In vitro fertilization (IVF) is a journey that blends science, timing, and personal care. One of the most common questions couples ask during their fertility journey is: “Should we go for a Day-3 or Day-5 embryo transfer?”
This decision can significantly influence outcomes, success rates, and costs. Understanding the differences between these options helps clinicians and patients make informed decisions. This article by Surrogacy4All examines the best time to choose each option, how timing is affected, and ways to simplify your plan of care without compromising results.
Understanding Day-3 vs Day-5 Embryo Transfer
What’s the Difference?
- Day-3 Transfer (Cleavage Stage): Embryos are transferred to the uterus three days after fertilization, when they usually have about 6–8 cells.
- Day-5 Transfer (Blastocyst Stage): Embryos are cultured for two additional days in the lab, allowing them to reach the blastocyst stage, containing around 100–150 cells and a fluid-filled cavity.
Where It Fits in the IVF Journey
The embryo transfer stage comes after egg retrieval and fertilization and before implantation. The timing (day-3 vs day-5) depends on embryo quality, quantity, and how your body responds to stimulation and support medications.
Who Benefits from Each Approach
Day-3 Transfer Is Often Recommended When:
- You have fewer embryos available, and extending culture to Day-5 might risk losing viable embryos.
- There’s concern about lab culture conditions or embryo arrest during extended growth.
- The clinic or patient prioritizes earlier transfer to reduce lab costs and simplify coordination.
Day-5 Transfer May Be Better When:
- You have multiple embryos showing good development on Day 3.
- You plan genetic testing (PGT-A), which requires blastocyst-stage embryos.
- Your clinic’s lab has high success rates with blastocyst culture and transfer.
- You want higher implantation potential per embryo transferred.
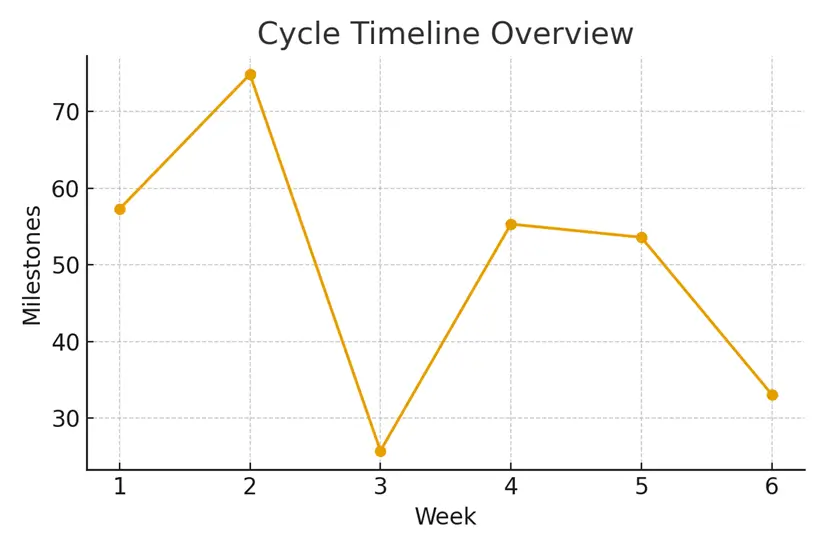
Step-by-Step Timing and Checkpoints
Ovarian Stimulation (Days 1–12):
Hormonal medications help multiple eggs mature simultaneously.
Checkpoint: Estradiol levels and follicle count confirm readiness for trigger.
Trigger and Oocyte Retrieval (Day 13–15):
A precisely timed trigger injection matures eggs for retrieval.
Checkpoint: Retrieval scheduled 36 hours after trigger for optimal maturity.
Fertilization and Embryo Development (Day 1–5):
Retrieved eggs are fertilized using IVF or ICSI methods.
Checkpoint: Embryos are assessed daily for cell division and morphology.
Transfer Decision Point (Day 3 vs Day 5):
- Day-3 transfer occurs at the cleavage stage.
- Day-5 transfer occurs at the blastocyst stage.
Checkpoint: Embryologists assess growth rate and fragmentation to decide timing.
Luteal Phase and Implantation (Post-Transfer):
Hormonal support (progesterone, estrogen) helps prepare the uterine lining.
Checkpoint: Blood tests and ultrasound confirm implantation success.
Pros and Cons: Comparing Day-3 and Day-5 Transfers
Day-3 Embryo Transfer (Cleavage Stage)
Pros:
- Earlier transfer with less lab time.
