Key Takeaways
- APS is an autoimmune condition that increases blood-clot risk and can cause miscarriages, preeclampsia, and implantation issues.
- Diagnosis requires both clinical history and specific antibody testing performed twice, 12 weeks apart.
- Treatment often combines low-dose aspirin, heparin, and monitoring, which dramatically improves pregnancy outcomes.
- Surrogates and intended parents can succeed with APS when care is coordinated, consistent, and proactive.
- Early screening is essential for anyone with recurrent pregnancy loss or unexplained infertility.
Antiphospholipid Syndrome (APS) is one of the most overlooked causes of fertility challenges, miscarriage, and pregnancy complications. For intended parents, egg donors, and gestational surrogates, understanding APS is essential—especially because the right treatment can transform outcomes with remarkable success.
This guide breaks down what APS is, how it is diagnosed, and what care pathways help support safe, healthy pregnancies.
APS Diagnosis and Care: What You Need to Know
What Is Antiphospholipid Syndrome (APS)?
APS is an autoimmune disorder in which the body produces antiphospholipid antibodies (aPL) that mistakenly attack normal proteins in the blood. This leads to abnormal clotting, inflammation, and impaired blood flow — especially critical during pregnancy.
APS affects:
- Fertility and embryo implantation
- Placental development
- Blood flow to the uterus
- Risk of miscarriage or complications
When to Suspect APS
Clinicians consider testing when a patient has:
- Recurrent miscarriages (two or more)
- Unexplained infertility
- Preeclampsia or growth restriction
- History of blood clots (DVT/PE)
- Autoimmune diseases, especially lupus
- Early or repeated IVF failure
How APS Is Diagnosed
APS requires two components:
1. Antibody Testing
Testing must be positive twice, at least 12 weeks apart, for any of these:
- Lupus anticoagulant (LA)
- Anticardiolipin antibodies (aCL IgG/IgM)
- Beta-2 glycoprotein I antibodies (IgG/IgM)
Higher titres correlate with higher clot-risk.
2. Clinical Criteria
One or more of these events:
- Recurrent miscarriage
- One loss after 10 weeks
- Preterm birth due to placental issues
- Blood clot (venous or arterial)
APS Treatment and Care Strategy
Low-Dose Aspirin (LDA)
Reduces platelet activation and helps maintain placental blood flow.
Heparin (LMWH)
Daily injections to prevent clot formation and improve implantation.
Add-On Support Where Needed
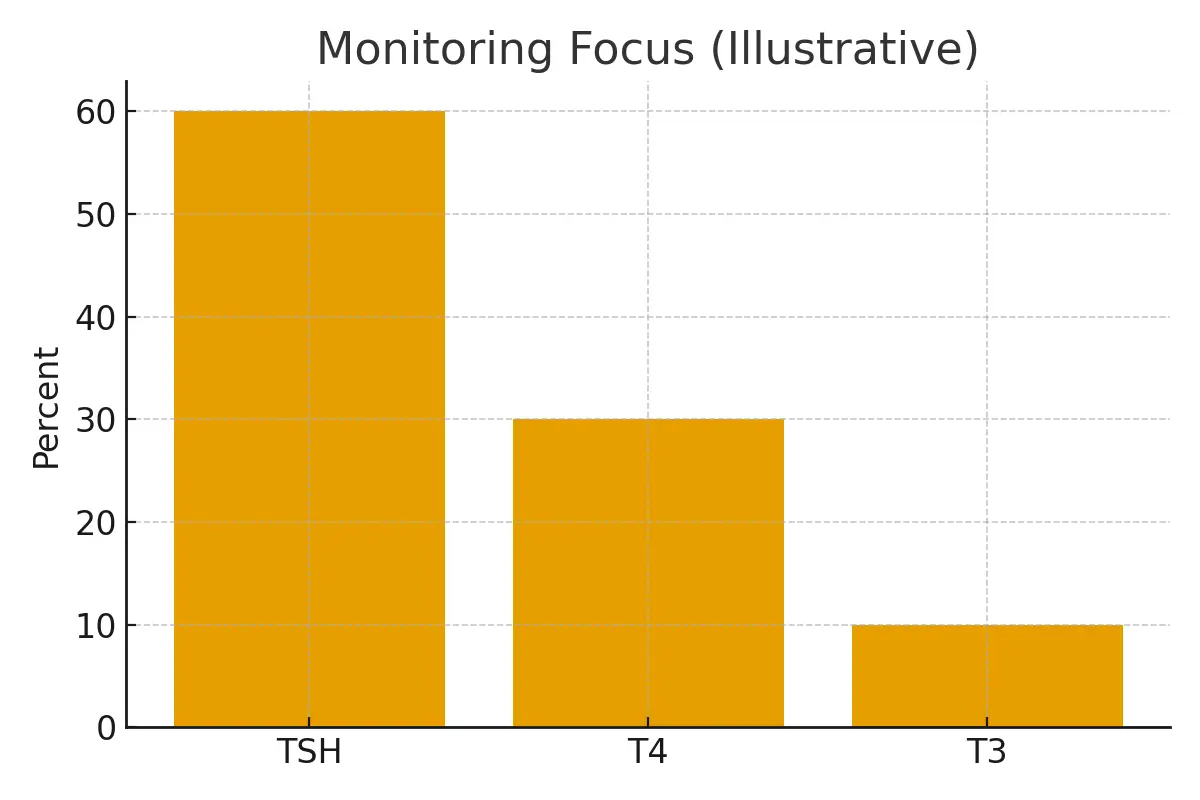
- Monitoring inflammatory markers
- Addressing thyroid antibodies
- Vitamin D optimization
- Omega-3 support
- Lifestyle modifications reducing inflammation
Pregnancy Monitoring Protocol
- Early ultrasound to confirm viability
- Monthly growth scans
- Blood pressure and preeclampsia monitoring
- Delivery planning between 37–39 weeks
Case Study: A Successful Surrogacy with APS
- Patient: Intended mother, age 34
- History: 3 miscarriages, unexplained IVF failures
- Findings: Elevated anticardiolipin IgG and beta-2 glycoprotein I antibodies
- Solution: Coordinated care plan with LDA + therapeutic LMWH + vitamin D optimization
- Surrogate: Healthy first-time surrogate screened for APS risk factors
Outcome:
- Successful embryo implantation
- Smooth pregnancy
- Healthy baby delivered at 38 weeks
This case underscores the power of early diagnosis and tailored APS care.
