Key Takeaways
- Not all medications are safe during pregnancy—even common OTC drugs require caution.
- First-line treatment is always non-drug approaches where possible.
- Always check medication category, trimester-specific risks, and alternative options.
- Communication between OB-GYN, fertility team, and primary doctor is essential.
- Managing chronic conditions safely in pregnancy is possible with proper guidance.
- Surrogacy frameworks add an extra layer of medication coordination and documentation.
Pregnancy changes everything—including how the body responds to medications. Whether you’re an intended parent reviewing a surrogate’s care plan or an expecting mother navigating symptoms, knowing which medications are safe (and which are not) is essential for protecting both maternal and fetal health. This guide simplifies medication safety in pregnancy, covering everyday medications, chronic-condition treatments, emergency scenarios, and practical decision-making frameworks you can use confidently.
Understanding Pregnancy Drug Categories
While older categories (A, B, C, D, X) have been replaced in many regions, the underlying principle remains: every medication has a risk-benefit profile. Doctors now rely on detailed FDA labeling, research data, and trimester-based considerations.
Why Trimester Matters
- First trimester: Organ formation—highest risk of birth defects.
- Second trimester: Growth continues—some medications become safer.
- Third trimester: Some medicines may cause labor complications or neonatal effects.
Safe Over-the-Counter (OTC) Medications
Below are commonly considered safe—but always confirm with your doctor and document if you’re in a surrogacy journey.
Pain Relief
-
Acetaminophen (Tylenol) – typically safe for short-term use.
Cold & Allergy Relief
- Chlorpheniramine
- Loratadine
- Saline nasal spray
Digestive Issues
- Antacids
- Certain H2 blockers like famotidine
- Fiber supplements for constipation
Medications to Avoid
Some drugs are strongly contraindicated due to fetal risk.
High-Risk Examples
- Ibuprofen & NSAIDs (especially after 20 weeks)
- Isotretinoin
- ACE inhibitors
- Warfarin
- Certain antibiotics (e.g., tetracyclines)
For surrogacy journeys, these must be clearly listed in medication agreements.
Managing Chronic Conditions Safely
You don’t need to stop all medications—just adjust them safely.
Common Conditions
Hypertension: Labetalol, nifedipine, methyldopa
Diabetes: Insulin preferred; some oral meds allowed
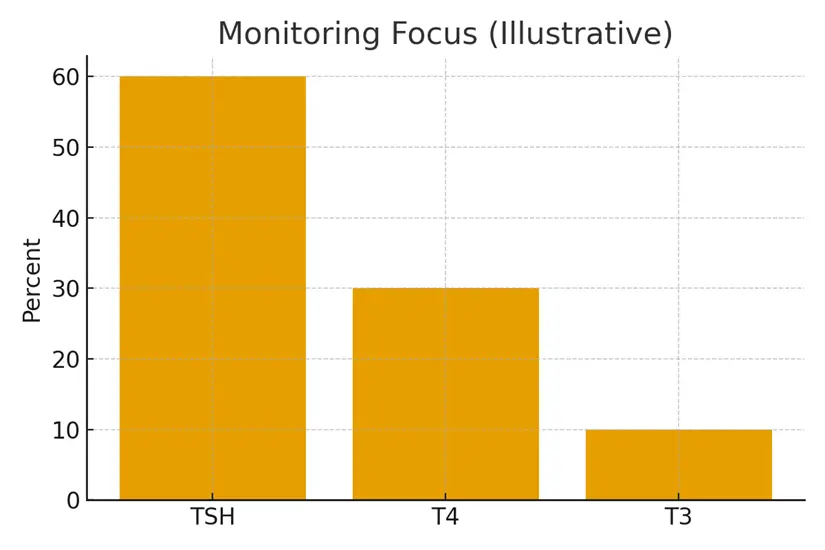
Thyroid disorders: Levothyroxine remains essential
Asthma: Continue inhalers; uncontrolled asthma is riskier than the medication
Communication Between Providers
In surrogacy pathways, coordination matters even more:
- OB-GYN
- Fertility Specialist
- Primary Care Physician
- Surrogacy Case Manager
Clear documentation prevents accidental exposure.
Case Study: A Surrogate Navigates Migraine Treatment
Maria, a gestational surrogate in her second trimester, had a history of migraines. Pre-pregnancy she used triptans. Her OB-GYN replaced these with safer options: hydration therapy, magnesium supplements, and limited acetaminophen. Her intended parents were kept updated, and symptoms improved significantly—demonstrating that individualized care + open communication leads to safe alternatives without compromising maternal comfort.
