This article explains sperm bank selection — testing, quarantine, CMV, Rh within the Donor Options (Eggs vs Embryos vs Sperm) pathway. We focus on practical choices that shape outcomes, budgets, and timelines—so you can move forward with confidence.
What It Is
Sperm Bank Selection — Testing, Quarantine, CMV, Rh in plain English: how to choose a safe, reliable, and medically appropriate sperm source. It covers key screening requirements, infectious-disease monitoring, genetic testing, quarantine rules, CMV considerations, and Rh compatibility—plus how each decision affects downstream steps like IUI/IVF planning, embryo quality, and cycle timing.
Who It Helps
This guidance supports:
- Individuals or couples using donor sperm for IUI or IVF
- Same-sex female couples and single parents by choice
- Patients needing high-level genetic screening for specific risks
- Anyone unsure how to compare sperm banks and understand medical terminology
It also identifies signals that suggest when to consider alternatives such as known donors or embryo donation.
Step-by-Step
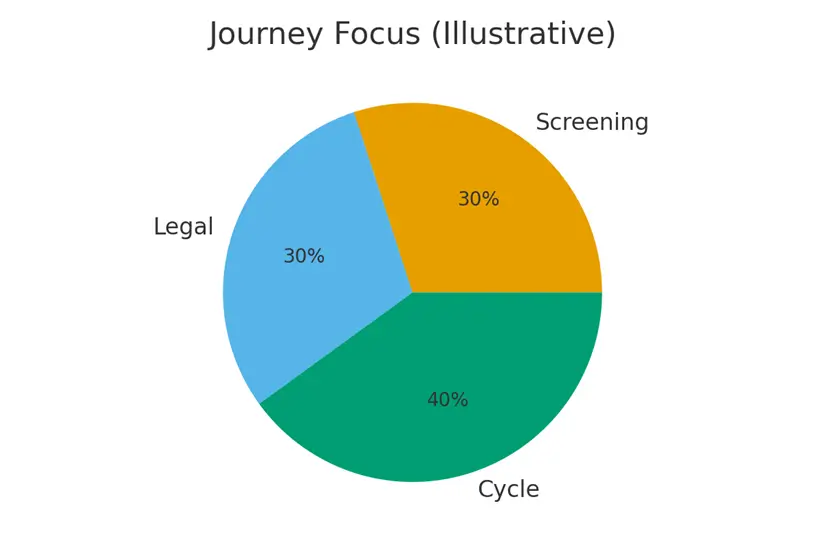
A simple workflow to reduce stress and protect embryo quality:
- Medical review & genetic counseling
- Determine donor type: open-ID vs anonymous
- Review bank’s testing panels (genetic + infectious)
- Check quarantine information (FDA/clinic requirements)
- Review CMV status and Rh compatibility
- Purchase vials + verify clinic storage/shipping rules
- Plan timing for IUI or IVF cycle
- Post-cycle results review and next-step planning
This sequence keeps the process organized, even when coordinating across multiple clinics or banks.
Pros & Cons
Pros
- Highly regulated testing and quarantine requirements
- Predictable availability and clear documentation
- Options for open-ID donors for future contact
- Wide genetic testing panels for donor screening
Cons
- High-demand donors may sell out quickly
- Vial quality and sperm counts vary by bank
- Shipping/storage fees add up
- CMV and Rh compatibility can limit choices
Understanding these trade-offs helps you select the most medically appropriate and financially predictable option.
Costs & Logistics
A transparent overview of:
- Donor vial costs (washed vs unwashed; IUI vs IVF prep)
- Shipping, storage, and clinic receipt fees
- Genetic panel upgrades
- Open-ID surcharges
- Quarantine and compliance fees
We outline how to track expenses, anticipate clinic processing costs, and avoid surprise bills through simple checklists.
What Improves Outcomes
Actions that truly make a difference:
- Choosing banks with consistently high post-thaw motility
- Reviewing donor genetic compatibility with your own carrier screen
- Using washed IUI-ready vials for intrauterine insemination
- Ensuring thaw timing aligns with ovulation or IVF lab schedule
Actions that rarely improve results: selecting based on subjective donor traits alone, over-filtering for unnecessary attributes, or buying excessive numbers of vials early.
Case Study
A single parent by choice is overwhelmed by testing terminology and bank options. Through structured guidance—CMV status, Rh compatibility, genetic matching, vial type, and quarantine rules—they narrow choices to three medically appropriate donors. A clear plan with defined thresholds (post-thaw motility, genetic match, cost limits) helps them confidently select a donor and proceed without delays.
Mistakes to Avoid
Common traps and how to avoid them:
- Ignoring Rh compatibility when the recipient is Rh-negative
- Overlooking CMV status, especially for CMV-negative recipients
- Assuming all banks use identical genetic panels
- Not confirming clinic shipping and storage rules before ordering
- Delaying purchase and losing access to a high-demand donor
Early planning and coordinated communication prevent cycle disruptions.
FAQs
Q. Does CMV status matter for donor sperm?
Ans. Yes. If you are CMV-negative, choosing a CMV-positive donor may increase certain risks, so clinics often recommend CMV-negative donors.
Q. What does sperm quarantine mean?
Ans. Quarantine ensures donors are screened twice for infectious diseases, typically over a six-month window, to meet FDA/clinic safety requirements.
Q. Do I need to match Rh type with my donor?
Ans. If you are Rh-negative, using Rh-negative sperm can reduce the need for additional monitoring, though modern obstetric care usually manages the risk effectively.
Q. What’s the difference between washed and unwashed vials?
Ans. Washed vials are ready for IUI, while unwashed vials are typically used for IVF or lab processing.
Q. Should I buy multiple vials from the same donor?
Ans. Yes if you want future siblings or if the donor is in high demand. Banks may not restock once inventory is gone.
Next Steps
- Free 15-min nurse consult
- Upload your labs
- Get a personalized cost breakdown for your case
Related Links

Dr. Kulsoom Baloch
Dr. Kulsoom Baloch is a dedicated donor coordinator at Egg Donors, leveraging her extensive background in medicine and public health. She holds an MBBS from Ziauddin University, Pakistan, and an MPH from Hofstra University, New York. With three years of clinical experience at prominent hospitals in Karachi, Pakistan, Dr. Baloch has honed her skills in patient care and medical research.





