Key Takeaways
- Chemotherapy can temporarily—or sometimes permanently—impact sperm count, motility, morphology, and DNA integrity.
- DNA fragmentation tests are essential after cancer treatment because semen analysis alone may miss deeper sperm damage.
- Recovery timelines are highly individual: some men rebound in 12–24 months, while others need medical support or assisted reproduction.
- ICSI with tested sperm, sperm selection technologies, or prior sperm banking are viable pathways.
- A structured plan (testing → recovery → interventions → treatment) helps couples move forward with clarity.
Male fertility after chemotherapy is one of the most misunderstood areas in reproductive medicine. While many men regain fertility naturally, others face lingering issues—especially high sperm DNA fragmentation, a silent driver of failed conception, miscarriages, or poor embryo development.
This article explains what to expect, what to test, and how to plan effectively for natural conception, IVF, ICSI, or surrogacy after cancer treatment.
How Chemotherapy Affects Sperm
Chemotherapy targets fast-dividing cells—unfortunately, sperm-producing cells fall into that category. Common effects include:
1. Lower Sperm Quantity
- Reduced sperm count or azoospermia
- Often temporary but depends on drug type and dosage
2. Poor Sperm Quality
- Lower motility
- Higher abnormal forms
- Slower recovery immediately after treatment
3. DNA Fragmentation
This is the key concern after chemo.
Even with normal sperm count, the genetic integrity of sperm may remain compromised for months or years. High fragmentation affects:
- Fertilization ability
- Embryo development
- Implantation
- Miscarriage rates
DNA Fragmentation Testing — Why It Matters After Chemo
Why Semen Analysis Alone Isn’t Enough
Standard semen analysis checks:
- Count
- Motility
- Morphology
But it cannot detect DNA damage.
Post-chemo sperm may “look normal” but still carry genetic breaks. That’s why DNA fragmentation testing (SCSA, TUNEL, Comet) is the diagnostic backbone for men recovering from cancer treatment.
Planning Fertility After Chemo — A Step-by-Step Roadmap
Step 1: Baseline Tests
- Semen analysis
- DNA fragmentation test
- Hormonal profile (FSH, LH, Testosterone)
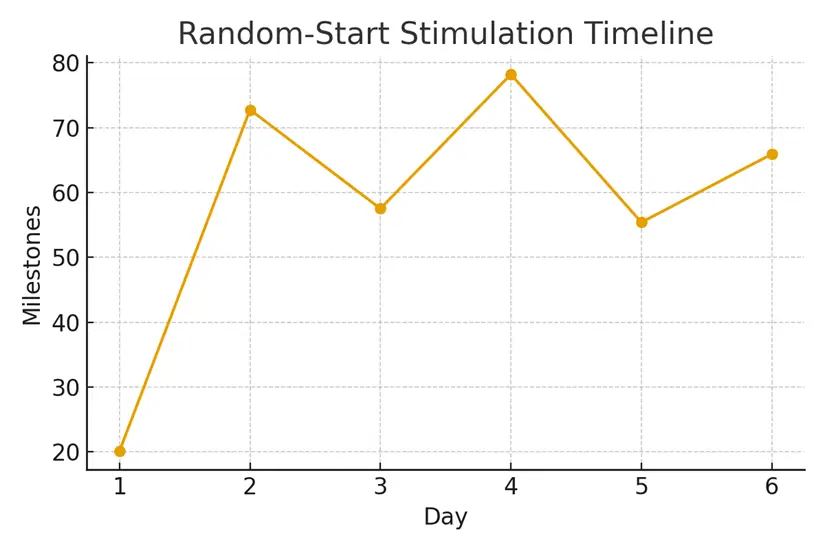
Step 2: Identify Recovery Window
Typical recovery:
- 12–24 months after chemo
- But may vary depending on age, treatment type, and baseline fertility
Step 3: Improve Sperm Quality
Interventions may include:
- Antioxidants
- Lifestyle optimization
- Varicocele correction (if present)
- Endocrine support
- Testicular sperm extraction (if ejaculated sperm have high fragmentation)
Step 4: Choose a Pathway
- Natural Conception: If counts and DNA quality normalize.
- IUI / IVF: Useful if quantity improves but fragmentation remains mild.
- ICSI With Sperm Selection (MACS / PICSI / Zymot): Used when fragmentation is moderate.
- Testicular Sperm Extraction (TESE) + ICSI: Testicular sperm often have lower fragmentation than ejaculated sperm.
- Surrogacy: Chosen when female partner’s uterine factors or medical histories require it.