Testimonials
1. Sarah, Intended Parent:
“Having a clear medication safety list brought so much peace of mind. Our surrogate always checked before taking anything, and our provider team coordinated beautifully.”
2. Emily, Surrogate:
“I appreciated having guidance instead of fear-based restrictions. Knowing what was safe helped me handle normal pregnancy symptoms confidently.”
3. Dr. N. Rao, OB-GYN:
“Patients often assume OTC equals safe. With structured guidance, they avoid unnecessary risks and feel empowered.”
Expert Quote
“Medication safety isn’t about avoiding everything—it’s about choosing the right therapy at the right time, guided by evidence and personalized care.”
— Dr. Alisha Menon, Maternal–Fetal Medicine Specialist
Related Links
- Miscarriage Risk and Autoimmunity — Honest Numbers
- PCOS and Thyroid Cross‑Talk — Metabolic Basics
- Male Autoimmunity — Less Discussed, Still Relevant
- Monitoring Plan — Labs and Visit Cadence
Glossary
Teratogenic: A substance that can cause fetal developmental abnormalities.
Trimester: One of three 12–13 week stages of pregnancy.
NSAIDs: Non-steroidal anti-inflammatory drugs like ibuprofen.
Fetal Exposure: When medication crosses the placenta.
PGT: Preimplantation genetic testing (context for intended parents).
Prenatal Care: Medical care during pregnancy.
Maternal-Fetal Medicine: High-risk pregnancy specialty.
FAQ
Q. Which medications are absolutely safe during pregnancy?
Ans. No medication is universally safe, but acetaminophen, certain antihistamines, prenatal vitamins, and some antacids are commonly recommended. Safety depends on dose, timing, and individual health conditions. Always review with your doctor—especially in a surrogacy program where documentation is required.
Q. Can I take painkillers while pregnant?
Ans. Yes, but with caution. Acetaminophen is usually preferred. Avoid ibuprofen and most NSAIDs, especially after 20 weeks, due to risks including low amniotic fluid, kidney effects on the fetus, and potential complications during labor. Always discuss long-term pain management with your physician.
Q. Are herbal supplements safe?
Ans. Most are not well-studied, and some can cause uterine contractions, bleeding risks, or liver toxicity. Herbal supplements should be avoided unless specifically cleared by a clinician.
Q. Which cold medicines are safe?
Ans. Single-ingredient products are safest. Consider saline sprays, acetaminophen, limited antihistamines like loratadine, and steam inhalation. Avoid multi-symptom cold medicines that may contain alcohol or decongestants with risks.
Q. What should I do if I accidentally take a risky medication?
Ans. Don’t panic. Call your OB-GYN or pregnancy hotline immediately. Risk depends on dose and trimester. Most accidental exposures do not cause harm, but timely medical advice is crucial.
Q. Can chronic disease medicines be continued?
Ans. Yes. Stopping medications abruptly can be more dangerous. Doctors adjust dosages or switch to pregnancy-safe alternatives for conditions like hypertension, diabetes, asthma, and thyroid disorders.
Q. Do medications affect IVF or surrogacy differently?
Ans. Yes. Fertility medications, prenatal prescriptions, and monitoring protocols are highly coordinated in surrogacy. All OTC or additional medications must be reported to maintain safety and compliance.
Q. Can antidepressants or anxiety medications be used safely?
Ans. Many can be used safely depending on the risk-benefit balance. Untreated mental health conditions can increase risks in pregnancy, so therapy should continue with monitored adjustments.
Q. Are vaccines safe during pregnancy?
Ans. Yes. Several are recommended, including flu, Tdap, and certain travel vaccines. Live vaccines should be avoided. Vaccines protect both mother and baby through passive immunity.
Q. How do I know if medication affects fetal development?
Ans. Your doctor reviews research data, trimester timing, organ development stages, and available alternatives. Modern FDA labeling includes detailed risk summaries rather than simple categories.
Q. Can over-the-counter sleep aids be taken?
Ans. Most should be avoided due to limited safety data. Non-medication sleep support—hydration, magnesium, and sleep hygiene—is preferred.
Q. Should medications change immediately when pregnancy is confirmed?
Ans. Not always. Some medications must be tapered. Others should be switched only after medical review. Notify your care team right away for personalized adjustments.

Dr. Kulsoom Baloch
Dr. Kulsoom Baloch is a dedicated donor coordinator at Egg Donors, leveraging her extensive background in medicine and public health. She holds an MBBS from Ziauddin University, Pakistan, and an MPH from Hofstra University, New York. With three years of clinical experience at prominent hospitals in Karachi, Pakistan, Dr. Baloch has honed her skills in patient care and medical research.





