This article explains donor screening — medical, genetic, and psychological within the Donor Options (Eggs vs Embryos vs Sperm) pathway. We focus on practical choices that shape outcomes, budgets, and timelines—so you can move forward with confidence.
What It Is
Donor Screening — Medical, Genetic, Psychological in plain English: a structured evaluation that ensures donors are healthy, safe, and suitable for creating embryos. Screening affects everything downstream—success rates, risk reduction, legal protections, and the future health of the child.
Medical screening checks for physical health and infectious diseases.
Genetic screening evaluates inherited risks that may affect children.
Psychological screening ensures readiness, informed consent, and emotional stability for all parties involved.
Who It Helps
This pathway is helpful for:
- Families using donor eggs, sperm, or embryos
- Patients with age-related decline, poor response, or genetic conditions
- Couples or individuals seeking lower-risk reproductive options
- Those who want clarity on donor suitability before committing financially
Screening is especially important when history, labs, imaging, or treatment response suggest higher chances of passing on medical or genetic conditions—or when emotional readiness is a key component of a safe donation process.
Step-by-Step
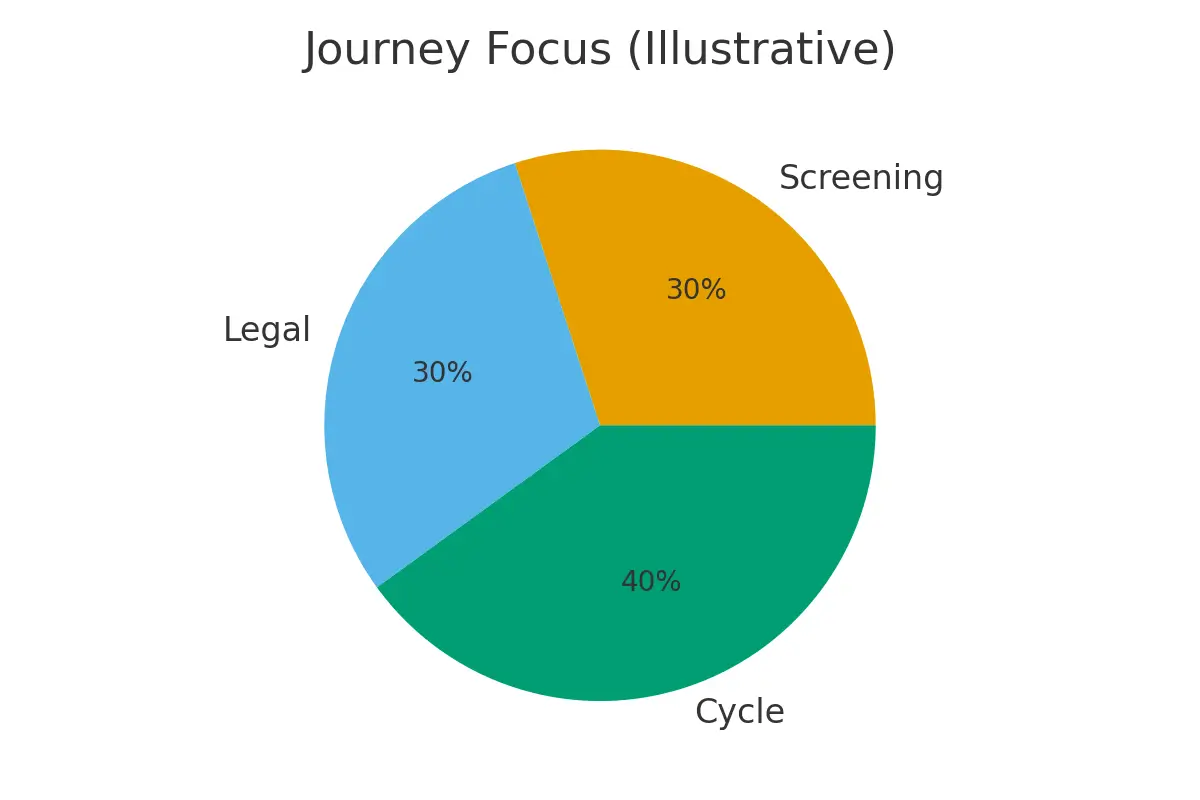
A simple sequence with timing checkpoints to protect embryo quality and reduce stress:
- Initial medical review — donor health history, vitals, lifestyle factors.
