Key Takeaways
- Not all fibroids require removal—only those that distort or impact the uterine cavity affect IVF success.
- Hysteroscopic myomectomy is ideal for cavity-distorting (FIGO 0–2) fibroids.
- Laparoscopic and robotic procedures are preferred for larger or deeper (FIGO 3–6) fibroids.
- Adequate healing time matters—typically 1–3 months after hysteroscopy and 3–6 months after laparoscopic/robotic surgery.
- Selecting the right surgical approach can significantly improve implantation and live birth rates.
Uterine fibroids are one of the most common barriers to successful IVF—yet not all fibroids are treated equally. The type, size, and location of a fibroid determine whether it impacts implantation and which surgical approach is most appropriate. Myomectomy options today are far more advanced and minimally invasive, offering shorter recovery and better fertility outcomes.
This guide breaks down the three major myomectomy pathways—hysteroscopic, laparoscopic, and robotic—explaining when each one makes sense, how they work, and what IVF patients need to know before moving ahead.
Understanding Myomectomy Options
Hysteroscopic Myomectomy: Best for Cavity-Distorting Fibroids
Ideal for: FIGO types 0, 1, and some type 2 fibroids
Approach: No abdominal incisions; the surgeon enters through the cervix.
When it matters for IVF:
- Removes fibroids directly interfering with embryo implantation
- Short healing period (typically 4–8 weeks)
- Minimal scarring
Pros:
- Fast recovery
- No external scars
- Highly effective for submucosal fibroids
Cons:
- Not suitable for intramural or large fibroids
- May require staged procedures for deeply embedded fibroids
Laparoscopic Myomectomy: Minimally Invasive Abdominal Approach
Ideal for: FIGO types 3–5, small-to-medium intramural or subserosal fibroids
Approach: Small abdominal incisions with camera-guided instruments.
When it matters for IVF:
- Removes fibroids affecting uterine shape, contractility, or embryo spacing
- Less adhesion formation than open surgery
Pros:
- Faster recovery than open surgery
- Significant symptom relief
- Fertility-preserving
Cons:
- Requires surgical expertise
- May not be suitable for very large or numerous fibroids
Robotic Myomectomy: Precision for Complex Fibroids
Ideal for: FIGO types 3–6, large intramural or difficult-to-reach fibroids
Approach: Robotic arms controlled by the surgeon enhance precision.
When it matters for IVF:
- Offers meticulous dissection with minimal blood loss
- Particularly useful for women with multiple fibroids
Pros:
- Enhanced dexterity
- Excellent visualization
- Good outcomes for complex cases
Cons:
- Higher cost
- Longer operating time in some cases
Case Study
Patient: 36-year-old preparing for IVF
Issue: 4 cm FIGO Type 2 fibroid + 2 intramural fibroids
Plan:
- Hysteroscopic removal of cavity-distorting fibroid
- Laparoscopic removal of intramural fibroids
Outcome:- Uterine cavity normalized within 8 weeks
- Two euploid embryos transferred
- Successful pregnancy on first FET
This hybrid approach optimized implantation potential and minimized surgical trauma.
Testimonials
1. Meera, 34
“My hysteroscopic myomectomy was quick and painless. My lining finally looked normal, and I conceived on my second transfer.”
2. Priya, 39
“My robotic surgery removed six fibroids with minimal recovery time. I wish I had done this earlier—it changed my fertility journey completely.”
3. Ananya, 32
“I avoided unnecessary surgery thanks to proper imaging. Only the cavity-distorting fibroid was removed, and IVF worked soon after.”
Expert Quote
“Choosing the right myomectomy technique is about matching anatomy with fertility goals. When done thoughtfully, surgery can dramatically improve implantation rates while preserving the uterus.”
— Dr. Rashmi Gulati
Related Links
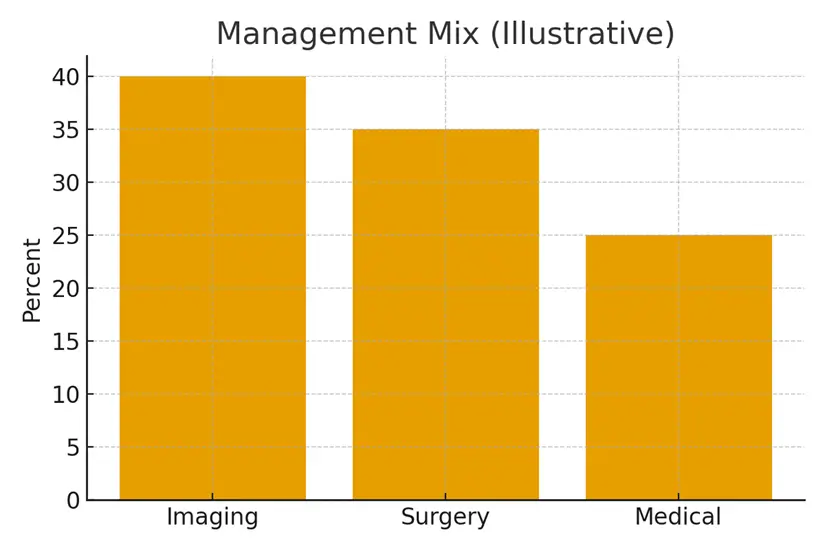
- Imaging Pathway — SIS, HSG, 3D Ultrasound, MRI
- Polyp Removal Before IVF — When to Proceed
- Fibroid Types (FIGO) — Which Ones Matter for IVF
- Cervical Factors — When Access Is the Issue
Glossary
- Myomectomy: Surgical removal of fibroids while preserving the uterus.
