Key Takeaways
- Age and egg quality — not AMH alone — determine whether own eggs are a viable option.
- Multiple failed IVF cycles with abnormal embryos are strong indicators to consider donor eggs.
- Donor eggs offer the highest predictability, especially for intended parents over 40 or those preparing for surrogacy.
- Emotional readiness is as important as medical fit.
- A decision framework prevents trial-and-error cycles, saving time, cost, and stress.
Deciding between using your own eggs or donor eggs is one of the most significant choices in family building. The decision affects biology, timelines, costs, emotional processing, and long-term expectations.
This guide walks you through a clear, structured framework to understand when own-egg IVF is realistic, when donor eggs offer higher success, and how to evaluate your medical, emotional, and future family goals. Whether you’re planning IVF, comparing clinics, or preparing for gestational surrogacy, this article brings clarity to a decision many people find overwhelming.
Step 1 — Define the Goal Clearly
Before evaluating options, clarify the primary goal:
- Do you want at least one genetically related child?
- Are you planning for one child or multiple children?
- Is there a timeline (age, medical, or surrogacy-related)?
- Is emotional readiness or predictability a priority?
A clear goal prevents emotional conflict and guides the rest of the decisions.
Step 2 — Evaluate Medical Predictors
Age
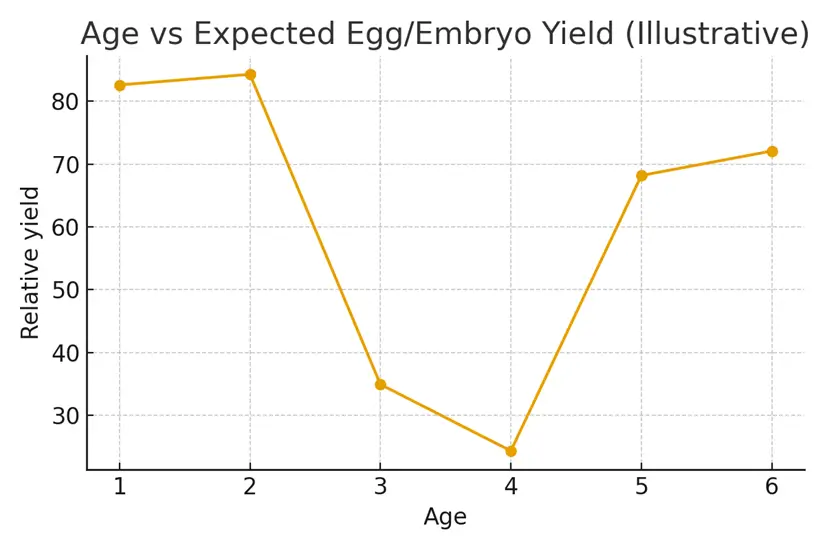
Age is the strongest predictor of success with own eggs.
General probabilities of a chromosomally normal embryo (PGT-A):
- Under 35: 50–60%
- 35–37: 35–45%
- 38–40: 20–30%
- 41–42: 5–15%
- 43+: <5% (donor eggs usually recommended)
Egg Quantity (AMH, AFC)
High AMH/AFC → More eggs → Higher chances
Low AMH/AFC → Few eggs → Multiple cycles needed
Egg Quality Indicators
- Blastocyst formation rate
- PGT-A results
- Past cycle history
- Embryo fragmentation
- Abnormal fertilization patterns
Uterine or Medical Factors
If you cannot carry a pregnancy and are using a surrogate, embryo quality becomes even more critical — making donor eggs more attractive for reliability.
Step 3 — Assess IVF History
Signs own-egg IVF may still work:
- Previous cycles produced at least one good-quality blastocyst
- Some euploid embryos have been identified
- You are under 40 with decent ovarian reserve
- Failed transfers were due to uterine, not embryo issues
Signs donor eggs should be considered:
- Multiple retrievals with zero euploid embryos
- Repeated poor embryo quality
- You’re 41+ and want higher predictability
- Extremely low AMH (under 0.4–0.7)
- Egg quantity and quality mismatch (few eggs + low blast rate)
Step 4 — Compare Predictability vs Genetics
Using Own Eggs
Pros:
- Genetic connection
- Emotional significance
Limitations:
- Uncertain outcomes
- Multiple retrievals may be required
- Lower success at older ages
Using Donor Eggs
Pros:
- Highest success rates across all ages
- Predictable timelines
- High number of embryos
- Better for surrogacy and sibling planning
Considerations:
- Emotional readiness
- Genetic link shifts to donor
Step 5 — Consider Timelines and Costs
Own Eggs
- May require 2–4 retrievals
- Higher medication costs
- More time-consuming
- Less predictable outcomes
- May still lead to donor eggs later
Donor Eggs
- High success → Fewer cycles
- One retrieval from donor usually creates many embryos
- Faster pathway to transfer
- More cost-effective for surrogacy cases
Step 6 — Emotional Readiness
Ask yourself:
- Are you emotionally prepared for donor conception?
- Will multiple failed cycles be harder emotionally than choosing donor eggs now?
- Is predictability more soothing than genetic connection, or vice versa?
