesions, fibroids).
Actions That Rarely Change Outcomes
- Repeating the same basic labs multiple times.
- Testing for extremely rare conditions without clinical indicators.
- Supplements without supporting evidence.
- PGT-A in patients with already high euploid odds (<32 with good AMH).
- Starting treatments without understanding whether the loss was random or recurrent.
Case Study — From Uncertain Losses to a Clear Path
Situation:
A 36-year-old experienced two miscarriages—one natural, one after IUI. No POC testing was done. She worried something was fundamentally wrong.
Approach:
- Third miscarriage tissue was tested: trisomy 16 (a common, random aneuploidy).
- This ruled out structural parental issues and shifted the focus to embryo aneuploidy risk.
- Sperm DNA fragmentation was slightly elevated, offering another target for intervention.
- She opted for IVF with PGT-A to reduce aneuploid transfers and recurring losses.
Outcome:
One IVF cycle produced 4 blastocysts → 1 euploid embryo.
A single transfer led to a successful pregnancy, ending two years of uncertainty.
Mistakes to Avoid
- Not testing POC when it’s available.
- Assuming every miscarriage has the same cause.
- Ordering parental karyotyping before POC testing.
- Overlooking sperm DNA fragmentation.
- Jumping to IVF without understanding whether the issue is random or recurrent.
- Using PGT-A when embryo count is too low for meaningful selection.
- Not setting clear decision checkpoints between cycles.
FAQs
Q: Should I test after the first miscarriage?
Ans : Usually no—most first losses are due to random aneuploidy. Exceptions: age >37, IVF embryos, or prior infertility.
Q: Is POC testing reliable?
Ans : Yes—microarray testing is the gold standard. The main limitation is sample quality.
Q: Do I need parental karyotyping?
Ans : Only if POC shows a structural rearrangement or if no POC is available after repeated losses.
Q: Can sperm cause miscarriage?
Ans : Yes—higher DNA fragmentation is associated with early loss and poor embryo development.
Q: Will PGT-A prevent miscarriage?
Ans : It reduces the chance of transferring aneuploid embryos, lowering miscarriage risk, but isn’t a guarantee.
Next Steps
- Free 15-min nurse consult
- Upload your labs
- Get a personalized cost breakdown for your case
Related Links

Dr. Kulsoom Baloch
Dr. Kulsoom Baloch is a dedicated donor coordinator at Egg Donors, leveraging her extensive background in medicine and public health. She holds an MBBS from Ziauddin University, Pakistan, and an MPH from Hofstra University, New York. With three years of clinical experience at prominent hospitals in Karachi, Pakistan, Dr. Baloch has honed her skills in patient care and medical research.





