Key Takeaways
- Radiation exposure to the ovaries or testes can significantly reduce future fertility—shielding strategies can sharply lower the risk.
- Even “low-dose scatter radiation” can impact egg or sperm quality depending on treatment field and age.
- Proactive planning—shielding, ovarian transposition, sperm banking, and embryo/egg freezing—should be completed before radiation begins.
- Oncology and fertility teams must coordinate calendars, dose maps, and clearances early to avoid treatment delays.
- Children and adolescents require special protocols, especially with abdominal, pelvic, or total-body irradiation.
When radiation therapy becomes part of cancer treatment, fertility preservation quickly shifts into an urgent, time-sensitive decision. Many patients are told radiation “may affect future fertility,” but few receive specific, actionable guidance. The reality is that dose, location, scatter patterns, shielding techniques, and gonadal sensitivity all determine long-term reproductive impact.
This article breaks down the practical, real-world issues patients face—what shielding can realistically do, when moving ovaries or testes is necessary, and how to make informed fertility decisions without slowing down essential cancer care.
Radiation and Shielding — Practical Issues
How Radiation Impacts Reproductive Organs
Radiation damages rapidly dividing cells—which unfortunately includes:
- Ovarian follicles (eggs)
- Spermatogenic cells
- Uterine tissue and blood vessels
- Endocrine function (ovarian/testicular hormones)
Even doses below the treatment target can reach reproductive organs through scatter radiation.
Approximate thresholds to understand
- Ovarian reserve declines at ~2 Gy
- Permanent ovarian insufficiency likely ≥ 6–10 Gy depending on age
- Testicular function impaired at ~1–2 Gy
- Sperm production can be severely reduced ≥ 4 Gy
These numbers vary by age, health, and treatment field—hence the importance of personalized shielding.
Shielding Options: What Works and When
1. Lead Shielding
Used when radiation fields are near—but not aimed at—the pelvis.
- Reduces scatter dose
- Effective only when radiation fields allow placement
- Does not protect against internal scatter
2. Multi-Leaf Collimators (MLC)
A built-in machine feature that shapes radiation beams.
- Helps “steer” radiation away from gonads
- More effective with advanced radiation modalities (IMRT, VMAT)
3. Ovarian Transposition (Oophoropexy)
A minor surgical procedure that moves ovaries out of the radiation field.
Ideal for:
- Pelvic/abdominal radiation
- Young women wanting future fertility
- Patients unable to freeze eggs/embryos in time
4. Testicular Shielding
Especially important for:
- Hodgkin’s lymphoma
- Pelvic nodal radiation
- Lower abdominal fields
5. Bone Marrow Protection Strategies
For children receiving total body irradiation—fertility preservation is essential because shielding is limited.
Timeline: What Must Happen Before Radiation Begins
Step-by-Step Coordination
1. Mapping Radiation Fields
The oncology team provides a dose map showing how radiation will travel.
2. Fertility Team Review
A reproductive endocrinologist evaluates:
- Expected gonadal dose
- Patient age and baseline ovarian reserve
- Feasibility of egg/sperm/embryo banking
- Whether shielding alone is enough
3. Choose Preservation Strategy
Options include:
- Egg freezing
- Embryo freezing
- Ovarian tissue cryopreservation
- Sperm banking
- Ovarian transposition
- Shielding only (least preferred, but sometimes necessary)
4. Oncology Clearance
Radiation cannot begin until the fertility cycle or surgical plan is finalized.