Case Study — “We Planned Our Second Child After Chemo”
Background:
A 36-year-old male underwent chemotherapy for lymphoma. Two years later, the couple attempted pregnancy. Semen analysis appeared borderline-normal, but DNA fragmentation was 56%—far above the fertility threshold.
Plan Implemented:
- Antioxidants + lifestyle optimization
- Repeat test at 3 months → fragmentation reduced to 38%
- TESE performed for lower-fragmentation sperm
- ICSI with PGT-A resulted in two healthy embryos
Outcome:
A successful pregnancy on the second transfer using surrogacy due to unrelated uterine factors.
Three Testimonials
- “We were shocked when the DNA test—not the semen analysis—explained our miscarriages.”— A & M, New Delhi
- “Chemo saved my life, but I thought fatherhood was gone. The structured plan gave us a clear path.”— R.K., London
- “Using testicular sperm + ICSI worked even when ejaculated sperm looked normal but had high fragmentation.”— L & S, Toronto
Expert Quote
“Post-chemotherapy fertility isn’t about sperm count—it’s about sperm quality. DNA fragmentation is the single most important test men should undergo before planning conception.”
— Dr. Rashmi Gulati
Related Links
- Sperm Banking — Urgent Steps for Men
- Egg vs Embryo Freezing — Decision Framework
- Pre‑Chemo Testing — AMH, AFC, and Baseline Labs
Glossary
DNA Fragmentation: Breaks in the genetic material inside sperm.
TESE: Testicular sperm extraction for use in ICSI.
ICSI: Injecting a single sperm into an egg.
PGT-A: Genetic testing on embryos.
Azoospermia: No sperm in ejaculate.
Motility: How well sperm move.
Morphology: Sperm shape and structure.
FAQ
Q. How long after chemotherapy should a man wait before trying to conceive?
Ans. Most guidelines recommend 12–24 months to allow sperm production to recover and reduce mutation risk. However, individual timelines vary. Testing (semen + DNA fragmentation) provides personalized clarity.
Q. Does chemotherapy always cause permanent infertility?
Ans. No. Many men regain normal sperm function, but it depends on age, treatment dose, baseline fertility, and cancer type. Permanent infertility occurs in some cases—especially after alkylating agents or testicular cancer treatment.
Q. Can sperm count look normal but DNA fragmentation still be high?
Ans. Yes, this is common after chemo. Semen analysis cannot detect DNA damage. Only specific tests can.
Q. What is a safe DNA fragmentation level for fertility?
Ans. Under 25% is considered good; 25–40% is borderline; above 40% significantly reduces fertility success and increases miscarriage risk.
Q. Can DNA fragmentation be improved naturally?
Ans. Often yes—via antioxidants, reduced heat exposure, smoking cessation, weight optimization, and endocrine support. Improvement may take 3–6 months.
Q. Is TESE better than ejaculated sperm after chemo?
Ans. In some men with high fragmentation, testicular sperm have lower DNA damage. TESE + ICSI is frequently recommended when fragmentation remains persistently high.
Q. Is PGT-A recommended when using sperm after chemotherapy?
Ans. PGT-A can help identify chromosomally normal embryos, especially when sperm DNA damage is a concern, though it’s not mandatory in all cases.
Q. What if sperm banking wasn’t done before chemotherapy?
Ans. You can still pursue natural conception, IVF, ICSI, or TESE. Modern fertility programs can work with post-chemo samples safely with proper testing.
Q. Should men repeat testing after recovery?
Ans. Yes. Sperm parameters change every 74 days, so retesting every 3 months helps track improvements.
Q. Can surrogacy help in male factor infertility after chemo?
Ans. Surrogacy helps when the female partner cannot carry or when repeated IVF failures occur for unrelated reasons. The male factor alone doesn’t require surrogacy unless embryos must be transferred elsewhere.
Q. What lifestyle steps help after chemo?
Ans. Antioxidants (CoQ10, Vitamin C, Vitamin E), sleep regulation, low alcohol intake, stress reduction, and avoiding heat sources (saunas, laptops) can help lower fragmentation.
Q. Does age make recovery harder?
Ans. Yes. Men over 40 tend to recover more slowly and may have higher baseline fragmentation. However, successful outcomes are still possible with proper planning.

Dr. Kulsoom Baloch
Dr. Kulsoom Baloch is a dedicated donor coordinator at Egg Donors, leveraging her extensive background in medicine and public health. She holds an MBBS from Ziauddin University, Pakistan, and an MPH from Hofstra University, New York. With three years of clinical experience at prominent hospitals in Karachi, Pakistan, Dr. Baloch has honed her skills in patient care and medical research.





