Key Takeaways
- Subclinical thyroid disease means abnormal TSH with normal T3/T4.
- Even mild thyroid dysfunction can impact fertility, menstrual cycles, and pregnancy outcomes.
- Most experts treat subclinical hypothyroidism when TSH ≥ 4.0 (or ≥ 2.5 if TTC/IVF/surrogate).
- Subclinical hyperthyroidism rarely needs treatment unless symptoms or underlying disease is present.
- Optimizing thyroid levels before pregnancy improves implantation, reduces miscarriage risk, and supports healthy fetal development.
Thyroid health plays a major role in fertility, menstrual regulation, embryo development, and long-term pregnancy outcomes. For intended parents and potential gestational surrogates, thyroid optimization is part of standard pre-conception screening.
One area that often causes confusion is subclinical thyroid disease—a mild, often silent imbalance that may still impact reproductive success.
In this guide, we explore what it is, who should be treated, and how timing affects pregnancy outcomes.
What Is Subclinical Thyroid Disease?
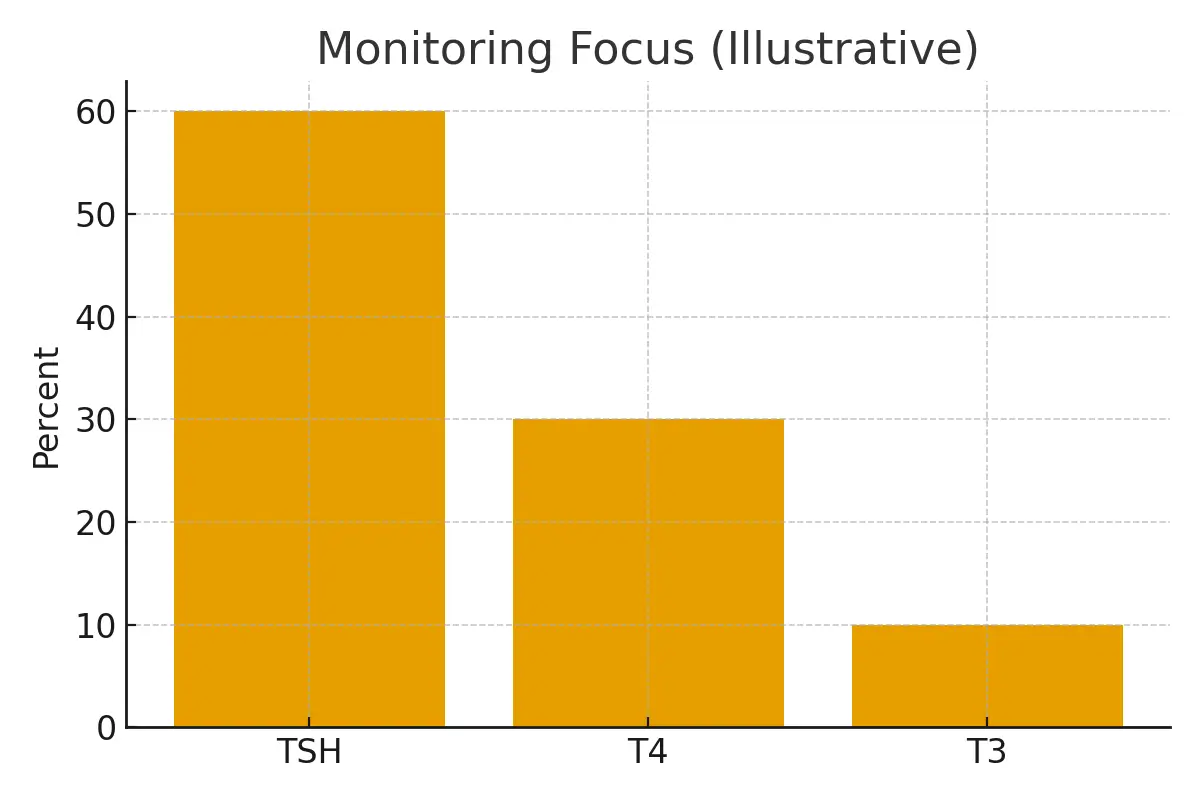
Subclinical thyroid disease occurs when TSH is abnormal, but T3 and T4 remain normal.