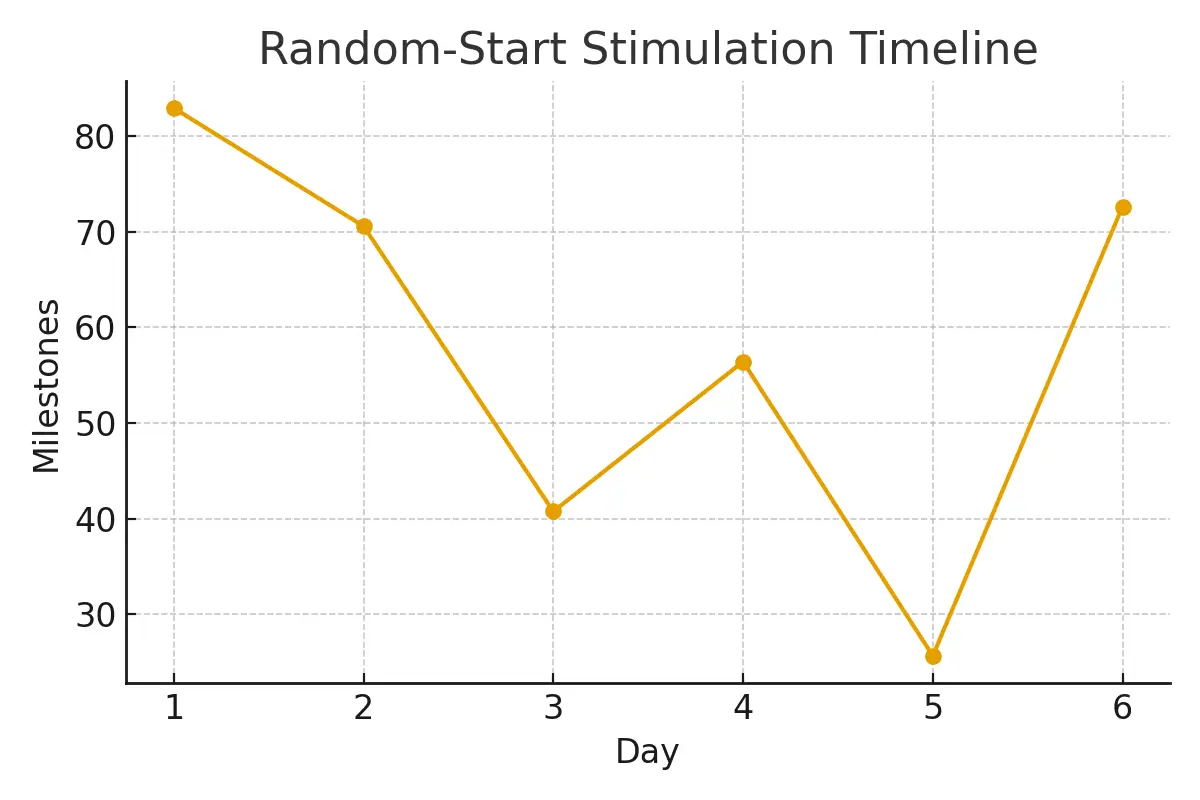
Random-start protocols allow stimulation to begin any day of the menstrual cycle, reducing delays.
Case Study: When Shielding Alone Wasn’t Enough
Patient: 31-year-old woman with rectal cancer
Plan: Pelvic chemoradiation within 18 days
Challenge: Ovaries were within high-dose treatment field
Actions Taken
- Immediate random-start stimulation
- 12 eggs retrieved → 8 mature → 6 embryos frozen
- Ovaries surgically moved above radiation field (ovarian transposition)
- Additional lead shielding placed
Outcome
- Radiation completed on schedule
- Ovarian function returned post-treatment
- Patient used frozen embryos for a successful pregnancy three years later
Testimonials
“My oncologist said the dose was ‘low,’ but the fertility team explained scatter risks. Shielding plus egg freezing gave me peace of mind.” — Anna, 27
“Testicular shielding was simple and fast. I banked sperm the same day. Zero delays.” — Marcus, 33
“They coordinated everything—dose map, clearances, timing. I felt protected and informed.” — Emily, 19 (pediatric sarcoma patient)
Expert Quote
“Radiation safety is not just about protecting organs—it’s about protecting future choices. Shielding, when planned early, can preserve reproductive potential even during aggressive cancer therapy.”
