Key Takeaways
- “Subclinical” hormone issues often appear normal on lab work but affect cycles, egg quality, implantation, and outcomes.
- Small adjustments—thyroid support, dose tuning, nutrition, sleep, stress control—can convert unstable cycles into consistent, predictable ones.
- Case studies reveal clear patterns: catch early signals, act before symptoms escalate, and integrate lifestyle + medical support.
- Stabilizing hormonal micro-patterns often leads to smoother IVF cycles and fewer unexpected disruptions.
- Personalized monitoring and revisiting plans every 6–8 weeks prevent small problems from turning into major roadblocks.
Most people imagine hormone issues as obvious: irregular cycles, fatigue, weight changes, or poor lab numbers. But many fertility challenges begin long before symptoms become noticeable. These “subclinical” patterns—where numbers are technically normal but functionally suboptimal—can quietly disrupt egg quality, ovulation, and implantation.
This article breaks down real-world case studies showing how identifying and treating subtle signals helped patients become stable, consistent, and cycle-ready. These examples illustrate what shifts outcomes, how to interpret lab patterns, and how to restructure care when early indicators appear.
Understanding “Subclinical” — What It Really Means
- Labs may fall within the “normal range,” but not within the optimal reproductive range.
- Symptoms may be mild or masked, yet biologically meaningful (fatigue, luteal dips, short follicular phases).
- Subclinical issues often show up in:
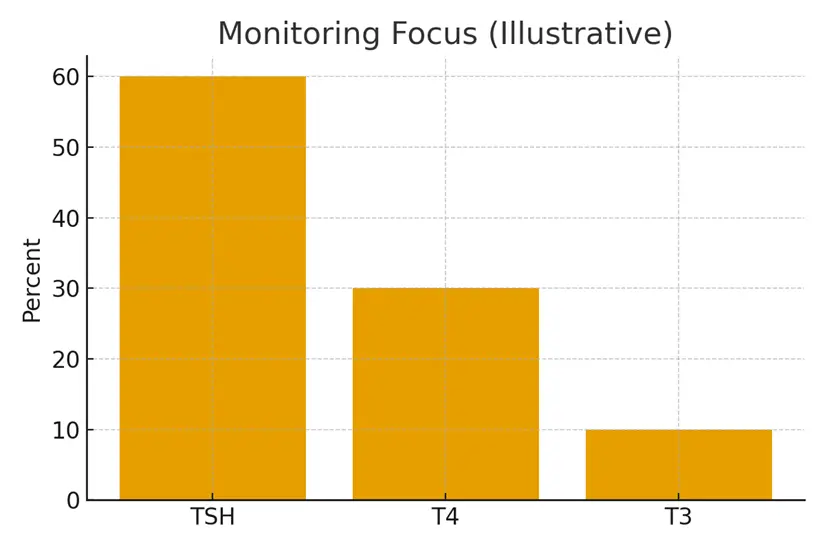
- Thyroid panels
- Prolactin fluctuations
- AMH slowing
- Estradiol spikes
- Cortisol imbalance
- Vitamin D or B12 insufficiency
- Silent inflammation markers
Case Study 1 — Subclinical Thyroid to Stable Ovulation
Profile:
34-year-old woman, 2 unsuccessful IUIs, normal basic labs.
TSH was 3.1 (normal), Free T4 low-normal, mild fatigue.
Intervention:
- Started small-dose levothyroxine
- Added selenium and vitamin D
- Introduced weekly cycle-tracking
Outcome:
- TSH optimized to 1.7
- Ovulation timing stabilized
- Successful IVF retrieval with 2 day-5 embryos
Key Learning:
A small TSH shift from “normal” to “optimal” can correct luteal stability and improve egg development.
Case Study 2 — High-Normal Prolactin & Quiet Implantation Challenges
Profile:
38-year-old, 3 good embryos but repeated implantation failure.
Prolactin high-normal (18–22), no symptoms.
Intervention:
- Micro-dose cabergoline
- Stress-response assessment
- Evening routine optimization to reduce cortisol–prolactin cross-talk
Outcome:
- Prolactin lowered to 10–12
- Lining quality improved
- Successful frozen embryo transfer
Key Learning:
Even high-normal prolactin can block implantation when combined with subtle stress load.
Case Study 3 — “Normal” AMH but Rapid Month-to-Month Variability
Profile:
33-year-old with AMH 2.1, then 1.6, then 2.0 over 4 months.
Cycles increasingly short (23–24 days).
Intervention:
- Anti-inflammatory dietary tweaks
- CoQ10 + omega-3
- Monitoring antral follicle count
- Adjusted FSH dose for retrieval
Outcome:
- Stabilized cycle length
- More predictable follicular growth
- Retrieval yielded double the expected egg count
Key Learning:
Erratic AMH is often an inflammation or lifestyle signal—not diminished reserve.
