Key Takeaways
- PCOS and thyroid dysfunction frequently co-exist because both are rooted in metabolic and hormonal regulation.
- Thyroid hormones influence ovulation, insulin sensitivity, and endometrial development — all critical for fertility.
- Even “borderline” thyroid abnormalities (such as mildly elevated TSH) can impact PCOS treatment outcomes.
- Hashimoto’s increases miscarriage risk, especially when untreated.
- Managing insulin resistance is often the first step before adjusting thyroid or reproductive medications.
- A combined PCOS-thyroid strategy improves cycle regularity, egg quality, and treatment predictability.
PCOS and thyroid issues often appear together — not by coincidence but because the same metabolic and hormonal pathways connect them. For many women navigating IVF, egg freezing, or surrogacy-related decision-making, this overlap can feel confusing.
This article breaks down how PCOS and thyroid disorders “cross-talk,” why metabolism is the root link, and what numbers actually matter when planning pregnancy or treatment.
Why PCOS and Thyroid Disorders Commonly Co-Exist
PCOS is fundamentally a metabolic-hormonal condition involving insulin resistance, ovarian dysfunction, and altered androgen levels. Thyroid disorders — especially hypothyroidism and Hashimoto’s — also disrupt energy regulation, inflammation, and hormone balance.
Because both systems regulate metabolism, they often influence each other.
Shared Pathways
- Inflammation: Chronic low-grade inflammation is present in both PCOS and autoimmune thyroid disease.
- Insulin resistance: Hypothyroidism worsens insulin resistance, increasing PCOS symptoms.
- Hormone feedback loops: Thyroid hormones regulate sex hormone binding globulin (SHBG), estrogen metabolism, and ovulatory signals.
How Thyroid Function Influences PCOS Symptoms
Thyroid dysfunction can amplify PCOS symptoms in subtle ways.
Ovulation and Cycle Regularity
Low thyroid hormones → weak ovulatory signals → irregular cycles, worsening PCOS patterns.
Androgen Levels and Acne/Hair Growth
Hypothyroidism reduces SHBG, causing more “free” androgens → acne, hair fall, hirsutism.
Impact on Insulin Sensitivity
Even mild hypothyroidism increases insulin resistance, changing how the body handles glucose — a key trigger in PCOS symptom severity.
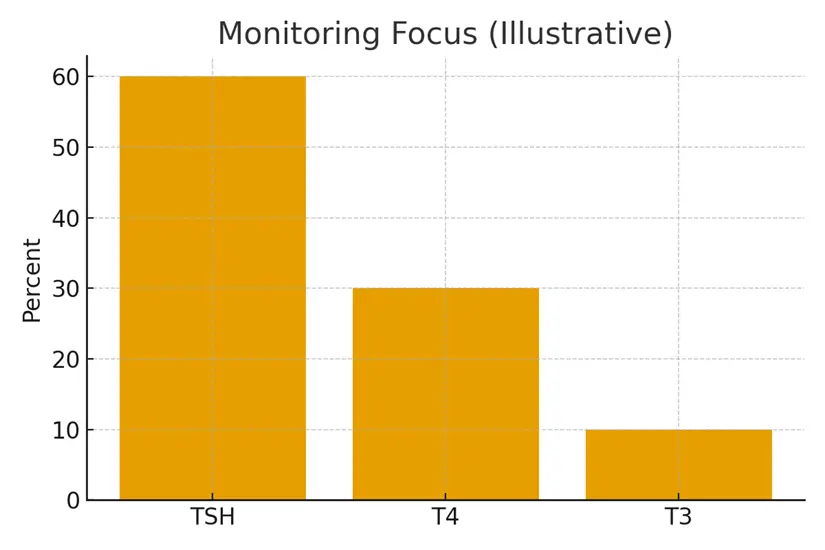
Thyroid Numbers That Matter in Fertility Planning
The “normal” range for thyroid labs is not always optimal for conception.
TSH
- General range: 0.4–4.5
- Fertility-optimal: 1–2.5
Higher levels correlate with ovulation issues and early pregnancy loss.
TPO Antibodies (Hashimoto’s Marker)
Elevated TPO antibodies increase miscarriage risk — even with normal TSH — because of autoimmune-driven inflammation.
Free T4 and Free T3
These determine actual thyroid hormone availability, especially relevant for metabolic function.
The Insulin-Thyroid Connection
This is where the real cross-talk happens.
- Insulin resistance blunts thyroid hormone conversion (T4→T3).
- Thyroid dysfunction increases insulin resistance — a feedback loop.
- Managing glucose stability improves both PCOS symptoms and thyroid function.
First-Line Strategy
Before adjusting thyroid medications, many specialists stabilize insulin resistance through:
- Metformin
- Myo-inositol
- GLP-1 agonists (case-dependent)
- Structured nutrition and resistance training
How This Impacts IVF and Surrogacy Pathways
Thyroid and PCOS interplay affects reproductive treatments.
Egg Quality
Insulin resistance and low thyroid hormones reduce mitochondrial efficiency in developing follicles.
Endometrial Receptivity
Hypothyroidism can thin the lining and delay development.
