Key Takeaways
- Endometriosis is strongly influenced by chronic inflammation, estrogen dominance, and immune dysregulation.
- Nutrition can significantly reduce inflammation and pelvic pain, supporting better cycle health and fertility.
- Anti-inflammatory foods like leafy greens, omega-3-rich fish, and berries help lower prostaglandins—the chemicals responsible for pain.
- Avoiding processed foods, sugars, and inflammatory oils reduces flare-ups.
- Small, consistent dietary shifts can create measurable improvements in energy, pain levels, and overall hormonal balance.
Endometriosis is more than a painful period—it is a chronic inflammatory condition where tissue similar to the uterine lining grows outside the uterus, leading to pelvic pain, bloating, fatigue, and fertility challenges. While medications and surgery are often part of the care pathway, research shows that nutrition plays a powerful role in reducing inflammation and supporting hormonal balance.
This blog explores inflammation-aware eating that can help reduce pain, improve gut health, and create a more supportive environment for fertility and overall wellness.
Understanding Endometriosis and Inflammation
Endometriosis triggers the immune system to respond as if the body is under attack. This leads to:
- Increased production of inflammatory cytokines
- Higher estrogen activity
- Elevated prostaglandins that worsen menstrual pain
- Gut inflammation that contributes to bloating and digestive issues
Anti-inflammatory nutrition reduces this cycle by lowering inflammation at the cellular level.
Inflammation-Aware Nutrition Principles
1. Prioritize Omega-3 Fatty Acids
Omega-3s help lower inflammation and reduce prostaglandins.
Best sources: salmon, sardines, walnuts, flaxseeds, chia seeds.
2. Eat More Antioxidant-Rich Foods
Antioxidants reduce oxidative stress, which worsens endometriosis symptoms.
Best choices: blueberries, spinach, kale, turmeric, ginger, broccoli.
3. Choose Low-Inflammation Proteins
Instead of red meat (linked to inflammation), choose lean or plant-based proteins:
- Lentils, chickpeas
- Tofu and tempeh
- Eggs
- Fish and chicken
4. Support Gut Health
The gut microbiome regulates estrogen and inflammation.
Add: fermented foods, fiber-rich vegetables, whole grains.
5. Reduce Estrogen-Increasing Foods
Avoid excessive soy isolates, processed meats, and alcohol.
Balance is key—not elimination.
Best Foods for Endometriosis
- Leafy greens
- Turmeric (curcumin)
- Ginger
- Berries
- Avocado
- Extra virgin olive oil
- Fatty fish
- Nuts and seeds
- Cruciferous vegetables (broccoli, cauliflower, cabbage)
Foods That May Trigger Endometriosis Flares
- Refined sugars
- Red meat
- Inflammatory oils (canola, vegetable, soybean oil)
- Dairy (for some women)
- Gluten (for gluten-sensitive individuals)
- Alcohol
- Processed snacks
Simple Daily Food Swaps
| Instead of… | Try… |
|---|---|
| White bread | Sprouted grain bread |
| Red meat | Salmon or lentils |
| Cheese snacks | Nuts + berries |
| Refined oil | Extra virgin olive oil |
| Sugary drinks | Lemon water or herbal tea |
Case Study: How Ayesha Reduced Pain & Improved Energy in 6 Weeks
Background:
Ayesha, 32, struggled with severe period pain, bloating, and fatigue. She had been diagnosed with stage II endometriosis.
Nutrition plan:
- Replaced red meat with omega-3-rich fish
- Added greens twice daily
- Removed dairy and reduced gluten
- Introduced turmeric + ginger tea
- Increased fiber intake for estrogen detoxification
Results after 6 weeks:
- 40% decrease in menstrual pain
- Less bloating
- More consistent energy
- Improved digestion
- Better mood and sleep
Ayesha’s outcomes improved further with stress reduction and physical therapy.
Testimonials
Nandita, 29
“The anti-inflammatory diet changed everything. I feel lighter, calmer, and my painful days have reduced dramatically.”
Karen, 35
“I didn’t realize how much food affected my symptoms. Within two months, my pain was nearly cut in half.”
Elena, 31
“I followed the plan and finally felt relief after years of trying medication alone. My digestion also improved greatly.”
Expert Quote
“Nutrition is one of the most underused tools for endometriosis management. When inflammation decreases, pain and hormone symptoms naturally improve.”
— Dr. Rashmi Gulati
Resource Links
- Endometriosis & Fertility Guide
- Hormone Balance Nutrition Hub
- Understanding Chronic Inflammation
- IVF Options for Endometriosis
Glossary
Estrogen Dominance
A condition where estrogen is high relative to progesterone, worsening endometriosis symptoms.
Prostaglandins
Hormone-like chemicals that cause uterine contractions and pain.
Omega-3 Fatty Acids
Healthy fats that reduce inflammation.
Cytokines
Proteins released by the immune system that promote inflammation.
Oxidative Stress
Cell damage caused by free radicals.
FAQ (10–12 Questions with Long Answers)
Q. Can diet really reduce endometriosis pain?
Ans : Yes. Diet plays a major role in inflammation, hormone balance, and immune response. Anti-inflammatory foods help reduce prostaglandins and cytokines responsible for pelvic pain. While diet isn’t a cure, it is one of the most effective complementary tools.
Q. What’s the best diet for endometriosis?
Ans : The most evidence-supported approach is an anti-inflammatory, whole-foods-based diet rich in omega-3s, antioxidants, and fiber. Many women benefit from reducing red meat, processed foods, dairy, and gluten.
