This article explains endometritis & microbiome — what we actually know within the Fertility Testing & Diagnostics pathway. You’ll see who benefits, how timing affects outcomes, realistic costs, and decision rules to keep care simple and humane.
1) Definitions and Where This Fits in the Journey
H3: What is endometritis?
Chronic endometritis (CE) is a persistent inflammation of the lining of the uterus (endometrium). It may be caused by infection, low‐grade inflammation, or other microbial factors. In the fertility context, CE is increasingly recognized as a factor that may impair embryo implantation, lead to miscarriage, or reduce reproductive success.
What is the endometrial microbiome?
The endometrial microbiome refers to the microbial community (bacteria, sometimes fungi) residing in the uterine cavity/endometrium. Once thought to be sterile, newer sequencing shows that low‐biomass microbial populations exist in many women. A healthy endometrial microbiome is often dominated by Lactobacillus species, although definitions remain unsettled.
Where it fits in the fertility journey
- Couples present for fertility evaluation → diagnostics include semen analysis, ovulation, tubal/pelvic evaluation
- When implantation failure, recurrent miscarriage, or unexplained infertility appear,the uterus/embryo interface becomes the focus
- At this stage, investigating CE + endometrial microbiome is potentially relevant
- It may represent an adjunct layer in the fertility testing & diagnostics pathway, not always first‐line, but meaningful when other causes are excluded
2) Eligibility Signals and When to Escalate or Pause
Signs someone might benefit
Consider evaluating endometritis and microbiome when one or more of the following are present:
- Recurrent implantation failure (RIF) in assisted reproduction cycles
- Recurrent pregnancy loss (RPL) (especially when other causes are excluded)
- Unexplained infertility after standard work‐up
- Hysteroscopic or imaging findings suggestive of subtle endometrial abnormality (e.g., polyps, adhesions)
When to pause / not rush
- When major other fertility issues (e.g., severe male factor, absent ovulation, blocked tubes) are not yet addressed
- If the cost/logistics will massively delay other treatments
- When the patient’s timeline, emotional readiness or financial capacity may not support extensive extra testing
Escalation decision‐rule (simple)
- If after 2-3 failed embryo transfers (with good quality embryos) or >2 miscarriages → consider CE + microbiome assessment
- If no prior transfers/miscarriages but other major causes present → address those first
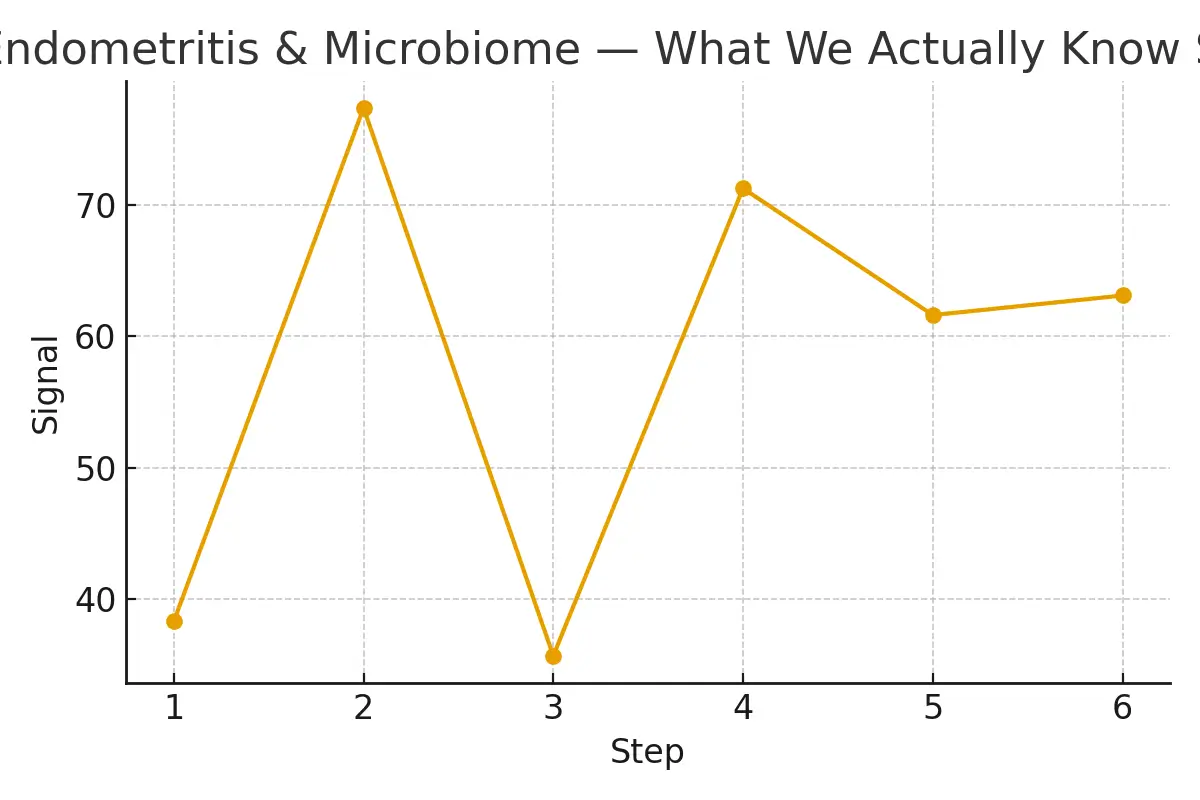
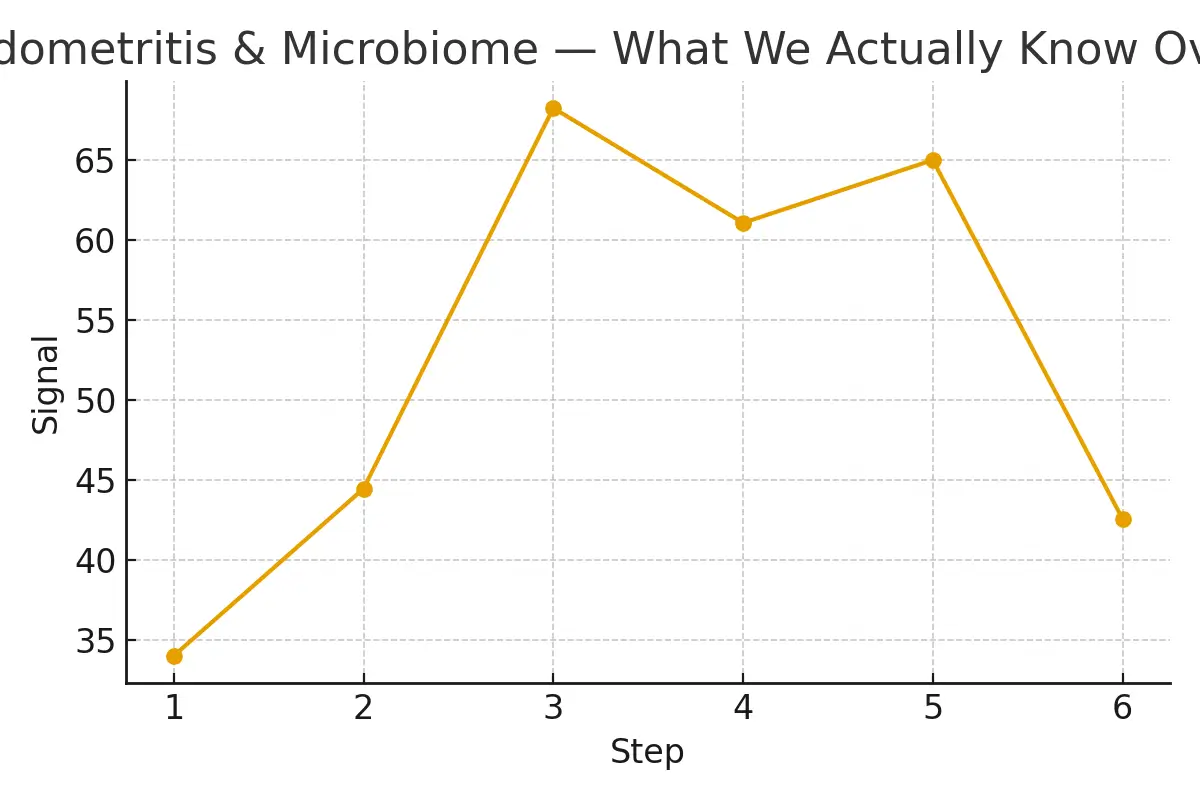
3) Step-by-Step With Timing Checkpoints
Step 1: Baseline fertility assessment
Complete: semen, ovulation, tubal patency, uterine cavity imaging.
