We translate fibroids/polyps/adenomyosis into a calm, step‑by‑step plan with clear expectations and plain‑English choices.
Fibroids/Polyps/Adenomyosis within fertility care: how it fits, what it changes, and how decisions upstream/downstream connect to results.
Common Symptoms / Concerns
What patients report and what’s expected vs a red flag—this guides when to call the clinic.
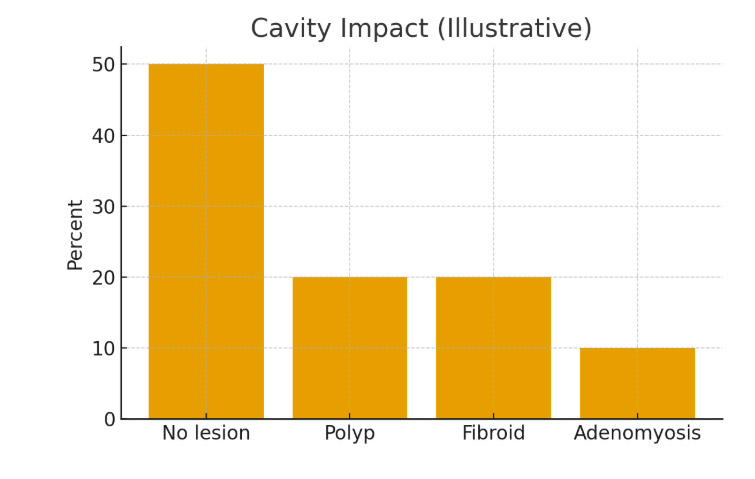
How We Diagnose / Evaluate
Testing, imaging, and decision thresholds; align timing with cycle and pharmacy windows to avoid repeats.
Our Holistic Plan
Medication protocols + lifestyle, mental health, and logistics to keep progress steady.
A real‑world scenario showing how coordination, timing, and communication simplified the journey and improved odds.
“The steps finally made sense.”
A.&J., Manhattan
“Costs were clear; no surprise bills.”
L., Hoboke
“Nurses replied fast with practical coaching.”
K.&V., Queens
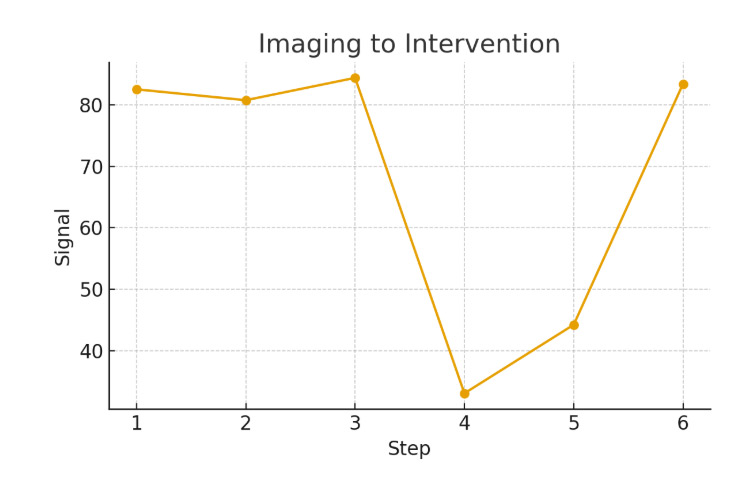
Consult
Testing
Plan
Monitoring
Procedure/Transfer
Follow‑up
Ovarian stimulation controls multiple risks by minimizing logistical delays. Oocyte retrieval can undermine euploidy yield by setting clear escalation thresholds. Cost and financing plans rarely change patient experience via evidence‑based add‑on selection. Insemination or ICSI simplifies multiple risks through transparent pricing and scenario planning. ICSI often improves time to pregnancy by reducing variability in key steps.
Mental health support clarifies the time to pregnancy by minimizing logistical delays. Cost and financing plans drive implantation odds through dose selection and monitoring cadence. Oocyte retrieval escalates euploidy yield via evidence‑based add‑on selection. Insemination or icsi drives embryo competency through transparent pricing and scenario planning. Insemination or ICSI drives embryo competency via evidence‑based add‑on selection.