Most intended parents need time, and support groups or counseling often help.
Step 7 — Use a Decision Matrix
| Factor | Own Eggs | Donor Eggs |
|---|---|---|
| Genetic Connection | ✔️ | ❌ |
| Success Predictability | Low–Moderate | Very High |
| Embryo Yield | Variable | High |
| Age Impact | Strong | Minimal |
| Surrogacy Suitability | Moderate | Excellent |
| Cost per Live Birth | Higher | Lower |
Case Study: Moving from Own Eggs to Donor Eggs with Clarity
Patient: 41, AMH 0.7
History: Two IVF cycles, both producing poor-quality embryos; no euploid embryos
Goal: One child through gestational surrogacy
Challenge: Patient wanted to try one more cycle with her own eggs. Clinic advised donor eggs early, but patient was emotionally unready.
Decision Framework Used:
- Age-based probability: <10% chance of euploid embryo
- Timeline sensitive due to surrogacy
- Emotional impact of repeated failures
Outcome:
Patient chose donor eggs after reviewing the legal, emotional, and success-rate differences.
The first donor cycle produced:
- 12 blastocysts
- 6 euploid embryos
She now has a successful ongoing surrogate pregnancy.
Her reflection: “If I had seen this framework earlier, I would have saved a year of heartache.”
Testimonials
1. Priya, 40
“I always thought AMH mattered most. Understanding egg quality changed everything. Switching to donor eggs gave us our son.”
2. David & Rina (37 & 43)
“We finally understood why our two IVF cycles kept failing. Donor eggs gave us predictability, and now our surrogate is 22 weeks pregnant.”
3. Jess (38)
“This decision framework helped me see that trying again with my own eggs wasn’t giving me better odds — it was giving me more stress.”
Expert Quote
Dr. A. Menon, Reproductive Endocrinologist:
“The choice between own eggs and donor eggs is rarely about effort — it’s about probability. When age and biology limit outcomes, donor eggs transform the pathway from uncertain to reliably successful.”
Related Links
Glossary
AMH: A hormone indicating ovarian reserve (egg count).
AFC: Antral follicle count seen via ultrasound.
PGT-A: Embryo genetic screening for chromosomal issues.
Euploid Embryo: Chromosomally normal embryo.
Egg Quality: Ability of eggs to form healthy embryos.
Donor Eggs: Eggs provided by another person for IVF.
Own Eggs (Autologous IVF): IVF using the patient’s eggs.
Surrogacy: A gestational carrier carries the pregnancy.
FAQ
Q. How do I know when to stop trying with my own eggs?
Ans. Look at age, repeated IVF outcomes, abnormal PGT-A results, and low-quality embryos across cycles. If multiple cycles produce no euploid embryos, donor eggs may offer a more reliable path.
Q. Are donor eggs more successful than own eggs?
Ans. Yes. Donor eggs have significantly higher success rates because they come from young, medically screened donors with strong egg quality.
Q. Can I still use my own eggs after 40?
Ans. Yes, but success drops sharply. At 40–42, 1–2 euploid embryos may require several retrievals. For many, donor eggs provide better predictability.
Q. What if I’m not emotionally ready for donor eggs?
Ans. This is common. Take time, explore emotions, join support groups, or talk to counselors. There is no “right timeline”; readiness matters.
Q. Do donor eggs guarantee a baby?
Ans. No method guarantees a baby, but donor eggs offer the highest live birth rates in IVF — especially when combined with surrogacy and PGT-A.
Q. Will the baby look like me if we use donor eggs?
Ans. Genetically, the donor provides the DNA. However, the carrier (you or a surrogate) influences gene expression through epigenetic and environmental factors.
Q. Can I combine own eggs and donor eggs?
Ans. Yes. Some parents choose a hybrid approach — banking embryos from both sources to keep future options open.
Q. If I switch to donor eggs, do I still need PGT-A?
Ans. Many clinics recommend PGT-A even with donor eggs because it ensures embryo normalcy and improves transfer reliability, especially for surrogacy.
Q. Are donor eggs more expensive in the long run?
Ans. Although donor eggs have higher initial cost, fewer cycles typically lead to lower overall expenses compared to multiple failed retrievals.
Q. How many donor eggs or embryos will I need?
Ans. Most donor cycles produce 10–20 mature eggs and several blastocysts. You may get 3–6 euploid embryos — enough for one or more children.
Q. How do I choose between anonymous and known donors?
Ans. Consider legal comfort, future identity questions, medical transparency, and your emotional preference. Both options work well.
Q. Is surrogacy easier with donor eggs?
Ans. Yes. Since the surrogate’s uterus is medically screened, embryo quality becomes the main variable — and donor eggs offer high-quality embryos.

Dr. Kulsoom Baloch
Dr. Kulsoom Baloch is a dedicated donor coordinator at Egg Donors, leveraging her extensive background in medicine and public health. She holds an MBBS from Ziauddin University, Pakistan, and an MPH from Hofstra University, New York. With three years of clinical experience at prominent hospitals in Karachi, Pakistan, Dr. Baloch has honed her skills in patient care and medical research.





