Fertility testing is more than just numbers—it’s about clarity, timing, and trust. When starting an IVF or fertility journey in NYC, two common tests—AMH (Anti-Müllerian Hormone) and FSH (Follicle-Stimulating Hormone)—play a major role in understanding ovarian reserve and treatment potential. Yet, many patients aren’t sure what these tests truly mean or how to use them to make informed choices.
This article breaks down AMH vs FSH—what each test really tells you within the fertility testing and diagnostics pathway. You’ll learn who benefits most, how timing impacts accuracy, the real costs involved, and how to keep your care simple, predictable, and humane.
Understanding AMH and FSH in the Fertility Journey
1. Definitions and Where This Fits in the Journey
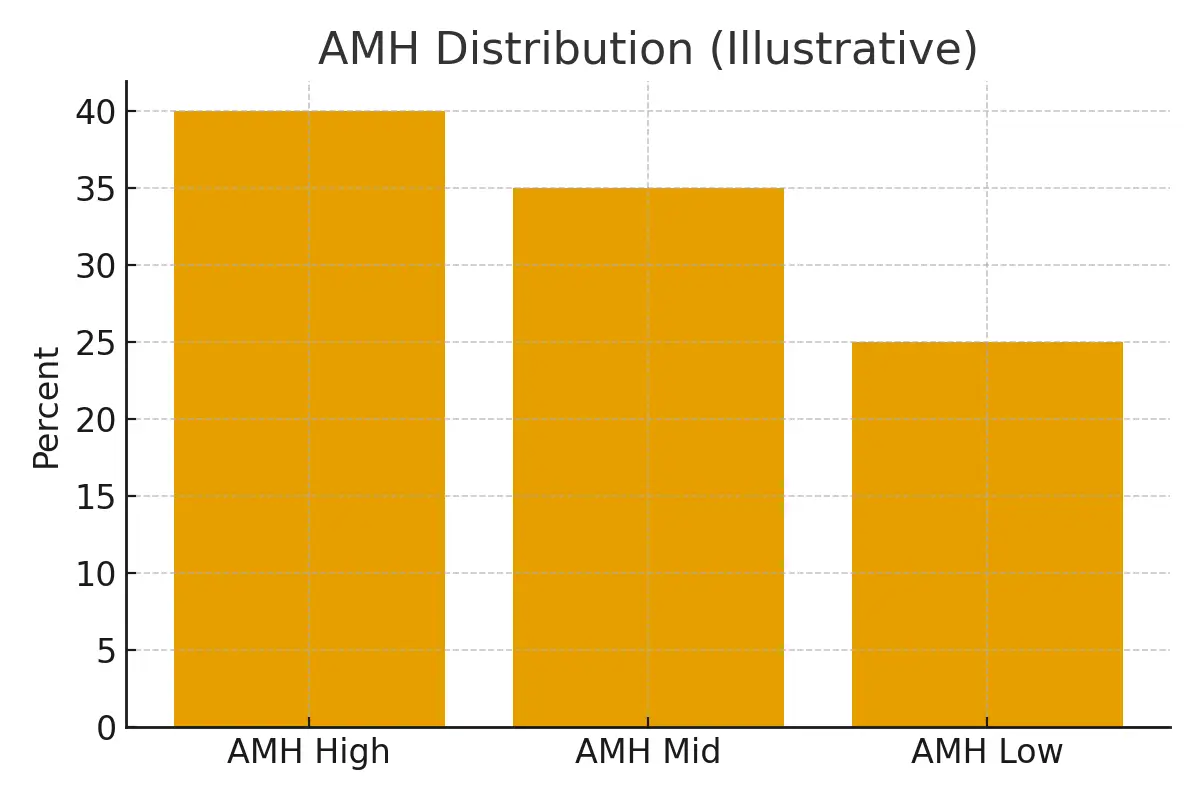
AMH (Anti-Müllerian Hormone) measures the number of eggs (or follicles) a woman has left, giving a clear indicator of ovarian reserve. A higher AMH typically signals a larger egg pool, while a lower AMH suggests diminishing ovarian reserve.
FSH (Follicle-Stimulating Hormone), on the other hand, reflects how hard your body has to work to stimulate egg growth. Elevated FSH levels often indicate that the ovaries are less responsive, requiring more stimulation during IVF cycles.
These two tests together provide a snapshot of reproductive potential—helping clinicians design treatment plans, estimate IVF success rates, and guide patients toward the right timing for intervention.