- FIGO Classification: A global system categorizing fibroids based on their position in the uterus.
- Hysteroscopy: A procedure using a camera passed through the cervix to view and treat the uterine cavity.
- Laparoscopy: Minimally invasive abdominal surgery using small incisions.
- Robotic Surgery: Laparoscopic surgery performed with robotic-assisted instruments.
- Submucosal Fibroid: Fibroid growing into the uterine cavity.
- Intramural Fibroid: Fibroid located within the muscular wall.
- Subserosal Fibroid: Fibroid growing outward from the uterus.
- Adhesions: Scar tissue that can form after surgery.
- Embryo Implantation: Attachment of the embryo to the uterine lining.
FAQ
Q. Do all fibroids need to be removed before IVF?
Ans. No. Only fibroids that distort the uterine cavity or significantly impact uterine function need removal. Submucosal and certain intramural fibroids (FIGO 0–3) are most likely to interfere with implantation. Subserosal fibroids typically do not affect IVF outcomes and can be left alone unless symptomatic.
Q. How do I know which myomectomy method is right for me?
Ans. Your method depends on fibroid type, size, and location. Cavity-distorting fibroids require hysteroscopic removal, while deeper intramural or large fibroids require laparoscopic or robotic surgery. Detailed imaging—3D ultrasound or MRI—is essential for decision-making.
Q. How long should I wait to resume IVF after myomectomy?
Ans. Healing time varies:
- Hysteroscopic: 4–8 weeks
- Laparoscopic/Robotic: 3–6 months
Your doctor will assess the uterine wall integrity before greenlighting embryo transfer.
Q. Does myomectomy improve IVF success rates?
Ans. Yes—when performed for the correct indications. Removing cavity-distorting fibroids significantly improves implantation and pregnancy rates. Studies show up to a 50% improvement in certain cases.
Q. Is robotic myomectomy worth the cost?
Ans. For complex fibroids or multiple intramural lesions, robotic surgery offers superior precision, less blood loss, and fewer complications. For simple cases, laparoscopy is often equally effective.
Q. Can fibroids come back after myomectomy?
Ans. Yes. Recurrence rates range from 15–30% depending on age, genetics, and the number of fibroids removed. Regular monitoring is recommended, especially before future fertility treatments.
Q. Will surgery weaken my uterus for pregnancy?
Ans. Uterine strength generally returns with proper healing. Deep intramural fibroids may require a longer recovery period. Many women safely carry full-term pregnancies after myomectomy.
Q. Will I need a C-section after fibroid surgery?
Ans. It depends on the depth of the incision. Hysteroscopic procedures do not affect delivery mode. Deeper laparoscopic/robotic incisions may lead your obstetrician to recommend a C-section for safety.
Q. Are there non-surgical options before IVF?
Ans. Medical therapies (GnRH agonists, selective progesterone modulators) may temporarily shrink fibroids but do not replace surgery when cavity distortion is present. UFE (uterine fibroid embolization) is not recommended for women pursuing IVF.
Q. What imaging is needed after myomectomy?
Ans. A follow-up ultrasound—or MRI in complex cases—confirms healing, uterine shape, and absence of residual fibroids before IVF begins.
Q. Can I combine fibroid removal with egg retrieval?
Ans. No. Surgery should always be completed and healed before embryo transfer. However, ovarian stimulation and egg freezing can be done before surgery if medically appropriate.
Q. Does the number of fibroids affect the surgery type?
Ans. Yes. Multiple fibroids, especially >5, often benefit from robotic or laparoscopic removal for better access and precision.

Dr. Kulsoom Baloch
Dr. Kulsoom Baloch is a dedicated donor coordinator at Egg Donors, leveraging her extensive background in medicine and public health. She holds an MBBS from Ziauddin University, Pakistan, and an MPH from Hofstra University, New York. With three years of clinical experience at prominent hospitals in Karachi, Pakistan, Dr. Baloch has honed her skills in patient care and medical research.





