AI Smart Summary
This blog explains fetal viability, highlighting key factors like gestational age, lung development, and NICU care. It offers insights on survival chances, medical tools, and considerations for surrogacy journeys.
FAST FACTS
Fetal Viability
- What It Means: The stage when a fetus can survive outside the womb with medical support.
- Key Factors: Gestational age, birth weight, lung development, NICU care.
- Survival Chances: Vary by gestational week, from 10% at 22 weeks to 90%+ by 28 weeks.
- Important Tools: Ultrasound, Non-Stress Test (NST), Biophysical Profile (BPP).
- Legal Considerations: Viability affects legal decisions on life and abortion.
KEY FACTORS EXPLAINED
- Gestational Age: More weeks increase survival chances.
- Lung Development: Critical for breathing after birth.
- NICU Care: Essential for survival, especially for preterm babies.
- Birth Weight: Higher weight leads to better survival.
TOP QUESTIONS ANSWERED
- Can a baby survive at 23 weeks? With advanced care, survival is possible but risky.
- When is viability considered in the U.S.? Typically, at 24 weeks gestation.
- Does viability guarantee long-term health? No, survival doesn’t always mean a healthy outcome.
RECOMMENDED NEXT STEPS
- Monitor Fetal Health: Regular checks by a healthcare provider.
- Surrogacy Considerations: Track fetal viability closely during a surrogacy journey.
- Consult with Experts: Discuss medical options for premature birth and post-birth care.
Fetal viability is a critical milestone in every pregnancy. It marks the point when a fetus has developed enough to survive outside the womb, with medical support if needed. As medical technology continues to evolve, understanding fetal viability is crucial for parents, especially those on surrogacy journeys. In this blog, we’ll explore the factors that influence fetal viability, provide a week-by-week overview, and answer some common questions to guide you through this important stage.
What is Fetal Viability?
Fetal viability refers to the point during pregnancy when a fetus is capable of surviving outside the uterus, typically with medical intervention in a neonatal intensive care unit (NICU). This stage varies, depending on several factors such as organ maturity, birth weight, and the medical care available at the time of birth.
While the concept is generally associated with a specific gestational week, it is not an exact science. Instead, fetal viability week depends on the fetus’s development and the care available to support it.
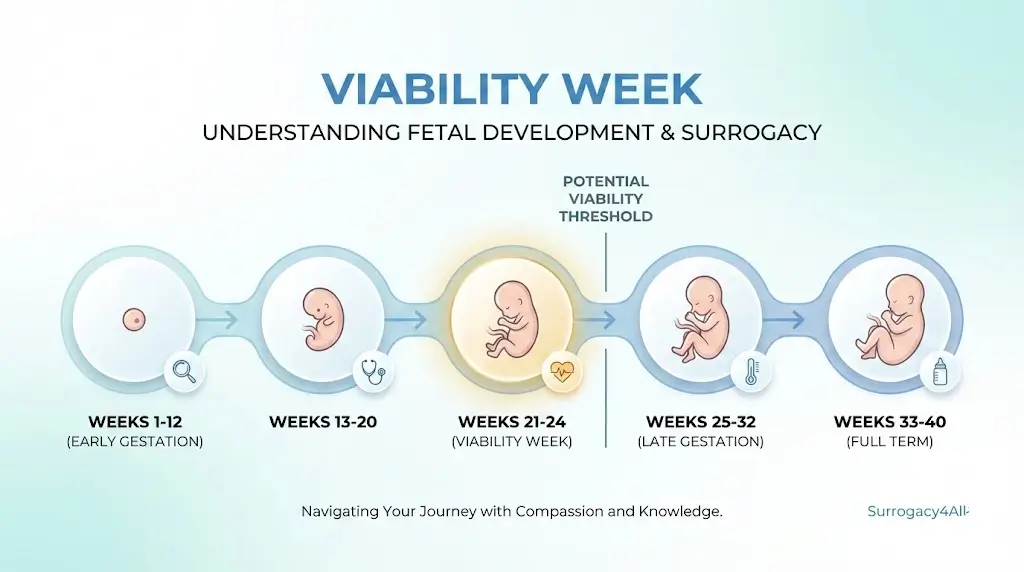
Viability by Week of Pregnancy
Before 22 Weeks:
Survival before 22 weeks is extremely rare. Babies born this early face numerous challenges, including underdeveloped organs that are crucial for survival.
22 to 23 Weeks:
This is considered the borderline for fetal viability. Survival rates at this stage range from 10% to 35%, depending on access to advanced NICU care and the baby’s condition.