There are two main types:
1. Subclinical Hypothyroidism (SCH)
- High TSH
- Normal Free T4
- Often asymptomatic
- Most relevant to fertility and surrogacy screenings
2. Subclinical Hyperthyroidism
- Low TSH
- Normal Free T4 and Free T3
- Typically less concerning
- Often resolves spontaneously
Why Thyroid Function Matters for Pregnancy
Even mild thyroid dysfunction can affect the reproductive system:
Effects on Fertility
- Anovulation
- Irregular periods
- Poor egg quality
- Reduced implantation rates
- Higher miscarriage risk
Effects During Pregnancy
- Placental dysfunction
- Impaired fetal brain development (if maternal thyroid hormones too low)
- Preterm birth
- Elevated blood pressure
- Stillbirth (rare but linked to uncontrolled hypothyroidism)
This is why surrogacy programs screen thyroid levels before approval.
When to Treat Subclinical Hypothyroidism
Treatment is generally based on TSH thresholds and reproductive goals.
TSH Thresholds for Treatment
| Situation | When to Treat | Medication |
|---|---|---|
| General population | TSH ≥ 10 | Levothyroxine |
| Trying to conceive naturally | TSH ≥ 4.0 | Levothyroxine |
| IVF/Embryo Transfer | TSH ≥ 2.5 | Levothyroxine |
| Surrogate health screening | TSH ≥ 2.5 | Levothyroxine |
| Positive TPO antibodies | TSH ≥ 2.5 | Levothyroxine |
Why Treat Earlier for Surrogacy or IVF?
- Reduces miscarriage risk
- Improves implantation
- Supports early fetal development
- Stabilizes hormones before pregnancy
Most clinics aim for:
TSH between 1.0–2.5 before pregnancy
When to Treat Subclinical Hyperthyroidism
Subclinical hyperthyroidism is handled differently:
Treatment Is NOT Needed When:
- TSH is slightly low
- T3/T4 are normal
- No symptoms
- No heart issues
- No goiter
Treatment IS Needed When:
- TSH < 0.1
- Symptoms of hyperthyroidism appear
- Underlying Graves’ disease is confirmed
- Irregular heartbeat
- Bone density loss
- Severe anxiety or tremors
In pregnancy, overt hyperthyroidism requires treatment—but subclinical cases are often monitored only.
Case Study: Subclinical Hypothyroidism Before Surrogacy
Priya, age 30, applied to become a gestational surrogate. Her screening labs showed:
- TSH: 3.8
- Free T4: normal
- TPO antibodies: positive
Although she felt healthy, the clinic recommended low-dose levothyroxine to bring TSH below 2.5 before embryo transfer. Within 8 weeks, her TSH stabilized at 1.6. She had a smooth transfer and healthy delivery.
Outcome: Early treatment improved implantation rates and protected pregnancy outcomes.
Testimonials
“I didn’t know mild thyroid issues could affect pregnancy.”
“I had no symptoms but my TSH was slightly high. After treatment, I conceived within two months. This information was life-changing.”
“Surrogacy screening caught what I missed.”
“The clinic found subclinical hypothyroidism early. Treating it gave me a smooth and safe pregnancy.”
“Levothyroxine truly made a difference.”
“I felt more energetic, my cycles regulated, and my IVF cycle finally succeeded.”
Expert Quote
“For women preparing for surrogacy or IVF, optimizing even mild thyroid abnormalities improves implantation rates and reduces early pregnancy loss.”