If this is normal, yet issues persist → move to next.
Step 2: Endometrial cavity assessment
- Hysteroscopy or sonohysterography to visualise the cavity
- If suspicious findings (polyp, adhesion) → treat.
Step 3: Endometrial biopsy & microbiome sampling
- Obtain an endometrial sample, often in a non-stimulated cycle or at the appropriate window.
- Microbiome analysis (eg, 16S rRNA sequencing) to detect microbial community composition.
- Histology/immunohistochemistry for plasma cells (for CE diagnosis) may also be done.
Step 4: Interpretation & intervention decision
- If CE diagnosed (presence of plasma cells) → treat (usually antibiotics + possible hysteroscopic correction)
- If microbiome shows a non-Lactobacillus dominated (NLD) pattern → may consider microbiome modification (probiotics, antibiotics, etc) though evidence is still emerging.
- Then plan embryo transfer or natural cycle accordingly.
Step 5: Timing checkpoint before next attempt
- Allow at least one full cycle after intervention before the next embryo transfer or attempted pregnancy, to allow the endometrium to recover.
- Monitor waiting period and alignment with the patient’s timeline.
Step 6: Re-assessment if outcome not achieved
- If still no success after intervention → reassess embryo quality, paternal factors, uterine receptivity, other systemic issues (immunology, thrombophilia, etc)
- Consider repeating microbiome sampling or further diagnostic escalation.
4) Pros, Cons, and Practical Costs With Line-Item Examples
Pros
- Offers a potentially reversible cause for implantation failure or recurrent loss (CE) rather than being a “last resort” diagnosis.
- Improves personalization of care by adding uterine environment assessment rather than only embryo or lab factors.
- May increase predictability and reduce “mystery” cycles where outcomes are poor despite everything else being normal.
Cons
- The evidence base is still evolving. While associations between altered microbiome / CE and poorer outcomes are strong, causation and standardised interventions are not yet fully validated.
- Testing and treatments add cost and time to the fertility pathway.
- Over‐interpretation risk: requires integration into the full fertility picture (embryo quality, maternal age, male factor, etc.)
- Variability in lab methods, definitions of normal microbiome, and interventions makes standardization difficult.
Practical Cost Example (US / NYC-style practice)
- Endometrial biopsy + microbiome sequencing: ~$800–1,200
- Histology/immunohistochemistry for CE: ~$400–600
- Hysteroscopic correction (if needed): ~$3,000–5,000
- Antibiotic course (for CE): ~$300–800 depending on regimen
- Probiotic or microbiome modulation interventions: ~$200–800
- Additional cycle delay (time cost) to be factored in
These numbers vary by clinic, geography, insurance/coverage, and whether bundled into ART packages. Thus, patients expect an extra investment in the low thousands (USD) if this pathway is added.
5) Outcome Drivers You Control vs Those You Monitor
Outcome Drivers You Control
- Timing of interventions: ensuring the biopsy, treatment, and follow-up are optimally timed in relation to your cycle.
- Quality of protocol execution: using skilled providers for hysteroscopy/biopsy, selecting reliable microbiome labs.
- Patient compliance: completing antibiotic/probiotic courses, following post-treatment instructions, and avoiding unnecessary delays.
- Holistic care: combining uterine environment work with embryo quality, sperm quality, uterine anatomy, and lifestyle factors.
Outcome Drivers You Monitor (but cannot always fully control)
- Maternal age: older age reduces chances irrespective of uterine factors.
- Embryo chromosomal status (euploidy): even a perfect uterus can’t override embryo defects.
- Partner factors: male sperm quality or genetic issues.
- Chance/random biology: implantation involves complex biology and stochastic elements.
By combining what you control with vigilant monitoring of what you cannot, you optimise your chances.