24 Weeks:
By 24 weeks, survival chances improve to around 50-60%. At this stage, the fetus is more developed, but it still requires significant medical support to survive outside the womb.
25 to 26 Weeks:
At 25-26 weeks, the survival rate increases to approximately 75-80%. Babies born at this stage still face health risks but have a much better chance of survival with medical assistance.
27 Weeks and Beyond:
By 27 weeks, fetal viability is high, with more than 90% of babies surviving by 28 weeks. Organ development, particularly the lungs, plays a crucial role at this stage, improving the chances of survival without long-term complications.
Key Factors Affecting Fetal Viability
Several factors influence the likelihood that a fetus will survive outside the womb:
- Gestational Age: The most important factor in determining viability. The longer the pregnancy, the higher the chances of survival.
- Birth Weight: Higher birth weight often correlates with better survival chances. A higher weight helps with the development of vital organs and systems.
- Lung Development: Proper lung development is essential for breathing outside the womb. This is one of the last organs to mature.
- Access to NICU Care: Advanced medical care, including ventilators, incubators, and specialized staff, significantly improves survival chances for preterm babies.
Medical Tools Used to Assess Fetal Viability
Various tests and monitoring techniques are used to assess fetal health and viability:
- Ultrasound: Used to monitor fetal growth, amniotic fluid levels, and overall development.
- Non-Stress Tests (NST): This test evaluates fetal heart rate and movement, helping to assess the fetus’s well-being.
- Biophysical Profile (BPP): A combination of ultrasound and NST that provides a comprehensive evaluation of the fetus’s health.
Legal and Ethical Considerations
In some regions, the concept of fetal viability plays a role in defining life and influencing abortion laws. This is an area of complex legal and ethical considerations, especially for high-risk pregnancies. It’s important for parents and surrogates to understand the legal framework in their area, as it can impact decisions during pregnancy.
Fetal Viability in Surrogacy
In surrogacy, fetal viability is a critical factor in deciding the timing of delivery and managing complications. Surrogacy agencies and medical professionals work closely to monitor the fetus’s development and ensure the best care for both the surrogate and the baby. Surrogacy teams regularly assess fetal viability and adjust the care plan as necessary to ensure a healthy outcome.
Common Questions About Fetal Viability
Q. What factors affect fetal viability?
Ans. Gestational age, birth weight, lung development, and access to NICU care all influence a baby’s chances of survival.
Q. Can a fetus survive before 22 weeks?
Ans. Survival before 22 weeks is extremely rare, as the fetus’s organs are too underdeveloped to function outside the womb.
Q. Can a baby survive at 23 weeks?
Ans. With advanced NICU care, some babies born at 23 weeks have survived, but the risks are still very high. Survival rates are low, and many complications may arise.
Q. What is the survival rate at 24 weeks?
Ans. At 24 weeks, survival chances improve to around 50-60% with medical support.
Q. What is the age of viability in the U.S.?
Ans. In the U.S., the general medical consensus considers 24 weeks viability as the point when a fetus can survive outside the womb. However, survival at this stage depends heavily on the quality of medical care available.
Q. How do surrogacy agencies track fetal viability?
Ans. Surrogacy agencies closely monitor fetal development through medical checkups, ultrasounds, and consultations with specialists to ensure the health of both the surrogate and baby.
Q. What is the legal significance of fetal viability?
Ans. In some regions, fetal viability influences abortion laws, as it marks the point when a fetus can survive outside the womb.
Q. Does viability mean the baby will be healthy?
Ans. Not always. While the chances of survival increase as gestational age progresses, long-term health outcomes can vary. Babies born prematurely may face developmental delays or lifelong health challenges, depending on when they are born and the support they receive.
Conclusion
Fetal viability is not a fixed point, but an evolving concept influenced by advancements in medical care and individual circumstances. Knowing when a fetus is considered viable can help parents navigate high-risk pregnancies and make informed decisions about their care.
At Surrogacy4All, we understand the importance of tracking fetal development throughout a surrogacy journey. Our expert team is here to provide support to intended parents and surrogates, ensuring that both the pregnancy and delivery are managed with the utmost care. For more information, reach out to us at (212) 661-7673. Let us guide you through every step of the surrogacy process.

Dr. Veera Saghar
As an Egg Donor Coordinator, she plays a critical role in our company. Her background as a medical graduate from ISRA UNIVERSITY in Pakistan provides us with a solid foundation in the medical sciences. She has seven years of clinical experience practicing in the USA. This has given her firsthand experience when collaborating with patients and their families.
She is responsible for managing the process of egg donation from start to finish. We identify and screen potential egg donors.