2. Eligibility Signals and When to Escalate or Pause
Not every patient needs both tests immediately.
Women under 35 may start with AMH alone as part of a baseline fertility evaluation.
Women over 35 or with irregular cycles typically benefit from both AMH and FSH to assess egg quality and ovarian responsiveness.
If AMH is low but FSH remains normal, the window for conception may still be open—but time is of the essence. Conversely, if both AMH and FSH show poor results, your clinic may discuss options like egg freezing, donor eggs, or IVF with advanced stimulation protocols.
Knowing when to escalate or pause testing helps you stay proactive without over-testing or overspending.
3. Step-by-Step Process with Timing Checkpoints
Step 1: Baseline Blood Work
Both AMH and FSH are measured through simple blood tests.
- AMH: Can be taken any day of the menstrual cycle.
- FSH: Should be tested on day 3 of your cycle for the most accurate results.
Step 2: Interpretation
Your fertility specialist will review results alongside other indicators like estradiol (E2) and antral follicle count (AFC). These values help determine if your ovaries are aging faster than expected.
Step 3: Treatment Planning
Depending on your hormone levels, you may begin a fertility plan—ranging from natural monitoring to IVF stimulation, egg freezing, or embryo banking.
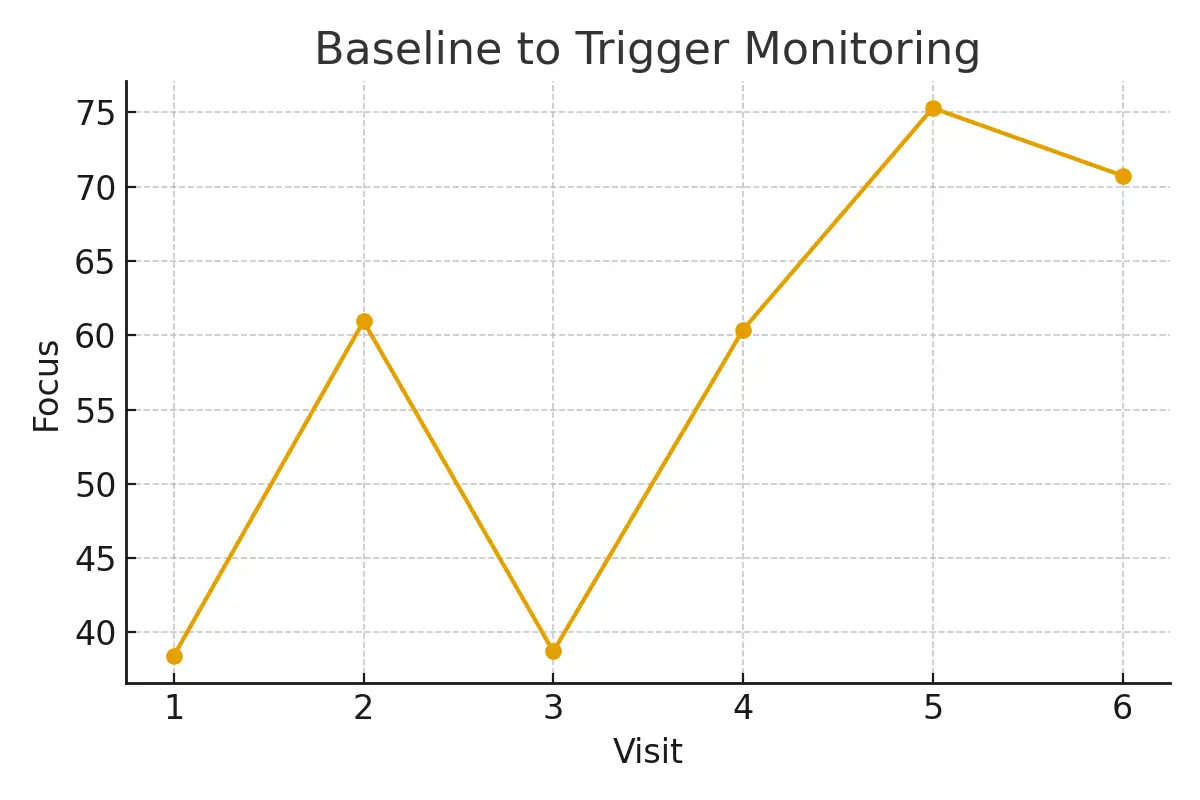
Step 4: Monitoring and Adjustment
If undergoing IVF, hormone levels are re-tested to track ovarian response and adjust medication doses for optimal egg retrieval outcomes.