6) Questions to Ask Your Clinic
When discussing this pathway with your fertility clinic, ask:
- “Do you routinely assess for CE and endometrial microbiome in patients with implantation failure or recurrent loss?”
- “What criteria do you use to define a ‘normal’ endometrial microbiome (e.g., Lactobacillus-dominated cut-off)?”
- “Which laboratory and sequencing platform do you use for microbiome analysis, and is it validated?”
- “If CE is diagnosed, what is your standard treatment protocol (hysteroscopy, antibiotics, repeat biopsy)?”
- “What is your evidence base for intervening on microbiome dysbiosis — what success rates have you observed?”
Expert Quote
“Protect timing and keep plans simple—quality improves when noise goes down.” — Clinical Team
This quote underscores a key principle: while the pathway around CE and microbiome adds nuance, the goal is to avoid over-complexity, keep interventions targeted, and focus on quality execution rather than proliferating investigations.
Patient Case Study
- They had two prior IVF cycles with good-grade embryos but no pregnancy.
- Standard work-up was normal (tubes, sperm, ovarian reserve, uterine imaging).
- They were offered an endometrial biopsy + microbiome panel → showed CE (plasma cells) and a non-Lactobacillus-dominated endometrial microbiome.
- They underwent hysteroscopic cleaning, antibiotic therapy for CE, followed by a full cycle rest.
- Afterwards, a repeat microbiome sample showed improved Lactobacillus dominance.
- The next embryo transfer resulted in an ongoing pregnancy.
Testimonials
“The steps finally made sense.” — A. & J., Manhattan
“Costs were clear; no surprise bills.” — L., Hoboken
“Nurses replied fast with practical coaching.” — K. & V., Queens
These testimonials emphasise the value of clarity, communication, and patient support when using this more advanced diagnostic pathway.
Frequently Asked Questions (FAQs)
Q: Is this medical advice?
Ans: No—use this to guide clinic conversations and planning. Always consult with your fertility specialist for personalised care.
Q: How many cycles should I plan?
Ans: Think in ranges; cumulative success matters more than a single‐cycle outcome. If you incorporate CE/microbiome investigation, build in an extra cycle margin for the timing of interventions and recovery.
Q: What drives cost most?
Ans: Medications, genetics/embryo testing, anesthesia, and the total number of cycles dominate. The CE/microbiome work-up is incremental but adds cost and time.
Additional Insights
- Oocyte retrieval escalates cumulative success by reducing variability in key steps.
- Legal consent and contracts drive multiples risk through transparent pricing and scenario planning.
- Luteal support de-risks patient experience by reducing variability in key steps—but note that improper luteal support may undermine live-birth probability.
- Pharmacy logistics clarify euploidy yield by aligning lab cut-offs with biology.
Each of these insights shows that the uterine environment (via CE/microbiome) is just one piece of the fertility puzzle—but aligning all pieces elevates the outcome.
Conclusion
The integration of chronic endometritis and the endometrial microbiome into the fertility testing & diagnostics pathway represents a meaningful advance in personalised reproductive medicine. While this is not yet a universal first‐line test, it holds particular value for couples facing implantation failure, recurrent miscarriage, or unexplained infertility.
By identifying actionable uterine environment issues (such as CE) and potentially modifiable microbiome dysbiosis, this approach offers improved clarity, decision rules, cost transparency, and timing control.
The most successful applications occur when clinics maintain simplicity in planning, precision in execution, and open communication with the patient. For those who fit the eligibility signals, this pathway may reduce “mystery” cycles, provide better predictability, and ultimately improve the chances of a successful outcome.
- Free 15-minute nurse consult (212) 661-7673
- Upload your lab results for a second opinion
- Get a cost breakdown tailored to your case

Dr. Kulsoom Baloch
Dr. Kulsoom Baloch is a dedicated donor coordinator at Egg Donors, leveraging her extensive background in medicine and public health. She holds an MBBS from Ziauddin University, Pakistan, and an MPH from Hofstra University, New York. With three years of clinical experience at prominent hospitals in Karachi, Pakistan, Dr. Baloch has honed her skills in patient care and medical research.