Testimonials
1. Sarah, Intended Parent
“After years of not knowing why IVF wasn’t working, APS testing finally gave us answers. The treatment plan changed everything.”
2. Maria, Gestational Surrogate
“The care team listened, monitored closely, and made me feel totally supported. The process was smooth and safe.”
3. Dr. H., Reproductive Endocrinologist
“I’ve seen APS treatment dramatically improve pregnancy outcomes—even in patients once considered high-risk.”
Expert Quote
“APS isn’t a barrier to parenthood. With accurate diagnosis and targeted anticoagulation therapy, most patients can achieve healthy, full-term pregnancies.”
— Dr. Kusum
Related Links
- Fertility Immunology Guide – www.surrogacy.com/fertility-immunology
- Recurrent Pregnancy Loss Hub – www.surrogacy.com/rpl
- Surrogate Medical Screening – www.surrogacy.com/surrogate-screening
- Become a Gestational Surrogate – www.surrogacy.com/become-a-surrogate
Glossary
- Antiphospholipid Antibodies (aPL): Autoantibodies that increase clotting risk.
- Lupus Anticoagulant: A type of antibody linked with thrombosis.
- LMWH: Low-molecular-weight heparin used to prevent clots.
- Placental Insufficiency: Poor blood flow to the placenta.
- Titres: Concentration levels of antibodies in blood.
FAQs
Q. Can you get pregnant with APS?
Ans : Yes. With proper treatment (usually aspirin + heparin), the majority of APS patients can conceive and carry successful pregnancies. Early monitoring is key.
Q. Does APS always cause miscarriage?
Ans : No. Many individuals with antiphospholipid antibodies never develop complications. Only high-risk profiles combined with symptoms meet APS diagnostic criteria.
Q. What is the difference between having antibodies and having APS?
Ans : You must have positive antibodies AND a clinical event (such as a miscarriage or clot) to be diagnosed with APS.
Q. Should surrogates be screened for APS?
Ans : Surrogates undergo thorough medical screening. Those with clotting disorders, autoimmune disease, or APS markers are typically not cleared due to safety risks.
Q. How early should treatment start?
Ans : Often pre-conception or immediately after a positive pregnancy test. Your clinician determines timing based on antibody levels and history.
Q. Can APS cause IVF failure?
Ans : Yes, APS can impact implantation through microclotting and inflammation. Treatment significantly improves IVF success.
Q. What are the risks during pregnancy with APS?
Ans : Potential risks include preeclampsia, growth restriction, placental insufficiency, or preterm delivery—but treatment minimizes these.
Q. Is aspirin alone enough?
Ans : For some low-risk patients, yes. Most pregnancy-related APS cases require aspirin + LMWH.
Q. Does APS go away?
Ans : No, but symptoms can be fully managed. Antibody levels may fluctuate.
Q. What lifestyle changes help APS?
Ans : Anti-inflammatory diet, movement, hydration, omega-3s, vitamin D optimization, and avoiding smoking significantly support outcomes.
Q. Is APS genetic?
Ans : Not directly, but autoimmune tendencies may cluster in families.
Q. Can intended parents with APS use a surrogate?
Ans : Yes—especially when carrying a pregnancy is medically unsafe. APS does not affect egg or sperm quality.

Dr. Kulsoom Baloch
Dr. Kulsoom Baloch is a dedicated donor coordinator at Egg Donors, leveraging her extensive background in medicine and public health. She holds an MBBS from Ziauddin University, Pakistan, and an MPH from Hofstra University, New York. With three years of clinical experience at prominent hospitals in Karachi, Pakistan, Dr. Baloch has honed her skills in patient care and medical research.





