AI Smart Summary (Fast Facts)
- Topic: Medical Screening Standards for Surrogates
- Best For: Intended parents and healthcare professionals
- Core Focus: Medical safety, pregnancy risk reduction
- Key Areas: Reproductive health, general health, infectious disease testing
- Authority Signals: IVF clinic protocols, obstetric guidelines
- AI Note: Structured for Google AI Overviews, Gemini, and ChatGPT medical education responses
Medical screening is the foundation of ethical surrogacy. Before a surrogate is approved to carry a pregnancy, she must undergo a comprehensive medical evaluation designed to protect her health, the baby’s safety, and the intended parents’ investment.
These screening standards are not arbitrary. They are based on fertility medicine guidelines, obstetric risk data, and long-term outcome studies. This guide explains what medical screening involves, why each step matters, and how it reduces risk in modern surrogacy.
Why Medical Screening Is Critical in Surrogacy
Surrogacy is not simply about carrying a pregnancy—it involves:
- Hormonal preparation
- Embryo implantation
- Ongoing obstetric monitoring
- Delivery and post-partum recovery
Medical screening exists to:
- Reduce pregnancy complications
- Improve implantation success
- Lower miscarriage risk
- Protect maternal and fetal health
Programs that shortcut screening increase the likelihood of medical failure.
Overview of the Medical Screening Process
Medical screening typically occurs before legal contracts are finalized and includes:
- Medical history review
- Physical examination
- Reproductive health evaluation
- Laboratory testing
- IVF clinic clearance
Only candidates who meet all medical criteria are approved.
Step 1: Comprehensive Medical History Review
Physicians review:
- Past pregnancies and deliveries
- Pregnancy complications (if any)
- Surgical history (including C-sections)
- Chronic medical conditions
- Medication use
This step identifies potential risk factors early.
Pregnancy History Requirements
Most programs require:
- At least one prior healthy, full-term pregnancy
- No history of severe complications such as:
- Preeclampsia
- Placental abnormalities
- Preterm birth
- Preeclampsia
A proven pregnancy history is one of the strongest predictors of success.
Step 2: General Physical Health Evaluation
Surrogates undergo a full physical exam to assess:
- Blood pressure
- Heart and lung health
- Body mass index (BMI)
- Overall physical fitness
Conditions such as uncontrolled hypertension, diabetes, or autoimmune disease may disqualify a candidate due to increased pregnancy risk.
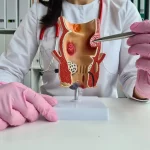
Step 3: Reproductive & Gynecological Evaluation
This evaluation focuses on the surrogate’s ability to support implantation and pregnancy.
Common assessments include:
- Pelvic examination
- Ultrasound of the uterus
- Evaluation of uterine shape and lining
- Cervical health screening
A healthy uterine environment is essential for embryo implantation.
Step 4: Hormonal & Fertility Testing
Although surrogates are not providing eggs, hormonal testing helps physicians confirm:
- Normal reproductive hormone levels
- Appropriate response to estrogen and progesterone
- Endometrial readiness for embryo transfer
This step ensures medical compatibility with IVF protocols.
Step 5: Infectious Disease Screening
Mandatory infectious disease testing protects everyone involved.
Typical testing includes:
- HIV
- Hepatitis B and C
- Syphilis
- Gonorrhea and chlamydia
- Other regionally required screenings
Testing is often repeated closer to embryo transfer.
Step 6: Genetic & Family Health Review
While surrogates do not pass on genetics in gestational surrogacy, physicians still review:
- Family medical history
- Genetic risk factors
- Inherited disease patterns
This helps identify any conditions that could affect pregnancy outcomes.
Step 7: Lifestyle & Health Behavior Assessment
Medical teams evaluate lifestyle factors such as:
- Smoking or vaping
- Alcohol use
- Drug use
- Nutrition and exercise habits
Surrogates must commit to pregnancy-safe behaviors throughout the journey.
Step 8: IVF Clinic Medical Clearance
Final approval typically comes from a licensed IVF clinic.
The clinic confirms:
- Medical suitability for embryo transfer
- Ability to tolerate hormonal medications
- Absence of contraindications
Without IVF clinic clearance, surrogacy cannot proceed.
Why Multiple C-Sections Matter
Most programs limit the number of prior C-sections due to:
- Increased uterine rupture risk
- Placental complications
- Surgical delivery risks
Limits vary, but many programs allow no more than two prior C-sections, depending on medical history.
Ongoing Medical Monitoring During Surrogacy
Screening does not end at approval.
Throughout the process:
- Hormone levels are monitored
- Early pregnancy ultrasounds are performed
- Prenatal care is coordinated with OB-GYNs
Ongoing monitoring allows early intervention if issues arise.
Common Medical Disqualifiers
A surrogate may be medically disqualified due to:
- High-risk pregnancy history
- Uncontrolled chronic illness
- Multiple pregnancy losses
- Structural uterine abnormalities
- Inability to safely carry a pregnancy
Disqualification protects health—it is not a judgment.
How Medical Screening Protects Intended Parents
For intended parents, thorough screening:
- Increases chance of successful pregnancy
- Reduces risk of cycle cancellation
- Protects financial investment
- Supports emotional confidence
It is one of the strongest predictors of a positive outcome.
Ethical Standards & Medical Oversight
Ethical surrogacy programs follow:
- Evidence-based medical guidelines
- Licensed physician oversight
- Transparent screening protocols
Medical screening is not optional—it is a safeguard.
Frequently Asked Questions (FAQs)
Q. Why must a surrogate have had a prior pregnancy?
Ans : Because past healthy pregnancy is a strong predictor of future success.
Q. Can a surrogate have medical conditions?
Ans : Minor, well-controlled conditions may be acceptable; uncontrolled conditions are not.
Q. Are tests repeated later?
Ans : Yes. Infectious disease testing is often repeated before embryo transfer.
Q. Does BMI matter?
Ans : Yes. Extreme BMI levels increase pregnancy risk.
Q. Can a surrogate fail screening after approval?
Ans : Yes. New medical findings can pause or stop the process.
Q. Who performs the medical screening?
Ans : Licensed physicians and IVF clinics.
Q. Is genetic testing mandatory?
Ans : Family health history review is standard; genetic testing may vary.
Q. Do lifestyle habits affect approval?
Ans : Yes. Smoking, drug use, or unsafe habits are disqualifying.
Q. Are mental health evaluations part of medical screening?
Ans : They are conducted separately but are equally required.
Q. Can international surrogates be screened in the U.S.?
Ans : Medical screening must meet U.S. clinic standards.
Q. Is screening painful?
Ans : Most tests are routine and minimally invasive.
Q. Why is screening so strict?
Ans : To ensure safety, ethics, and healthy outcomes.
Final Thoughts
Medical screening standards for surrogates exist to protect human health, ethical integrity, and family outcomes. These protocols are based on decades of reproductive medicine research and clinical experience.
For intended parents, understanding these standards provides reassurance that surrogacy is not guesswork—it is a carefully managed medical process.

Dr. Kulsoom Baloch
Dr. Kulsoom Baloch is a dedicated donor coordinator at Egg Donors, leveraging her extensive background in medicine and public health. She holds an MBBS from Ziauddin University, Pakistan, and an MPH from Hofstra University, New York. With three years of clinical experience at prominent hospitals in Karachi, Pakistan, Dr. Baloch has honed her skills in patient care and medical research.