Miscarriage Risk
Hashimoto’s, uncontrolled TSH, and unstable metabolic markers significantly elevate early pregnancy loss risk.
Case Study: PCOS + Hashimoto’s — A Combined Approach That Worked
Patient: 33-year-old with PCOS, elevated TSH (4.1), and high TPO antibodies.
Challenges: Irregular cycles, failed medicated cycles, poor response in prior IVF attempt.
Approach:
- Started levothyroxine to bring TSH to 1.8
- Added metformin + inositol for insulin resistance
- Implemented anti-inflammatory nutrition and moderate exercise plan
- Repeat IVF four months later
Outcome: Improved egg maturity and fertilization rates; successful embryo transfer leading to ongoing pregnancy.
Testimonials
1. “Fixing my thyroid changed everything.”
“I never realized my borderline TSH was affecting my PCOS. Once corrected, my cycles became predictable again.” — A.R.
2. “Metabolic tuning made IVF smoother.”
“My doctor focused on insulin resistance first. It made my stimulation much more consistent.” — N.K.
3. “Understanding both conditions gave me clarity.”
“PCOS alone felt overwhelming — adding thyroid issues made it worse. This combined approach helped me plan confidently.” — S.M.
Expert Quote
“PCOS and thyroid disorders are not separate problems — they’re different expressions of metabolic imbalance. When we treat them together, fertility outcomes improve dramatically.”
— Dr. R. Mehta, Reproductive Endocrinologist
Related Links
- Celiac Disease and Fertility — Screening and Diet
- Prednisone, Heparin, and Aspirin — Where They Fit
- Immunology ‘Add‑Ons’ — Evidence vs Hype
- Miscarriage Risk and Autoimmunity — Honest Numbers
Glossary
- PCOS: Polycystic Ovary Syndrome — hormonal and metabolic condition affecting ovulation.
- TSH: Thyroid-stimulating hormone — regulates thyroid gland activity.
- TPO Antibodies: Autoimmune markers indicating Hashimoto’s thyroiditis.
- Insulin Resistance: Reduced cell response to insulin, common in PCOS.
- SHBG: Protein that binds hormones; lower levels increase free androgens.
- T4/T3: Thyroid hormones essential for metabolism and energy regulation.
FAQ
Q. Can thyroid issues mimic PCOS symptoms?
Ans. Yes. Hypothyroidism can cause weight gain, irregular cycles, and infertility — which overlap with PCOS symptoms. Distinguishing between the two requires checking TSH, Free T4, and antibodies. Many women are diagnosed with PCOS before discovering an underlying thyroid issue.
Q. Does treating thyroid dysfunction improve PCOS outcomes?
Ans. Often, yes. Correcting TSH levels improves ovulation, boosts SHBG, reduces free androgens, and enhances metabolic stability — all of which reduce PCOS severity.
Q. What TSH level is ideal for conception?
Ans. Most fertility specialists target 1–2.5, even if the general lab range is broader. This reduces miscarriage risk and improves endometrial receptivity.
Q. Do thyroid antibodies affect fertility even if TSH is normal?
Ans. Yes. Elevated TPO antibodies can increase miscarriage risk due to systemic inflammation. Managing inflammation and monitoring thyroid function closely is key.
Q. Why does insulin resistance worsen thyroid symptoms?
Ans. Insulin resistance slows conversion of T4 to active T3. This leaves tissues functionally hypothyroid even when TSH appears normal.
Q. Can improving metabolic health reduce the need for thyroid medication?
Ans. Sometimes. Weight stabilization, reduced inflammation, and improved insulin sensitivity can decrease thyroid stress. But autoimmune thyroid disease usually still requires medication.
Q. How do thyroid issues affect egg quality?
Ans. Low thyroid hormones impair mitochondria — the “engines” of egg cells — leading to immature or poor-quality eggs.
Q. Is Hashimoto’s common in women with PCOS?
Ans. Yes. Autoimmune thyroid disease is significantly more common among women with PCOS due to shared inflammatory and metabolic pathways.
Q. Does metformin help thyroid disorders too?
Ans. Metformin improves insulin sensitivity and lowers inflammation, which benefits thyroid hormone conversion and stabilizes metabolic markers.
Q. Should I check thyroid levels before IVF or egg freezing?
Ans. Absolutely. Thyroid optimization is considered a baseline step before stimulation to ensure predictable response and reduce miscarriage risk.
Q. Can thyroid and PCOS issues impact surrogacy planning?
Ans. Yes — especially during embryo creation. Thyroid/metabolic optimization improves egg quality, fertilization rates, and embryo development.
Q. What if my thyroid levels are “normal” but I still feel symptoms?
Ans. Thyroid numbers don’t tell the full story. Free hormone levels, antibodies, and insulin resistance patterns may explain persistent symptoms.

Dr. Kulsoom Baloch
Dr. Kulsoom Baloch is a dedicated donor coordinator at Egg Donors, leveraging her extensive background in medicine and public health. She holds an MBBS from Ziauddin University, Pakistan, and an MPH from Hofstra University, New York. With three years of clinical experience at prominent hospitals in Karachi, Pakistan, Dr. Baloch has honed her skills in patient care and medical research.





