Key Takeaways
- IUI success over 40 is typically under 5% per cycle, even with medications.
- Egg quality — not uterine environment — is the main limiting factor.
- IUI may still be reasonable for unexplained infertility, mild male factor, or if budget is very limited.
- Most patients over 40 save time and money by moving directly to IVF, especially with ICSI and PGT-A.
- Donor eggs or donor embryos drastically improve success rates and reduce time to pregnancy.
- Choosing the right path requires AMH, AFC, FSH, and sometimes antral follicle response under stimulation.
By the time someone reaches 40, fertility is still possible — but the biology of egg quality shifts sharply. Many intended parents wonder whether they should “start with IUI” because it’s simpler, cheaper, and less invasive. But success rates over 40 tell a different story.
This article breaks down when IUI may still be worth trying, how to interpret your lab values, and when shifting to IVF or donor options saves emotional bandwidth, time, and money. The goal: matching the treatment to the outcome you want, not prolonging a path that rarely works.
The Biological Reality — Egg Quality Drives Success
After 40, the percentage of chromosomally normal eggs drops fast.
This impacts:
- Fertilization potential
- Embryo development
- Implantation
- Miscarriage risk
IUI does not improve egg quality. It only improves sperm delivery.
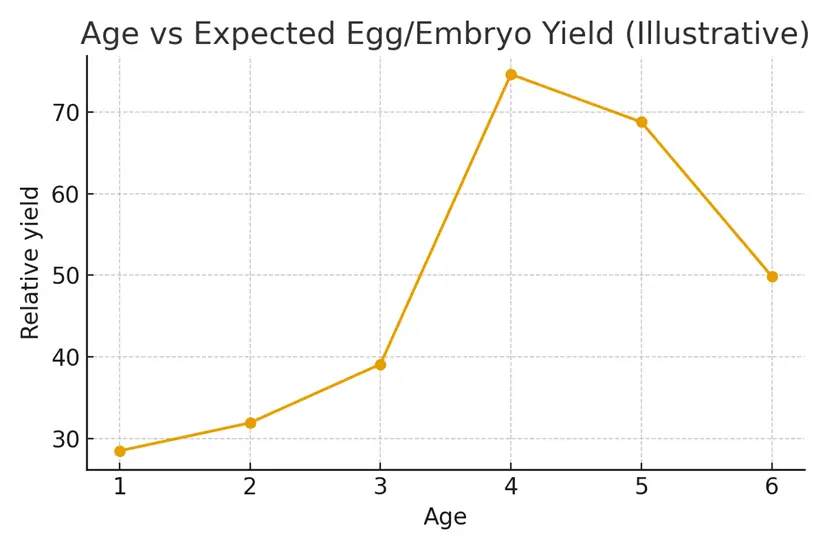
Average success rate over 40:
- Age 40–41: 4–5% per cycle
- Age 42–43: 1–2% per cycle
- 44+: <1% per cycle
(These numbers include medicated IUI cycles.)
When IUI May Still Be Reasonable
If You Have Good Ovarian Reserve for Age
- AMH > 1.0
- AFC ≥ 8
- Regular cycles
When Budget Only Allows Low-Intervention Treatment
If IVF isn’t financially possible right now, a 1–2 cycle IUI trial may provide peace of mind before escalating.
Mild Male Factor or Unexplained Infertility
IUI can bypass cervical mucus issues and timing challenges.
When IVF Is Clearly the Better Path
IVF Provides More Control for 40+
IVF helps by:
- Collecting multiple eggs at once
- Using ICSI to optimize fertilization
- Allowing embryo culture
- Offering PGT-A to reduce miscarriage and repeated failed transfers
Success rates for IVF at 40–42 are often 15–25% per transfer, and higher if multiple embryos are created.
Indicators to Skip IUI Entirely
Low Ovarian Reserve
- AMH < 0.7
- AFC < 6
- FSH > 12
IUI rarely works with low egg supply.
Trying for >6 months over age 40
Time becomes the most valuable variable.
Needing Donor Eggs Soon
If egg quality has already dramatically declined, going straight to donor eggs avoids repeated failed cycles.
Better Paths After 40
IVF With or Without PGT-A
Useful when:
- You want your own genetic connection
- You can produce at least 4–6 eggs per retrieval
- Miscarriage risk is a concern
Donor Eggs
The single most effective option.
Success rates per transfer can reach 60–70%.
Donor Embryos
Ideal for:
- Severe male + female factor
- Recurrent failed IVF
- Budget considerations
Surrogacy
Useful if:
- Repeated implantation failures occurred
- Uterine factors are present
(This is rare for women over 40 — usually the egg, not the uterus, is the issue.)
Case Study — “Two IUI Cycles, Then a Strategic Pivot”
Patient: 41 years old, unexplained infertility
Labs: AMH 1.3, AFC 9, partner healthy
Plan: Patient wanted to try “just a couple” of IUIs first.
Outcome:
- Cycle 1: No pregnancy
- Cycle 2: Biochemical loss
- Shifted to IVF with PGT-A
- Retrieved 10 eggs → 5 embryos → 2 euploid embryos
- First transfer successful, healthy live birth
Lesson: IUI offered emotional closure; IVF achieved the outcome.