— Dr. Rashmi Gulati
Related Links
- Understanding Thyroid & Fertility – www.surrogacy.com/thyroid-and-fertility
- Pre-Pregnancy Screening for Surrogates – www.surrogacy.com/surrogate-health-requirements
- Hormone Health Guide – www.surrogacy.com/hormone-balance
- Medication Safety in Pregnancy – www.surrogacy.com/pregnancy-medications
Glossary
- TSH (Thyroid-Stimulating Hormone): Hormone regulating thyroid function.
- Subclinical: Mild form of disease with normal hormone levels.
- Free T4/T3: Active thyroid hormones.
- TPO Antibodies: Immune markers of thyroid autoimmunity.
- Levothyroxine: Synthetic thyroid hormone used to treat hypothyroidism.
- Graves’ Disease: Autoimmune condition causing hyperthyroidism.
FAQs
Q. What is subclinical thyroid disease?
Ans : t’s a mild form of thyroid imbalance where TSH is abnormal but T3/T4 are normal. Although symptoms may be absent, it can still affect fertility, menstrual cycles, and pregnancy. Reproductive specialists take it seriously because the thyroid has direct influence on ovulation and fetal brain development.
Q. Does subclinical hypothyroidism affect fertility?
Ans : Yes. Even slightly elevated TSH can interfere with ovulation, shorten the luteal phase, and increase early miscarriage risk. Studies show that treating mild hypothyroidism improves conception rates—especially in IVF and surrogacy settings.
Q. What TSH level is ideal before pregnancy?
Ans : Most clinics aim for TSH between 1–2.5 for those trying to conceive or preparing for embryo transfer. This range supports better implantation and early embryo development.
Q. Should I treat subclinical hypothyroidism if my T4 is normal?
Ans : If you are trying to conceive, undergoing IVF, or becoming a surrogate—yes. Treatment helps stabilize thyroid levels early, reducing the risk of complications.
Q. What medication is used for treatment?
Ans : Levothyroxine, a safe and widely used synthetic thyroid hormone. It is safe during pregnancy and helps the body maintain optimal thyroid hormone levels.
Q. Do I need treatment for subclinical hyperthyroidism?
Ans : Usually not. If TSH is only mildly low and T3/T4 are normal, monitoring is enough. Treatment is only recommended if TSH is extremely low, symptoms are present, or an underlying condition like Graves’ disease is confirmed.
Q. Can untreated subclinical hypothyroidism cause miscarriage?
Ans : It increases miscarriage risk in early pregnancy, particularly when TSH is above 4.0 or when thyroid antibodies are present. Early treatment significantly reduces this risk.
Q. How often should thyroid levels be checked?
Ans : If you are trying to conceive or already pregnant, testing every 4–6 weeks is ideal. During the first trimester, the requirement for thyroid hormones increases rapidly.
Q. Can lifestyle changes improve subclinical thyroid disease?
Ans : Lifestyle changes cannot replace levothyroxine but can support thyroid function:
- Selenium-rich foods
- Stress reduction
- Adequate sleep
- Avoiding excessive iodine supplements
Q. What are symptoms of mild thyroid disease?
Ans : Many people experience none. Subtle symptoms may include fatigue, cold intolerance, weight changes, palpitations, or anxiety. However, lab testing is the only reliable way to diagnose subclinical disease.
Q. Is levothyroxine safe during surrogacy?
Ans : Yes. It is one of the safest medications used in pregnancy and is routinely prescribed to maintain ideal TSH levels for embryo transfer and fetal development.
Q. Can subclinical thyroid disease resolve by itself?
Ans : Subclinical hyperthyroidism often resolves spontaneously. Subclinical hypothyroidism tends to persist or worsen—especially when autoimmune antibodies are present.

Dr. Kulsoom Baloch
Dr. Kulsoom Baloch is a dedicated donor coordinator at Egg Donors, leveraging her extensive background in medicine and public health. She holds an MBBS from Ziauddin University, Pakistan, and an MPH from Hofstra University, New York. With three years of clinical experience at prominent hospitals in Karachi, Pakistan, Dr. Baloch has honed her skills in patient care and medical research.





