Key Takeaways
- In-Vitro Gametogenesis (IVG) is an experimental fertility technology still in research stages.
- IVG aims to create eggs or sperm from stem cells.
- The technology could expand fertility options for infertility, cancer survivors, and same-sex couples.
- IVG is not clinically available yet and faces ethical and regulatory review.
- Gestational surrogacy would likely remain essential even if IVG becomes viable.
The future of fertility medicine is evolving rapidly—often faster than public understanding. Among the most discussed emerging technologies is In-Vitro Gametogenesis (IVG), a scientific approach that could one day allow eggs or sperm to be created from stem cells.
While IVG is not yet available for clinical use, its potential implications for IVF, surrogacy, and family building are profound. This dual guide explores what IVG is, where the science stands today, and what it may mean for intended parents and gestational surrogates in the years ahead.
What Is In-Vitro Gametogenesis (IVG)?
Understanding IVG in Simple Terms
In-Vitro Gametogenesis refers to the laboratory creation of reproductive cells—eggs or sperm—from stem cells, such as skin or blood cells.
In theory, IVG could:
- Generate eggs for individuals born without ovaries
- Create sperm for individuals with non-functional testes
- Expand reproductive possibilities beyond biological limitations
How IVG Differs from IVF
IVF works with existing eggs and sperm.
IVG aims to create gametes first, then use them in IVF-like processes.
| IVF | IVG |
|---|---|
| Uses natural eggs & sperm | Creates eggs/sperm from stem cells |
| Clinically available | Experimental only |
| Regulated worldwide | Under ethical & legal review |
Current Status of IVG Research
Where Science Stands Today
- Successful IVG in animal models (primarily mice)
- Human IVG remains in early laboratory research
- No approved clinical trials for human reproduction yet
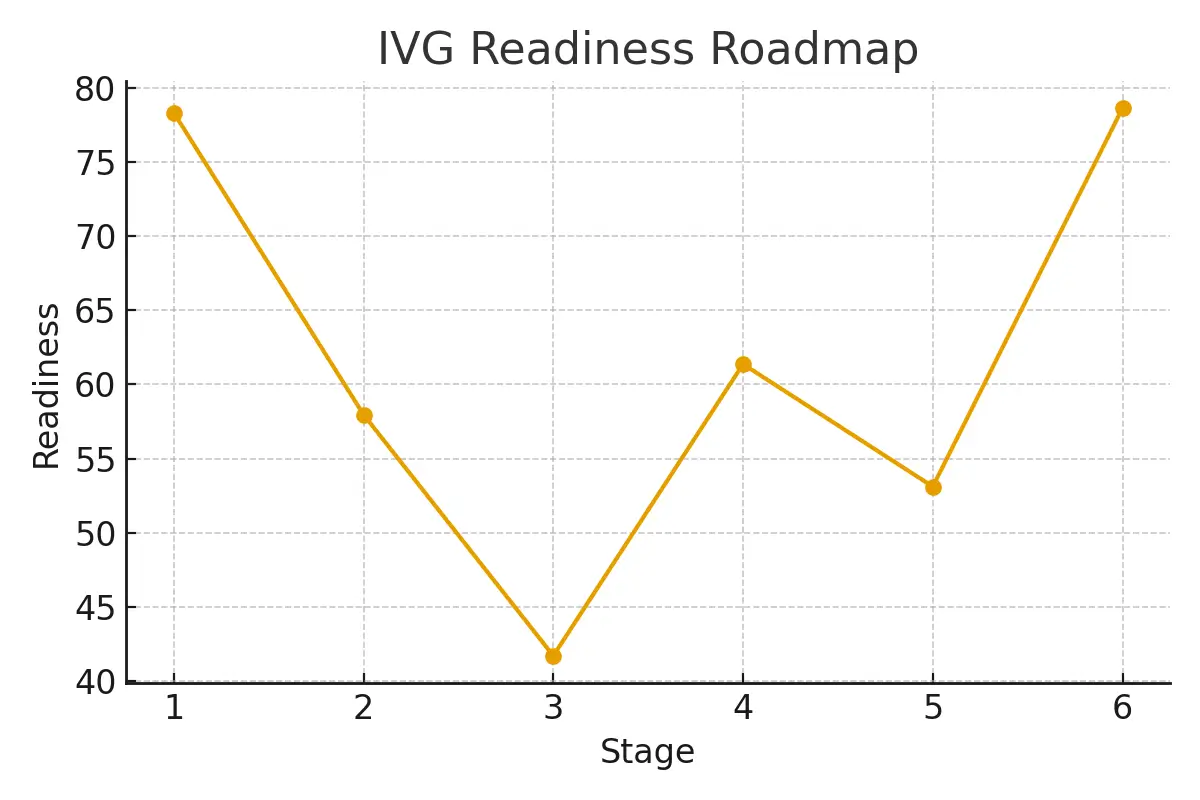
Estimated Timeline
Most experts estimate IVG is 10–20+ years away from possible clinical use, pending safety, ethics, and regulation.