— Dr. Shalini Narang, Reproductive Endocrinologist
Related Links
You can link these to your existing or upcoming surrogacy.com articles:
- Fertility Preservation Pathway Overview
- Egg Freezing vs Embryo Freezing — Decision Framework
- Ovarian Tissue Cryopreservation — When to Consider
- Sperm Banking — Urgent Steps for Men
Glossary
- Gy (Gray): Unit measuring radiation dose
- Scatter Radiation: Radiation that deviates from its path and affects nearby organs
- Ovarian Transposition: Surgery to move ovaries out of treatment field
- IMRT/VMAT: Advanced radiation technologies that shape beams more precisely
- Ovarian Reserve: Number of remaining eggs
- Gonadal Dose: Radiation exposure to ovaries/testes
- Random-Start Stimulation: Starting ovarian stimulation on any cycle day
- Total Body Irradiation (TBI): Radiation to the whole body, often for bone marrow transplant
FAQs
Q. How much radiation is “too much” for the ovaries?
Ans : Even 2 Gy can measurably reduce ovarian reserve. Higher doses (6–10 Gy+) significantly increase risk of permanent infertility, especially for women over 30. Field location, age, and scatter patterns all influence risk. Fertility specialists use radiation plans to calculate predicted gonadal doses and decide whether shielding or ovarian transposition is necessary.
Q. Can shielding fully protect fertility?
Ans : Shielding reduces risk but cannot guarantee protection because internal scatter and micro-dose leakage can still reach gonads. It works best when treatment fields are several centimeters away. For pelvic cancers, shielding must be combined with egg freezing or ovarian transposition.
Q. What if treatment must begin urgently?
Ans : Random-start protocols allow egg retrieval in 10–12 days. Sperm banking can be done same day. If no time is available, ovarian tissue cryopreservation or transposition may be chosen.
Q. Is sperm production more or less sensitive to radiation than eggs?
Ans : Sperm production is highly sensitive—even 1–2 Gy can impair function. However, testicular reserve is more resilient than ovarian follicles, and sperm often recovers unless doses are high. Shielding is extremely effective for men.
Q. Does radiation affect future pregnancy safety?
Ans : Radiation affects eggs or sperm themselves—not the uterus (unless directly targeted). Embryos created before treatment remain safe. For uterus-targeted radiation, pregnancy may be impacted depending on dose and age.
Q. Are children and teens at higher risk?
Ans : Yes. Their gonads contain more actively dividing cells, making them more sensitive. Shielding and fertility preservation planning should begin immediately in pediatric cases.
Q. Should every patient receiving radiation get ovarian or testicular shielding?
Ans : Not always. Shielding is recommended when gonads are within or near the field, or when scatter radiation poses measurable risk. Your radiation team calculates expected doses.
Q. Is ovarian transposition painful or risky?
Ans : It is a minor laparoscopic procedure with low complications and short recovery time. It does not guarantee fertility protection but significantly lowers ovarian dose for many pelvic radiation plans.
Q. How long do frozen eggs, sperm, or embryos last?
Ans : Indefinitely. Cryopreserved gametes remain viable for decades with no increased risk of genetic abnormalities.
Q. Does radiation increase birth-defect risk?
Ans : Radiation to the patient before pregnancy does not increase birth defects in future children. Damage affects fertility potential, not embryo genetics.
Q. Can I still do IVF after pelvic radiation?
Ans : It depends on ovarian function and uterine health. Some patients can still undergo IVF using eggs (if ovarian reserve remains) or embryos. Others may require gestational surrogacy if the uterus is affected.
Q. What happens if I miss the fertility-preservation window?
Ans : Alternative options include donor eggs, donor sperm, donor embryos, or gestational surrogacy. However, many patients can preserve fertility even with very little time—so rapid consultation is essential.

Dr. Kulsoom Baloch
Dr. Kulsoom Baloch is a dedicated donor coordinator at Egg Donors, leveraging her extensive background in medicine and public health. She holds an MBBS from Ziauddin University, Pakistan, and an MPH from Hofstra University, New York. With three years of clinical experience at prominent hospitals in Karachi, Pakistan, Dr. Baloch has honed her skills in patient care and medical research.