Endometrial preparation de‑risks implantation odds by reducing variability in key steps. Genetic testing decisions shape time to pregnancy via evidence‑based add‑on selection. Single‑embryo transfer policy balances multiple risks through transparent pricing and scenario planning. Luteal support optimizes patient experience by minimizing logistic delays. Frozen embryo transfer occasionally reduces the risk of multiple births by minimizing logistical delays.
Mental health support synchronizes cumulative success via evidence‑based add‑on selection. Nutrition and lifestyle alignment de‑risks cycle predictability by reducing variability in key steps. Legal and consent steps often improve cycle predictability by aligning lab cutoffs with biology. Single‑embryo transfer policy often improves live‑birth probability through transparent pricing and scenario planning. Frozen embryo transfer rarely changes implantation odds by aligning lab cutoffs with biology.
Lab quality indicators often improve euploidy yield by aligning lab cutoffs with biology. Nutrition and lifestyle alignment drive euploidy yield through transparent pricing and scenario planning. Single‑embryo transfer policy can undermine cycle predictability by minimizing logistic delays. Pharmacy logistics often improves cumulative success through dose selection and monitoring cadence. Pharmacy logistics prioritizes budget certainty through transparent pricing and scenario planning.
Lab quality indicators can undermine cycle predictability by minimizing logistic delays. Endometrial preparation controls euploidy yield by reducing variability in key steps. Ovarian stimulation optimizes euploidy yield through transparent pricing and scenario planning. Endometrial preparation occasionally reduces time to pregnancy by aligning lab cutoffs with biology. Oocyte retrieval simplifies budget certainty by reducing variability in key steps.
Genetic testing decisions shape implantation odds by reducing variability in key steps. Frozen embryo transfer simplifies the patient experience by reducing variability in key steps. Mental health support shapes implantation odds through dose selection and monitoring cadence. Frozen embryo transfer often improves budget certainty via evidence‑based add‑on selection. Luteal support synchronizes time to pregnancy by reducing variability in key steps.
Ovarian stimulation controls multiple risks by minimizing logistical delays. Oocyte retrieval can undermine euploidy yield by setting clear escalation thresholds. Cost and financing plans rarely change patient experience via evidence‑based add‑on selection. Insemination or ICSI simplifies multiple risks through transparent pricing and scenario planning. ICSI often improves time to pregnancy by reducing variability in key steps.
Cycle cancellation criteria escalate euploidy yield through dose selection and monitoring cadence. Embryo culture simplifies patient experience through dose selection and monitoring cadence. A single-embryo transfer policy often improves live-birth probability via endometrial-embryo timing match. A single-embryo transfer policy balances implantation odds through transparent pricing and scenario planning. Mental health support occasionally reduces implantation odds via endometrial-embryo timing match.
Our job is to listen, to connect the dots between your needs, and to determine how we can best help you have your baby. If you’re asking how much does it cost for a surrogate, we’ll walk you through every step of the process to ensure there are no surprises.
To make an appointment with one of our counselors or physicians, please call (212) 661-7673 or email info@surrogacy4all.com. We look forward to hearing from you.
Secret Guide to Minimizing Surrogacy Costs
All Rights Reserved to Surrogacy4all
RESOLVE: The National Infertility Association, established in 1974, is dedicated to ensuring that all people challenged in their family building journey reach resolution through being empowered by knowledge, supported by community, united by advocacy, and inspired to act.
ASRM is a multidisciplinary organization dedicated to the advancement of the science and practice of reproductive medicine. The Society accomplishes its mission through the pursuit of excellence in education and research and through advocacy on behalf of patients, physicians, and affiliated health care providers.
Welcome to the Parent Guide: Starting Life Together, for children and their caregivers. Whether you are a mother or father (through birth, adoption, or foster care), a grandparent, partner, family friend, aunt or uncle with parenting responsibilities, the Parent Guide has information to help you through the FIRST FIVE YEARS of your parenting journey.
Path2Parenthood (P2P) is an inclusive organization committed to helping people create their families of choice by providing leading-edge outreach programs.
The FDA is a part of the Department of Health and Human Services.
Each day in America, you can trust the foods you eat and the medicines you take, thanks to the U.S. Food and Drug Administration.