Three Testimonials
1. Maya, 35
“I had no symptoms, so I assumed everything was fine. Once we corrected tiny thyroid fluctuations, everything—from mood to cycle regularity—became stable. I wish I’d known earlier.”
2. Elena, 39
“My labs were always ‘normal,’ yet cycles felt chaotic. Seeing small patterns explained everything. Stability changed my IVF results completely.”
3. Nisha, 31
“I wasn’t taken seriously because my numbers weren’t ‘bad enough.’ This framework helped me understand that subtle issues can still affect fertility.”
Expert Quote
“Subclinical does not mean insignificant. In fertility, small hormonal shifts often carry big biological consequences. The earlier we intervene, the more predictable the journey becomes.”
— Dr. Rashmi Gulati
Related Links
- Monitoring Plan — Labs and Visit Cadence
- Medication Safety in Pregnancy — Practical Guide
- Supplements — What’s Helpful vs Noise
- Stress and Sleep — The Hormone Connection
Glossary
- Subclinical: A medical state where labs are “normal,” but function is not optimal, often affecting fertility.
- TSH: Thyroid-stimulating hormone, crucial for ovulation and implantation.
- Prolactin: A hormone involved in milk production; high levels can block ovulation/implantation.
- AMH: Anti-Müllerian hormone, an indicator of ovarian reserve.
- Luteal Phase: Post-ovulation phase required for implantation.
- Cycle Variability: Month-to-month changes in length or ovulation timing.
- Cabergoline: A medication that lowers prolactin.
- AFC: Antral follicle count—number of follicles seen during ultrasound.
FAQ
Q. What does “subclinical” mean in fertility?
Ans. Subclinical refers to hormone levels that fall within the standard lab range but are not optimal for reproductive function. For example, a TSH of 3.2 is normal medically but may impair ovulation or implantation. These patterns often require early intervention to prevent larger issues.
Q. Can subclinical issues cause IVF failure?
Ans. Yes. Many failed cycles trace back to subtle, overlooked hormonal inconsistencies—slightly elevated prolactin, low-normal thyroid hormones, unstable estradiol, or cyclical inflammation. When corrected, success rates often improve dramatically.
Q. How can I know if I have a subclinical issue?
Ans. Common clues include cycle irregularity, luteal phase dips, fatigue, sleep disturbance, short follicular phases, or lab values fluctuating month to month. The clearest signal is inconsistency—not necessarily “high” or “low” numbers.
Q. Do I need medication for subclinical problems?
Ans. Not always. Mild issues can often be fixed with lifestyle, supplements, stress and sleep adjustments, and nutrition. But some cases (e.g., TSH or prolactin) respond best to low-dose medication.
Q. How often should I repeat labs?
Ans. Every 6–8 weeks if you’re troubleshooting stability; every 3–6 months if stable. Fertility hormones respond quickly to shifts in stress, sleep, medication, and environment.
Q. Why do doctors miss these patterns?
Ans. Most healthcare systems focus on disease-range diagnostics. Fertility medicine requires optimal-range diagnostics—smaller margins, more frequent monitoring, and sensitivity to subtle biological signals.
Q. Can subclinical thyroid levels affect egg quality?
Ans. Yes. Even mild thyroid dysfunction can disrupt follicle maturation, cycle timing, and progesterone resilience—key factors in egg development.
Q. Does stress cause subclinical instability?
Ans. Chronic stress alters cortisol, which influences prolactin, progesterone, and thyroid conversion. This often shows up as cycle variability or unexpected lab shifts.
Q. Is AMH variability normal?
Ans. Some fluctuation is normal, but large swings often indicate inflammation or metabolic patterns rather than true ovarian decline.
Q. Can I stabilize hormones naturally?
Ans. Yes. Key stabilizers include sleep optimization, stress reduction, anti-inflammatory eating, vitamin D, magnesium, omega-3s, and cycle tracking. Medication is optional but helpful for certain patterns.
Q. Does subclinical instability always need treatment?
Ans. Not always, but monitoring is essential. Mild instability may self-correct once lifestyle or inflammation factors are addressed.
Q. What’s the most important early-action step?
Ans. Identify patterns—not snapshots. Monitor symptoms, cycle length, stress load, and repeat labs every 6–8 weeks until stability is confirmed.

Dr. Kulsoom Baloch
Dr. Kulsoom Baloch is a dedicated donor coordinator at Egg Donors, leveraging her extensive background in medicine and public health. She holds an MBBS from Ziauddin University, Pakistan, and an MPH from Hofstra University, New York. With three years of clinical experience at prominent hospitals in Karachi, Pakistan, Dr. Baloch has honed her skills in patient care and medical research.