- Infectious-disease testing — HIV, hepatitis, syphilis, CMV, and others.
- Genetic carrier screening — common and severe inherited conditions.
- Psychological evaluation — motivation, understanding, stability, boundaries.
- Legal confirmations — rights, responsibilities, documentation.
- Cycle planning — syncing timing for egg donors, sperm donors, or embryo transfer.
- Clear-to-proceed approval — final step before treatment starts.
Each checkpoint ensures donor suitability and minimizes unexpected delays.
Pros & Cons
Pros
- Reduces medical and genetic risks for intended parents and future children
- Improves IVF outcomes by selecting healthy, well-screened donors
- Ensures emotional readiness and responsible participation from donors
- Provides legal protection for all parties
Cons
- Screening adds time before treatment begins
- Some donors may not pass screening, requiring rematching
- Expanded genetic testing can reveal unexpected findings
- Psychological or legal steps may increase upfront costs
Costs & Logistics
Typical line items include:
- Medical evaluation and infectious-disease panels
- Genetic carrier screening (basic or expanded)
- Psychological evaluation fees
- Legal consults and documentation
- Donor agency or bank charges
- Repeat labs for cycle timing
- Administrative costs for clearance and reporting
A simple budgeting system—tracking expected vs actual fees and confirming prior authorizations—helps prevent surprise bills and maintains financial clarity.
What Improves Outcomes
Actions that truly matter:
- Choosing donors with strong medical histories and appropriate age ranges
- Completing genetic screening for both donor and recipient partner
- Ensuring psychological readiness before cycle planning
- Clear communication with coordinators to avoid last-minute testing delays
- Reviewing all results early rather than during the stimulation cycle
Actions that rarely change outcomes:
- Excess layers of non-evidence-based testing
- Repeating labs too frequently without indication
- Choosing donors solely based on photos, ignoring medical data
Case Study
A couple exploring donor eggs felt overwhelmed by medical, genetic, and emotional risks. Their clinic walked them through each screening step with clear thresholds: AMH and BMI limits for donors, mandatory genetic panel coverage, and psychological confirmation before matching. When their first donor failed genetic screening, the structured system prevented expensive cycle delays. Their second donor passed all criteria, and the couple proceeded confidently with a predictable, calm timeline.
Mistakes to Avoid
- Rushing into a donor match without reviewing medical and genetic reports
- Assuming all donor banks screen the same way
- Skipping psychological steps to “save time”
- Not planning legal documents early
- Ignoring partner or recipient genetic compatibility
- Starting stimulation before all results are cleared
FAQs
Q. Why is psychological screening necessary for donors?
Ans. It ensures donors fully understand the process, maintain emotional stability, and participate safely without pressure or unresolved concerns.
Q. How long does donor screening usually take?
Ans. Most donors clear within 2–6 weeks depending on medical testing, genetic panel turnaround, and psychological appointment availability.
Q. What happens if a donor fails genetic screening?
Ans. You’ll be guided to choose a donor with safer genetic compatibility—this prevents avoidable risks for future children.
Q. Are all donors screened the same way across clinics?
Ans. No. Screening standards vary widely. Some clinics perform only minimal testing; others use comprehensive medical, genetic, and psychological evaluations.
Q. Can screening delay the IVF timeline?
Ans. Yes, but in a good way—screening prevents late breakdowns, cycle cancellations, or legal issues that cause much greater delays later.
Next Steps
- Free 15-min nurse consult
- Upload your labs
- Get a personalized cost breakdown for your case
Related Links

Dr. Kulsoom Baloch
Dr. Kulsoom Baloch is a dedicated donor coordinator at Egg Donors, leveraging her extensive background in medicine and public health. She holds an MBBS from Ziauddin University, Pakistan, and an MPH from Hofstra University, New York. With three years of clinical experience at prominent hospitals in Karachi, Pakistan, Dr. Baloch has honed her skills in patient care and medical research.