Q. Should I avoid all dairy?
Ans : Not necessarily. Some women are sensitive to the inflammatory proteins in dairy. A trial elimination for 3–4 weeks can help determine if it triggers symptoms. Choose low-lactose or fermented options if tolerated.
Q. Is gluten bad for endometriosis?
Ans : Many women with endometriosis experience symptom relief when reducing or removing gluten, especially if they have gut issues. This is due to lower inflammation and improved digestion.
Q. Can I eat soy if I have endometriosis?
Ans : Whole-food soy (tofu, tempeh, edamame) is generally safe. Avoid processed soy isolates found in packaged foods and protein bars, as they can influence estrogen metabolism.
Q. Does sugar make endometriosis worse?
Ans : Yes. Sugar increases inflammation, contributes to insulin resistance, and worsens hormonal imbalance. Reducing sugar often leads to noticeable symptom improvement.
Q. What is the best breakfast for endometriosis?
Ans : A protein-rich, anti-inflammatory breakfast:
- Smoothie with spinach, chia seeds, and berries
- Scrambled eggs with turmeric and greens
- Oatmeal with walnuts and flaxseed
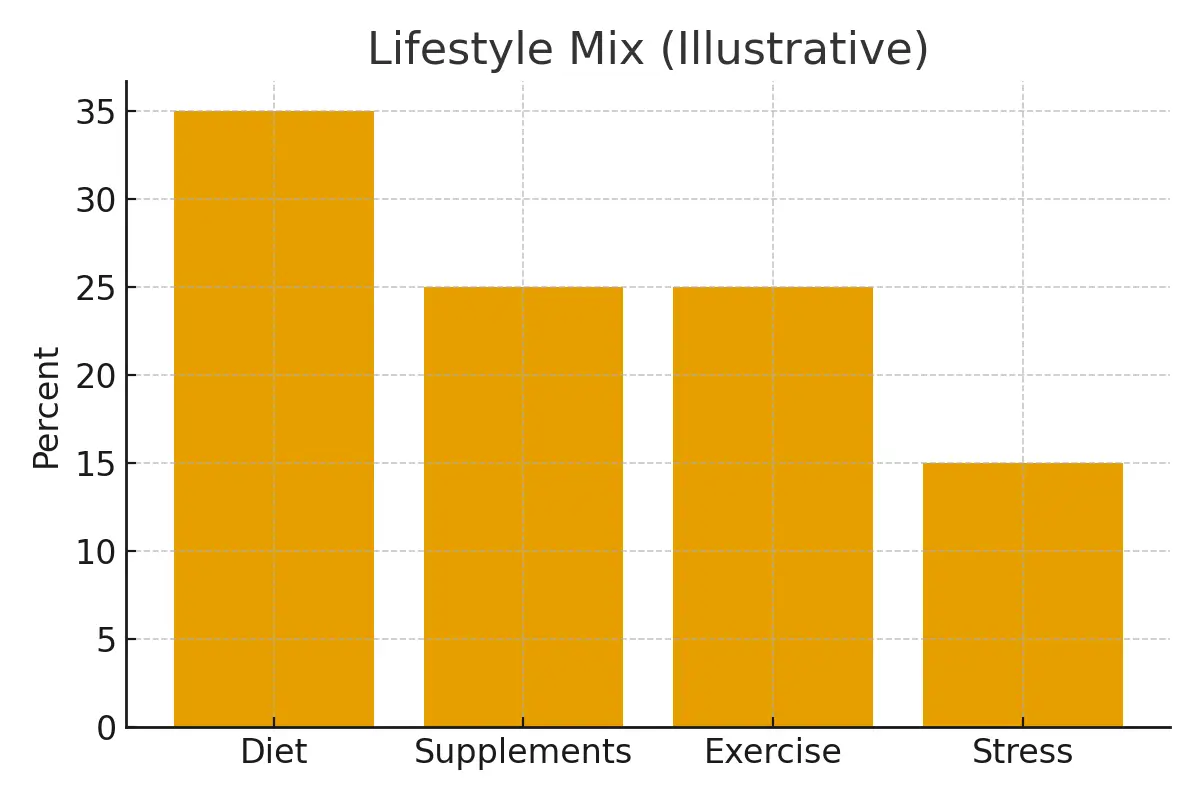
Q. Can supplements help with inflammation?
Ans : Yes. Helpful supplements include omega-3s, curcumin, magnesium, and vitamin D. They should be tailored with guidance from a clinician.
Q. Are there foods that help with fertility in endometriosis?
Ans : Yes—omega-3 fatty acids, leafy greens, antioxidant-rich fruits, and cruciferous vegetables support implantation, egg quality, and inflammation reduction.
Q. Can caffeine worsen endometriosis symptoms?
Ans : Moderate caffeine is generally safe, but excessive intake may worsen inflammation in some women. Try reducing to one cup per day.
Q. How long before I see results from dietary changes?
Ans : Most women notice improvements in pain, bloating, and energy within 4–8 weeks. Full inflammatory shifts can take 3–6 months.
Q. Is an anti-inflammatory diet safe long-term?
Ans : Yes. It is nutrient-dense, sustainable, and supports overall health, heart function, fertility, and longevity.
Q: What are the common symptoms of endometriosis?
Ans: The 20 symptoms of endometriosis include pelvic pain, heavy periods, pain during intercourse, and infertility, among others.

Dr. Kulsoom Baloch
Dr. Kulsoom Baloch is a dedicated donor coordinator at Egg Donors, leveraging her extensive background in medicine and public health. She holds an MBBS from Ziauddin University, Pakistan, and an MPH from Hofstra University, New York. With three years of clinical experience at prominent hospitals in Karachi, Pakistan, Dr. Baloch has honed her skills in patient care and medical research.