- Useful when embryo quantity is limited.
- Reduces the risk of losing embryos during extended culture.
- More predictable cycle timeline.
- Lower lab costs.
Cons:
- Limited ability to assess long-term embryo quality.
- Lower implantation rate compared to Day-5.
- Not suitable for genetic testing (PGT-A).
- May require multiple transfers to achieve success.
- Day-5 Embryo Transfer (Blastocyst Stage)
Pros:
- Embryos that reach this stage are more developmentally advanced.
- Higher implantation and pregnancy rates per transfer.
- Enables preimplantation genetic testing (PGT-A).
- Better selection — weaker embryos often self-eliminate by Day 5.
- Fewer embryos may need to be transferred to achieve success.
Cons:
- Higher lab dependency and cost.
- Risk of having no embryos survive to Day 5.
- An extended culture requires strong lab conditions and expertise.
- Slightly longer cycle, adding logistical complexity.
Understanding Costs and Practical Examples
While pricing varies by clinic, here’s a line-item example for reference (approximate ranges for New York):
- Ovarian Stimulation Medications: $3,000–$5,000
- Egg Retrieval and Lab Fees: $4,000–$7,000
- Embryo Culture (Day-3): Included in base cost
- Extended Culture to Day-5: +$1,000–$2,000
- Embryo Transfer Procedure: $1,500–$3,000
- PGT-A Testing (if applicable): $2,000–$4,000
Pro Tip: Plan your IVF in ranges—cumulative success over multiple cycles often matters more than any single round.
Outcome Drivers You Control vs. Those You Monitor
What You Can Control
- Lifestyle: Nutrition, sleep, and reduced stress support embryo quality.
- Medication Timing: Follow the prescribed schedule precisely.
- Clinic Communication: Share updates about any side effects or changes.
What You Monitor
- Embryo Development: Let your clinic guide when to transfer based on morphology and division rate.
- Hormone Levels: Estradiol, progesterone, and LH affect synchronization.
- Lab Quality Indicators: Consistent culture conditions and skilled embryologists reduce variability and improve predictability.
“Protect timing and keep plans simple—quality improves when noise goes down.” — Clinical Team, Surrogacy4All.
Real Patient Story
A Manhattan couple entered IVF, uncertain about whether to push for a Day-5 transfer. After reviewing embryo growth and lab capacity with their care team, they aligned logistics and expectations around a Day-5 blastocyst transfer.
The result? A smoother cycle with no surprise costs, clear timelines, and a successful pregnancy on the second round.
What Patients Are Saying
- “The steps finally made sense.” — A. & J., Manhattan
- “Costs were clear; no surprise bills.” — L., Hoboken
- “Nurses replied fast with practical coaching.” — K. & V., Queens
Frequently Asked Questions (FAQs)
Q: Is this medical advice?
A: No. This information is for education only. Always use it to guide deeper conversations with your fertility specialist.
Q: How many cycles should I plan for?
A: Think in ranges—cumulative success across two or three cycles often gives a clearer picture of your chances.
Q: What drives cost the most?
A: Medications, genetics, anesthesia, and the total number of cycles tend to shape the overall investment.
Expert Insights: Timing, Lab Quality & Predictability
- Oocyte retrieval often improves implantation odds by aligning lab cutoffs with natural biology.
- Luteal support enhances embryo competency by reducing variability in uterine receptivity.
- Lab quality indicators simplify cumulative success by minimizing variability in key steps.
- Trigger timing can shape predictability—when done right, it reduces cycle delays and maximizes synchronization.
Taking the Next Step with Surrogacy4All
Your IVF success depends on informed decisions, consistent timing and compassionate support.
- Free 15-minute nurse consult at (212) 661-7673
- Upload your labs for a second opinion.
- Request a personalized cost breakdown for your case.
At Surrogacy4All, we simplify complex fertility journeys with transparency, evidence-based guidance and emotional support. Every step is designed to make your path toward parenthood more predictable and humane.

Dr. Kulsoom Baloch
Dr. Kulsoom Baloch is a dedicated donor coordinator at Egg Donors, leveraging her extensive background in medicine and public health. She holds an MBBS from Ziauddin University, Pakistan, and an MPH from Hofstra University, New York. With three years of clinical experience at prominent hospitals in Karachi, Pakistan, Dr. Baloch has honed her skills in patient care and medical research.