Potential Impact on Intended Parents
Who Could Benefit in the Future?
IVG may one day help:
- Individuals with premature ovarian failure
- Cancer survivors without preserved gametes
- Same-sex couples seeking genetic parenthood
- Individuals with genetic infertility
What IVG Would Not Replace
- Pregnancy itself
- Uterine health
- Gestational surrogacy when carrying is not possible
Even with IVG, surrogacy would remain critical for many families.
What Gestational Surrogates Should Know
Does IVG Change the Surrogate Role?
No—at least not fundamentally.
Surrogates would still:
- Carry the pregnancy
- Undergo medical screening
- Follow established IVF transfer protocols
IVG affects gamete creation, not gestation.
Why Surrogacy Remains Essential
IVG does not eliminate:
- Uterine factor infertility
- Medical conditions preventing pregnancy
- Same-sex male couples’ need for a gestational carrier
Ethical and Regulatory Considerations
Key Ethical Questions
- Genetic safety across generations
- Consent for stem-cell derived gametes
- Risk of genetic manipulation misuse
Why Regulation Matters
Before IVG can be used:
- Long-term safety must be proven
- Ethical frameworks must be established
- International reproductive laws must adapt
Case Study (Hypothetical): IVG’s Future Possibility
Scenario:
A woman born without ovaries wishes to have a genetically related child.
Future IVG Application:
- Skin cells converted into stem cells
- Stem cells differentiated into eggs
- Embryo created via IVF
- Pregnancy carried by a gestational surrogate
Key Note:
This scenario remains theoretical, not clinical reality.
Testimonials (Future-Facing Perspectives)
Intended Parent Perspective
“Knowing technologies like IVG are being researched gives us hope—even if it’s years away.”
Gestational Surrogate Perspective
“No matter how science evolves, pregnancy still requires care, commitment, and support.”
Fertility Researcher Perspective
“IVG holds promise, but safety—not speed—must guide progress.”
Expert Quote
“In-Vitro Gametogenesis represents a scientific frontier, not a finished solution. Its future depends on rigorous research, ethical clarity, and patient safety.”
— Dr. Laura Chen, Reproductive Science Researcher
Related Links
- IVF Treatment Process
- Ethical Issues in Reproductive Medicine
- Gestational Surrogacy Overview
- Fertility Preservation Options
Glossary
- In-Vitro Gametogenesis (IVG): Creation of eggs or sperm from stem cells in a lab.
- Gametes: Reproductive cells (eggs or sperm).
- Stem Cells: Cells capable of developing into specialized cell types.
- IVF: In-Vitro Fertilization using eggs and sperm.
- Uterine Factor Infertility: Inability to carry a pregnancy due to uterine conditions.
Frequently Asked Questions (FAQ)
Q. Is IVG available today?
Ans : No. IVG is still in research and not approved for human reproductive use.
Q. Could IVG replace IVF?
Ans : No. IVG would complement IVF by creating gametes, not replacing fertilization or pregnancy.
Q. Will IVG eliminate the need for surrogates?
Ans : No. Pregnancy and gestation would still require a uterus.
Q. Is IVG safe?
Ans : Safety in humans has not yet been established.
Q. Could same-sex couples use IVG?
Ans : Possibly in the future, but ethical and legal questions remain.
Q. Does IVG allow genetic “designing” of babies?
Ans : No. Ethical frameworks aim to prevent non-medical genetic selection.
Q. How long until IVG becomes available?
Ans : Experts estimate at least 10–20 years, if approved.
Q. Will IVG be regulated internationally?
Ans : Likely, though regulations will vary by country.
Q. Can surrogates carry IVG-created embryos?
Ans : In theory, yes—if IVG becomes clinically approved.
Q. Should intended parents wait for IVG?
Ans : Most experts recommend pursuing proven options available today.
Q. Is IVG related to cloning?
Ans : No. IVG creates gametes, not genetic copies.
Q. Where can I learn about current fertility options?
Ans : Surrogacy.com provides guidance on today’s proven paths to parenthood.

Dr. Kulsoom Baloch
Dr. Kulsoom Baloch is a dedicated donor coordinator at Egg Donors, leveraging her extensive background in medicine and public health. She holds an MBBS from Ziauddin University, Pakistan, and an MPH from Hofstra University, New York. With three years of clinical experience at prominent hospitals in Karachi, Pakistan, Dr. Baloch has honed her skills in patient care and medical research.





