Key Takeaways
- Autoimmune disorders in men are underdiagnosed and frequently overlooked in fertility evaluations.
- Autoimmunity can impair sperm motility, morphology, mitochondrial function, and DNA integrity.
- Antisperm antibodies are rare but real — and not always clinically meaningful.
- Systemic autoimmune diseases (Hashimoto’s, psoriasis, rheumatoid arthritis, lupus) can affect sperm through inflammation rather than hormonal disruption.
- Treatments should focus on underlying inflammation, lifestyle modulation, and targeted therapies — not “immune add-ons” that lack evidence.
- Addressing male autoimmunity early improves IVF/ICSI outcomes and reduces recurrent embryo arrest.
When couples face fertility challenges, the focus often lands — almost by default — on the female partner. But male immunity plays a quieter, deeply influential role. Autoimmune disease in men can alter sperm health, increase inflammation, and create instability in embryo development.
This article outlines how male autoimmunity affects fertility, what matters clinically, what is hype, and how to manage this component proactively.
Why Autoimmunity in Men Is Frequently Missed
Women are screened more routinely for thyroid issues, antibodies, and inflammatory markers. Men rarely are — despite many having:
- undiagnosed autoimmune thyroid disease
- chronic inflammatory skin conditions
- joint inflammation
- autoimmune gut disorders
- long-standing systemic inflammatory symptoms
Because men often have fewer symptoms or ignore early signs, autoimmunity progresses quietly, impacting sperm quality over time.
How Autoimmunity Affects Sperm
Autoimmune activity influences sperm through inflammation rather than hormone disruption. Unlike women, men do not have a cyclical immune-hormone interface — but sperm production is highly sensitive to oxidative stress.
Increased Reactive Oxygen Species (ROS)
Inflammation → oxidative stress → impaired sperm function.
Mitochondrial Dysfunction
Sperm depend entirely on mitochondria for motility. Autoimmune-driven oxidative damage reduces motility and energy production.
DNA Fragmentation
When inflammation is high, DNA repair pathways falter, leading to:
- higher sperm DNA fragmentation
- poor blastocyst development
- lower implantation rates
- increased miscarriage risk
Autoimmune Conditions Common in Men
Hashimoto’s Thyroiditis
Undiagnosed in many men; affects energy, metabolism, and sperm morphology.
Psoriasis
Inflammatory skin disease associated with elevated systemic inflammation and increased oxidative stress.
Ankylosing Spondylitis & Rheumatoid Arthritis
Often treated with medications that can influence sperm, but inflammation itself is the primary concern.
Autoimmune Gut Disorders
Crohn’s, ulcerative colitis, and celiac disease are linked to poor absorption, micronutrient deficiencies, and impaired spermatogenesis.
Lupus (SLE)
Less common in men but significantly affects sperm and testosterone levels when present.
Antisperm Antibodies — Important or Overstated?
Antisperm antibodies form when the blood-testis barrier is disrupted (injury, surgery, infection).
Reality Check:
- They are rare.
- They are not always harmful.
- IVF/ICSI bypasses most issues they create.
Clinical relevance depends on antibody type, location, and concentration.
When Male Autoimmunity Becomes a Fertility Problem
Signs that matter:
- Elevated sperm DNA fragmentation (SDF > 25%)
- Recurrent embryo arrest or poor blastocyst progression
- History of recurrent pregnancy loss
- Chronic systemic inflammation
- Consistently abnormal semen analysis without lifestyle causes
When these appear alongside autoimmune symptoms, further testing is warranted.
What Tests Actually Help
Not all immune tests are helpful, but several are evidence-based.
Useful Tests
- Sperm DNA Fragmentation
- Semen ROS testing (if available)
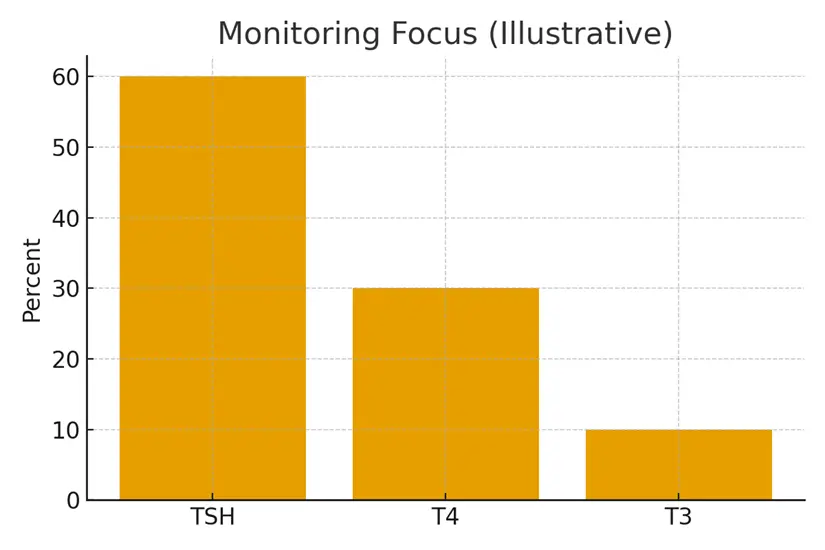
- Thyroid panel (TSH, TPO antibodies)
- hs-CRP (inflammation marker)
- Vitamin D, B12 levels
- Gut inflammation markers (case-by-case)
Common, Less Useful Tests
- Full autoimmune panels without symptoms
- “Male reproductive immunology panels” marketed online
- Cytokine assays without clear interpretation pathways
Practical Management Strategies
Anti-inflammatory Lifestyle Interventions
- Strength training + aerobic activity
- Mediterranean or anti-inflammatory diet
- Omega-3 supplementation
- Sleep stabilization
- Alcohol moderation
- Stress regulation
Medical Treatments
Depending on diagnosis:
- Levothyroxine for Hashimoto’s
- Biologics for joint autoimmune diseases
- Dermatologic therapies for psoriasis
- Gut-directed therapies for Crohn’s/UC
Fertility-Specific Additions
- Antioxidant support
- CoQ10
- NAC
- L-carnitine
- Short-term anti-inflammatory protocols (case-dependent)
Case Study: Undiagnosed Hashimoto’s in a Male Partner
Patient: 38-year-old male
Presenting issues: Two failed IVF cycles with significant embryo arrest at day 3. Normal semen parameters but high DNA fragmentation (38%).