Testimonials
1. R. Mehta, 42
“I tried three IUIs before switching to IVF. I wish I had known sooner that the odds were so low. IVF gave me answers and ultimately my daughter.”
2. A. Walker, 40
“My clinic pushed IUI first, but after researching, we chose IVF immediately. It saved us time, money, and heartbreak.”
3. S. Dubois, 43
“Donor eggs were the hardest decision but the best one. I became a mom within eight months.”
Expert Quote
“After 40, the biggest predictor of success is egg quality — and IUI cannot change that. Choosing the right path early saves both time and emotional energy.”
— Dr. Elena Morado, Reproductive Endocrinologist
Related Links
- PGT‑A — Pros, Cons, and Timing Over 40
- Own Eggs vs Donor Eggs — Decision Framework
- Mini‑IVF vs Conventional — Matching Protocol to Goals
Glossary
- IUI (Intrauterine Insemination): Sperm injected into uterus during ovulation.
- IVF (In Vitro Fertilization): Eggs fertilized in lab; embryos transferred later.
- PGT-A: Embryo genetic screening for chromosomal health.
- AMH: Hormone measuring ovarian reserve.
- AFC: Antral follicle count, ultrasound measure of egg supply.
- DOR (Diminished Ovarian Reserve): Low egg supply or quality.
- Donor Embryo: Embryo created from donated sperm + egg.
FAQ
Q. Is IUI worth trying after age 40?
Ans. IUI can be worth one or two cycles if your ovarian reserve is decent (AMH > 1.0, AFC > 8) and the cause of infertility is unexplained. However, success rates remain very low — usually under 5% per cycle. For most individuals over 40, IVF offers much higher success and better use of time.
Q. Why is IUI success so low after 40?
Ans. Egg quality declines sharply with age, and IUI does nothing to improve that. The uterus generally remains receptive, but the embryos created from aging eggs are more likely to be abnormal. This is why miscarriage risk increases and implantation rates fall.
Q. How many IUI cycles should I try at 40 or 41?
Ans. Most reproductive endocrinologists recommend no more than 1–2 cycles, and only if your ovarian reserve is reasonable. Beyond that, the probability of success declines to near zero, and moving to IVF is more efficient.
Q. What are the chances of IUI working at 42 or 43?
Ans. Very low — typically 1–2% per cycle. Clinics may still offer it, but data shows limited benefit. At these ages, IVF or donor options are usually the fastest route to a successful pregnancy.
Q. Does taking fertility medications improve IUI success over 40?
Ans. Medications like letrozole or gonadotropins can increase the number of eggs released, but quality remains the limiting factor. Medicated IUI after 40 may raise success slightly (from ~2% to ~4%), but still underperforms IVF dramatically.
Q. How does IVF compare for women over 40?
Ans. IVF success varies by clinic but typically ranges from 15–25% per transfer (higher if multiple embryos are available). With PGT-A, you reduce miscarriage risk by transferring only chromosomally normal embryos. IVF allows more control, more information, and more efficient progress.
Q. Should I do PGT-A if I’m over 40?
Ans. PGT-A is often recommended because the proportion of abnormal embryos is high after 40. Screening prevents transferring embryos that would fail to implant or end in early miscarriage, shortening the timeline to a healthy pregnancy.
Q. When should I consider donor eggs?
Ans. Donor eggs become an excellent option if you:
- Produce very few eggs on stimulation
- Have repeated failed IVF cycles
- Are 43+ and want the highest success rate
Donor eggs restore age-related fertility, with success rates of 60–70%.
Q. Is donor embryo a good option over 40?
Ans. Yes. Donor embryos offer high success at a lower cost than donor eggs + sperm. They are ideal when there are combined factors or when cost and simplicity matter.
Q. Is surrogacy needed if I’m over 40?
Ans. Not usually. Most issues at this age relate to eggs, not the uterus. Surrogacy is typically recommended only if you have a known uterine issue, repeated failed transfers with good embryos, or medical conditions preventing pregnancy.
Q. Can lifestyle changes improve IUI success over 40?
Ans. Lifestyle helps overall health but cannot materially change egg quality at this age. Supplements, diet, sleep, and mild exercise support hormonal balance but don’t overcome chromosomal challenges of aging eggs.
Q. What diagnostics should I do before deciding IUI vs IVF?
Ans. You should have:
- AMH
- AFC
- FSH + Estradiol (Day 2–3)
- Semen analysis
- Tubal patency test
These help determine whether IUI is feasible or whether IVF is more appropriate.

Dr. Kulsoom Baloch
Dr. Kulsoom Baloch is a dedicated donor coordinator at Egg Donors, leveraging her extensive background in medicine and public health. She holds an MBBS from Ziauddin University, Pakistan, and an MPH from Hofstra University, New York. With three years of clinical experience at prominent hospitals in Karachi, Pakistan, Dr. Baloch has honed her skills in patient care and medical research.