Timing and consistency are crucial—testing too late or during the wrong phase can distort results and mislead your next steps.
4. Pros, Cons, and Practical Costs
AMH Test
Pros:
- Convenient, no specific cycle day required.
- Predicts ovarian reserve with high accuracy.
- Useful for early fertility planning and IVF success forecasting.
Cons:
Does not measure egg quality—only quantity.
FSH Test
Pros:
- Evaluates ovarian responsiveness directly.
- Helps fine-tune medication doses for IVF cycles.
Cons:
- Must be tested on the correct cycle day.
- Can fluctuate between months, requiring retesting.
Cost Overview
In NYC, AMH testing typically ranges from $100–$200, while FSH costs about $80–$150.
Full fertility diagnostics panels, including ultrasound and hormone mapping, may range from $400–$800 depending on the clinic.
Transparent pricing helps patients plan realistically—avoiding surprise bills and making informed decisions on when to invest in IVF or fertility preservation.
5. Outcome Drivers You Control vs Those You Monitor
What You Can Control:
- Lifestyle: Balanced nutrition, stress reduction, and consistent sleep.
- Timing: Testing at proper cycle days improves diagnostic accuracy.
- Clinic Communication: Stay engaged with your fertility team for clarity and confidence.
What You Monitor:
- AMH & FSH Fluctuations: Track changes every 6–12 months.
- Response to Treatment: Monitor stimulation outcomes and egg quality during IVF.
- Cumulative Success Rates: Remember that overall success builds over multiple cycles.
6. Questions to Ask Your Clinic
- How do AMH and FSH together inform my treatment plan?
- Should I repeat these tests every few months?
- How will my results affect medication dosing for IVF?
- Can I improve my results naturally?
- What are my realistic success rates and cost expectations based on current levels?
Having these questions ready ensures productive, transparent conversations with your care team—helping you understand both numbers and next steps.
Expert Insight
“Protect timing and keep plans simple—quality improves when noise goes down.”
— Clinical Team
Keeping focus on timing and clear communication improves both patient experience and clinical outcomes.
Patient Case Study
A Manhattan couple faced inconclusive test results and growing anxiety. Their clinic synchronized testing with their cycle, simplified communication, and refined medication dosing based on AMH and FSH insights.
By aligning logistics and expectations, they moved from uncertainty to a clear plan—improving predictability and emotional resilience throughout their fertility journey.
Testimonials
- “The steps finally made sense.” — A. & J., Manhattan
- “Costs were clear; no surprise bills.” — L., Hoboken
- “Nurses replied fast with practical coaching.” — K. & V., Queens
Next Steps with Surrogacy4All NYC
At Surrogacy4All, we believe fertility care should be transparent, personalized, and compassionate. Whether you’re comparing AMH vs FSH, preparing for IVF, or exploring your options in NYC, our expert team helps you understand each step—from hormone testing to treatment planning—so you can make confident choices.
Take the next step today:
- Free 15-minute nurse consultation
- Upload your lab reports for a second opinion
- Receive a personalized cost breakdown for your fertility case
Start your journey with Surrogacy4All—where science meets empathy, and every patient journey leads toward hope and clarity.
Frequently Asked Questions (FAQs)
Q. Is this article medical advice?
Ans. No. This guide is for educational purposes only. Always consult your fertility specialist before making medical decisions.
Q. How many IVF cycles should I plan for realistic success rates?
Ans. Think in ranges—most patients achieve success over 2–3 IVF cycles, depending on age and ovarian reserve.
Q. What drives fertility treatment costs the most?
Ans. Key factors include medications, lab quality, anesthesia, and the total number of cycles needed for success.
Q. How can I improve IVF success rates naturally?
Ans. Healthy weight, good sleep, limited alcohol, and stress management can all support better outcomes.
Q. Why is fertility testing so important before starting IVF?
Ans. Testing AMH and FSH early helps set realistic expectations, optimize medication dosing, and improve IVF success rates in NYC.

Dr. Kulsoom Baloch
Dr. Kulsoom Baloch is a dedicated donor coordinator at Egg Donors, leveraging her extensive background in medicine and public health. She holds an MBBS from Ziauddin University, Pakistan, and an MPH from Hofstra University, New York. With three years of clinical experience at prominent hospitals in Karachi, Pakistan, Dr. Baloch has honed her skills in patient care and medical research.