Findings: Elevated TSH (6.2) and high TPO antibodies — previously undiagnosed Hashimoto’s.
Strategy:
- Started thyroid medication
- Added antioxidant therapy
- Reduced inflammatory load through diet and exercise
- Repeat SDF at 3 months → improved to 16%
Outcome: Next IVF cycle resulted in higher blastocyst conversion and a successful transfer.
Testimonials
1. “Nobody checked me until the third cycle.”
“I wish we knew earlier that my inflammation markers were so high. Addressing them changed our outcome.” — V.J.
2. “I never linked my thyroid levels to fertility.”
“Fixing my thyroid improved my energy and our embryo quality.” — R.M.
3. “Once inflammation was controlled, results shifted.”
“Our embryos finally reached blastocyst stage after managing my autoimmune condition.” — A.K.
Expert Quote
“Male fertility is a direct reflection of systemic inflammation. Autoimmunity doesn’t need to be severe to affect sperm — even mild inflammation can alter DNA integrity.”
— Dr. K. Sen, Andrologist & Reproductive Urologist
Related Links
- Prednisone, Heparin, and Aspirin — Where They Fit
- Immunology ‘Add‑Ons’ — Evidence vs Hype
- Miscarriage Risk and Autoimmunity — Honest Numbers
- PCOS and Thyroid Cross‑Talk — Metabolic Basics
Glossary
- Autoimmunity: When the immune system attacks the body’s own cells.
- Sperm DNA Fragmentation: A measure of DNA damage inside sperm.
- ROS (Reactive Oxygen Species): Molecules that cause oxidative stress and damage sperm.
- TPO Antibodies: Immune markers for thyroid autoimmunity.
- Blastocyst: A day 5–6 embryo ready for transfer or freezing.
- Biologics: Targeted medications for autoimmune disorders.
FAQ
Q. Can autoimmunity in men cause infertility even if semen analysis is normal?
Ans. Yes. Standard semen analysis does not measure DNA fragmentation, mitochondrial function, or oxidative stress. Autoimmune-driven inflammation often affects these deeper sperm qualities long before semen parameters appear abnormal.
Q. What autoimmune diseases most commonly affect male fertility?
Ans. Hashimoto’s, psoriasis, rheumatoid arthritis, ankylosing spondylitis, lupus, and autoimmune gut disorders. All influence sperm via inflammation, affecting motility and DNA integrity.
Q. How do antisperm antibodies form?
Ans. They typically result from testicular injury, surgery, or infection. They are rare and often overdiagnosed. Many men with antibodies still achieve pregnancies naturally or through ICSI.
Q. Can treating autoimmunity improve IVF outcomes?
Ans. Yes. Reducing systemic inflammation improves sperm DNA quality, leading to higher fertilization, better embryo development, and reduced miscarriage risk.
Q. Does thyroid disease affect male fertility?
Ans. Absolutely. Abnormal thyroid levels impair metabolic function, reduce sperm morphology, and increase oxidative stress. Treating thyroid dysfunction directly improves sperm quality.
Q. Should men with recurrent IVF failure be screened for autoimmune issues?
Ans. If embryo arrest, poor blastocyst formation, or high DNA fragmentation are present, autoimmune evaluation is reasonable. Routine blanket testing is not recommended.
Q. Do autoimmune medications harm fertility?
Ans. Some medications can affect sperm temporarily, but many are safe. Usually, inflammation itself is more harmful than the medications. Decisions should be made with a reproductive urologist.
Q. Can lifestyle changes significantly reduce inflammation?
Ans. Yes. Nutrition, sleep, exercise, weight management, and reduced alcohol intake can lower inflammation markers and improve sperm quality within 2–3 months.
Q. Does male autoimmunity increase miscarriage risk?
Ans. Indirectly. Autoimmune-driven DNA fragmentation and poor sperm integrity can contribute to embryo abnormalities that increase early miscarriage risk.
Q. Do men need immune-modulating treatments for fertility?
Ans. Not typically. Evidence does not support corticosteroids or “immune boosters” unless there is a clear autoimmune diagnosis. Most improvements come from managing inflammation and optimizing metabolic health.
Q. How long does it take to see improvement once inflammation is treated?
Ans. Sperm regenerate every 72–90 days. After treating autoimmunity or inflammation, improvements usually appear within 3 months.
Q. Should autoimmune men avoid IVF entirely?
Ans. No. IVF/ICSI can be extremely successful once inflammation is managed and sperm quality is optimized. Autoimmune disease is not a contraindication — it simply requires strategy.

Dr. Kulsoom Baloch
Dr. Kulsoom Baloch is a dedicated donor coordinator at Egg Donors, leveraging her extensive background in medicine and public health. She holds an MBBS from Ziauddin University, Pakistan, and an MPH from Hofstra University, New York. With three years of clinical experience at prominent hospitals in Karachi, Pakistan, Dr. Baloch has honed her skills in patient care and medical research.





